HIVAIDS/HIV the virus
HIV/AIDS
- Introduction to HIV/AIDS
- Overview of HIV/AIDS
- Health Promotion and Prevention of HIV
- HIV the virus
- AIDS and Opportunistic Infections
- Legal, Ethical, Moral Issues
- Mental Health and Spirituality
- Issues for Women and Children
- Sex workers and Intravenous Drug Users
- The face of HIV/AIDS
- Care of people with HIV/AIDS
- Community support and alternative therapies
- Critiquing literature and poster assignment
- Assessments
- Picture Gallery
HIV the Virus
Objectives
To Do
For this topic you will need to:
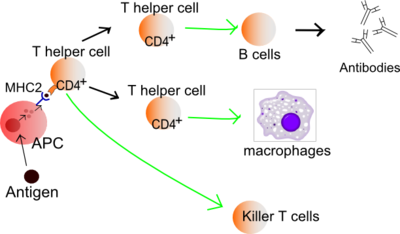
- Review the immune system particularly - the components and their functions - white blood cells (Macrophages and neutrophils, B lymphocytes, T killer lymphocytes, T helper lymphocytes), special organs - bone marrow, spleen, lymph nodes), lymph.
- Look at the module on the Immune system in the Moodle Learning Management System used in this course which has quizzes for you to test your knowledge; it is not as detailed as the Wikipedia information.
- Test yourself with the quizzes.
- View the two DVDs available at the Bill Robertson Library – 1. HIV and overview of drug therapy; 2. HIV vaccine.
- Explore the following topics which are outlined below:
- First steps in HIV infection;
- The daily cycle of HIV production and T helper lymphocyte destruction;
- The immune system kills only those HIV infected cells which it can recognise;
- From HIV infection to AIDS;
- The viral load predicts how fast the T helper lymphocyte count will fall;
- The viral load and the T helper lymphocyte count predict the risk of AIDS.
Topics
The immune system - HIV's target
For this topic you will need to refer to the letters and numbers on the diagrams. They can all be enlarged by clicking on them, or you may prefer to download printable versions - a link to a pdf file can be found below each diagram.
HIV infects cells of the immune system and AIDS is predominantly a disease due to failure of the immune system. It is not possible to understand how HIV causes AIDS and how AIDS leads to death without a basic understanding of the immune system.
HIV's structure and life cycle
Viruses are extremely small organisms, which can only multiply and reproduce themselves when they are inside the cells of some other larger organism. Most viruses can only survive for short periods outside the body of the organism they normally infect. HIV is especially adapted to infect T helper lymphocytes and can only infect a small number of other cells, for example some cells of the brain, the intestines and the skin, and another cell of the immune system – the macrophage.
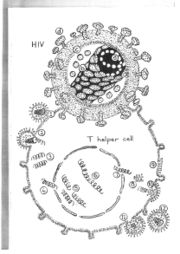
HIV is composed of its genetic code, which will be used to direct the machinery of the host cell to manufacture more HIV components, surrounded by an inner core and an outer envelope. The genetic code of HIV is contained in two long strands of RNA (a), which is very similar to the DNA in our cells. The inner core of HIV (b) is composed of proteins made within the infected cell and then assembled around the RNA . The outer envelope (c) is a small portion of the cell membrane, which wraps around the virus core as it is released from the infected cell. Some protein molecules (d) protrude from the surface of the outer envelope.
HIV uses these protein molecules to begin the process of infecting a cell. The gp120 molecule sticking out from the surface of HIV attaches firmly to a CD4 molecule present on the surface of a T helper lymphocyte or other susceptible cell (1). The outer envelope of the virus merges with the cell membrane of the T helper lymphocyte and the inner core of the virus is released into the cell (2). The virus RNA is copied into DNA (3) which is transported into the nucleus of the infected cell (4). The host cell DNA is cut, the virus DNA is inserted into the gap and the ends of the DNA are joined together (5). The genetic code instructions for making new HIV will remain in that cell until it dies (6).
Some infected cells do not immediately start making new HIV but remain inactive for months or years. When the infected cell is stimulated it neglects its normal functions and instead uses the HIV DNA as instructions (7) to produce the various components necessary to assemble new viruses. The infected cell makes new core proteins (8), new gp120 protein which is inserted into the host cell membrane (9), and a complete RNA copy of the HIV DNA. The virus RNA is then surrounded by the core proteins and buds out of the surface of the host cell taking its altered cell membrane as an outer envelope (10). After leaving the cell (11) some of the components of the virus core are split by a protease enzyme and the separate parts reorganise themselves into the structure of a mature infections virus (12). A single T helper lymphocyte infected with HIV will act as an extremely efficient factory producing thousands of new HIV to infect other cells.
First steps in HIV infection

Click on the diagram to enlarge or download a printable diagram - First steps in HIV infection.
The first cells to be infected with HIV soon after the virus enters the body, probably are macrophages (1). HIV can replicate within these cells but the amount of virus produced is not large. T helper lymphocytes are attracted to the infected macrophages by the chemicals released from the infected cells (2). While responding to the infected macrophages the T helper lymphocytes become infected by HIV released from the macrophages (3).
The T helper lymphocytes produce large amounts of HIV (4) which then infects other T helper lymphocytes, other macrophages or other cells of the macrophage family such as microglial cells in the brain, dendritic cells in the lymph nodes and spleen and similar cells in the gut and skin. These cells of the macrophage family serve as a reservoir of infection releasing virus over the coming years.
The daily cycle of HIV production and T helper lymphocyte destruction
In an HIV infected person, approximately 1 in 100 to 1 in 1000, T helper lymphocytes are infected with HIV with 1% to 0.01% of these infected cells actively producing new virus. During an average day approximately 1,000,000,000 HIV infected T helper lymphocytes produce the same number of new HIV. The T helper lymphocytes producing HIV are promptly destroyed by T killer lymphocytes. However new T helper lymphocytes become infected by the recently produced HIV and the process of virus production and T helper lymphocyte destruction continues. Most T helper lymphocytes are in the lymph nodes and the spleen and this is where almost all HIV is made and most infected lymphocytes are killed.
The immune system kills only those HIV infected cells which it can recognise
The process of copying RNA into DNA soon after HIV infects the T helper lymphocyte is a rather inaccurate one and errors are frequently made. This high mutation rate allows HIV to evolve rapidly and this evolution is thought to be a major reason why the immune system has so much difficulty controlling the infection.
A T helper lymphocyte which has been infected by HIV produces many different versions of the virus which infected the cell. These new strains of the original virus then infect other T helper lymphocytes. Some strains of the virus are recognised by the immune system, and the cells producing these strains are destroyed by T killer lymphocytes. Other new strains of HIV are not recognised by the immune system and the cells producing these strains are not killed but go on producing more HIV.
A person’s T killer lymphocytes can recognise a huge variety of different HIV strains and kill the cells producing these strains. However, HIV has an almost unlimited ability to evolve new strains. Eventually many strains of HIV which are not recognised by the immune system evolve. These strains proliferate without control and the amount of virus in the blood gradually rises.
From HIV infection to AIDS
When a person is first infected with HIV, the virus invades macrophages and T helper lymphocytes and a few other cells which also have [CD4 molecules on their surface. These infected cells produce more HIV which then infects other cells, and over the next few weeks more and more cells become infected, and the amount of virus released into the blood rapidly rises.
An antigen is ingested and processed by an Antigen Presenting Cell (APC). It presents fragments from it to T cells. The upper, Th0, is a T helper cell. The fragment is presented to it by Major Histocompatibility Complex 2 (MHC2).
About four to six weeks after becoming infected, the person’s immune system recognises that T helper lymphocytes are producing virus. Over the next few weeks T killer lymphocytes destroy more than 99% of the virus producing cells, and the amount of virus in the blood is rapidly reduced. However, the T killer lymphocytes can only recognise as infected those cells which are actively producing virus. Many infected cells are not producing virus, and escape detection to become a reservoir of HIV for the rest of the person’s life.
The destruction of so many infected cells at one time commonly causes a brief illness. The lymph nodes which contain most of the infected T helper lymphocytes become swollen and tender as the virus-producing cells are killed. Other common symptoms include exhaustion, sore throat, headache, fever, and skin rash. The illness is quite similar to glandular fever, another disease also due to a virus which infects lymphocytes. After about a week when most of the virus-producing cells have been killed the person recovers and feels perfectly well again.
Shortly after the T killer lymphocytes have started destroying HIV infected cells, B lymphocytes start making antibodies against the different parts of the virus. The antibodies coating the virus make it more difficult for HIV to invade T helper lymphocytes, and they also help other cells of the immune system to engulf and destroy the virus. B lymphocytes continue to produce large amounts of antibodies against the many components of HIV for the rest of the person’s life. When the B lymphocytes start to produce antibodies against HIV, the person is said to change from being sero-negative (antibody-negative) to sero-positive (antibody-positive). As a glandular fever-like illness occurs shortly before this change, it is often called the sero-conversion illness.
Diagnosis of HIV infection
Finding antibodies to HIV in a person’s blood is the usual method of diagnosing HIV infection. This method is used because it is simple, cheap and reliable. It can give an incorrect result (false positive) in the first month of infection when there is a lot of virus in the blood but antibodies have not yet been produced. For someone to be confirmed negative, it is necessary to be tested three months after the first test.

Two different methods of detecting antibodies can be used to diagnose HIV infection. A simple and cheap but slightly less reliable test (the screening test) is used first on all blood samples, and a more complicated, expensive and reliable test (the confirmatory test) is used to retest all those blood samples found positive on the first test.
The first test method, the ELISA test, will be positive if the blood sample contains antibodies against one or more parts of the virus. It may however also be misleadingly positive if the blood sample contains an antibody against some portion of another organism which is immunologically similar to a part of HIV. The second test method, the Western blot, will show whether there are antibodies to many different parts of HIV. There is lots of information about HIV testing. A person who is infected with HIV has antibodies to several parts of the virus. However a person who has a positive ELISA test, but who does not actually have HIV infection, will have antibodies which cross-react with one or, at most two parts of HIV. When blood samples are tested with the ELISA followed by the Western blot the results are almost 100% accurate.
Once a person has developed antibodies against HIV the infection is unable to be eradicated and will be present lifelong. However most people with HIV infection remain well for many years before developing HIV-related illnesses. During these years the amount of HIV in the blood remains relatively constant.
However the number of T helper lymphocytes in the blood gradually falls, and eventually gets so low that there are not enough T helper lymphocytes to adequately regulate the other cells of the immune system. The infected person starts to develop minor immune deficiency illnesses and gradually progresses to AIDS.
In a person without HIV infection there are usually between 400 and 1600 T helper lymphocytes in every cubic millimeter of blood. The number of T helper lymphocytes in the blood usually falls to about 500 at the time of the initial T killer lymphocyte respond four to six weeks after infection. Following this early severe fall there is usually a period of several years when the T helper lymphocyte count falls more gradually, and when it gets below 100 there is a high risk of developing an AIDS illness.
The amount of HIV in the blood also goes through dramatic changes. It rises quickly in the first few weeks after infection to reach approximately one million viruses per millilitre of plasma and then falls to a lower level as the immune system starts killing infected cells. During the following years the level of HIV in the blood remains relatively stable but it rises again shortly before the onset of AIDS.
The viral load predicts how fast the T helper lymphocyte count will fall
Measuring the amount of HIV in the blood (the viral load) is extremely useful for predicting whether the T helper lymphocyte count is likely to fall quickly or slowly over the next few years. People with untreated HIV infection usually have a viral load between 100 and 1,000,000 HIV per millilitre of plasma. The laboratory measuring the viral load usually reports the results in logarithms (or logs) because these numbers are easier to use. For example 1,000,000 is reported as 6.0, 100,000 is reported as 5.0, 10,000 is reported as 4.0, etc. Most laboratories cannot measure below a level of 50 HIV per millilitre of plasma. While a small proportion of untreated people have a viral load greater than 100,000, most have a viral load between 1,000 and 100,000, and a few have a viral load less than 1,000.
People with very large amounts of HIV in the blood tend to have a rapid, severe decline in their T helper lymphocyte count and commonly develop AIDS within a few years of becoming HIV infected. People with average levels of HIV in their blood have a gradual decline in their T lymphocyte count and usually develop AIDS about 10 years after becoming HIV infected. People with very low levels of HIV in their blood have a very slow decline in their T helper lymphocyte count and may have relatively normal health despite having had HIV infection for many years.
The viral load and the T helper lymphocyte count predict the risk of AIDS
The risk of developing AIDS in the next few years can be estimated once the blood has been tested to measure the viral load and the number of T helper lymphocytes in the blood. A person with a high viral load and a low T helper lymphocyte count has a very high chance of developing AIDS in the next few years while a person with a low viral count and high T helper lymphocyte count is extremely unlikely to develop AIDS in the next few years.

![Diagram of the HIV virus [1] [2]](/images/a/a3/114px-Niaid-hiv-virion-mod_media_commons.jpg)