User:Lanazmb
Contents
- 1 Living Well with Dementia
- 1.1 Home
- 1.2 About
- 1.3 Course
- 1.3.1 Unit 1 The Person
- 1.3.2 Unit 2 Living Well
- 1.3.3 Unit 3 The Diseases
- 1.3.4 Unit 4 Tools
- 1.4 The Team
- 1.5 Contact
Living Well with Dementia
Home
Welcome!
In this course we will be exploring how to live a full engaged, productive, and satisfied life with dementia; in your own home and community!
If you would like to earn a “Living well with dementia” completion badge you must complete the following 3 activities:
- How Person Centered am I? (Use reply box)
- Healthy Brain quiz (create an account by providing email address)
- Signs and Symptoms quiz
About
In this course, you will work through four units at your own pace:
- The Person
- Living Well with Dementia
- The Disease
- Tools
In each unit there will be readings, videos, and activities that you will be asked to participate in to enhance your understanding. At the end of each unit you will be given the opportunity to reflect on what you have learned. You are welcome to write your responses in the “Reply” box at the bottom of the page or write in a separate notebook to keep for future reference.
Activities will be indicated by
Reflections will be indicated by
Listening to audio will be indicated by![]()
Now you are ready to start, go ahead enjoy your learning journey!
Netiquette
Netiquette: Internet Etiquette
It is important to understand that this online course is public and can be viewed by anyone and everyone. Remember that you should only share information that you are willing to share with anyone and everyone! Below are a few rules to guide you as you respond to the course activities:
Be Nice
- The first rule of Internet etiquette is to be nice.
- Show respect for the opinions of others, even if you don’t agree
- Refrain from name-calling. Avoid saying anything negative about others.
Keep Messages and Posts Brief
- Short responses will hold other’s attention
Don't Shout
- Avoid using all caps in any email or post, it comes across as shouting, which is rude.
Use Discretion
- Anything you put on the Internet can be there forever. Even if you remove the material, someone may have copied or saved it.
- Rule of thumb to never post anything you wouldn’t want your parents, children, grandchildren or boss to see.
Protect Personal Information
- Avoid adding anything personal such as address, phone number, social security number, and driver’s license information.
- You don’t want to make things easy for identity thieves, burglars, and predators.
Read Before You Click "Send"
- It is always a good idea to reread anything you type before clicking the “send” button.
- Check for your spelling, grammar, and tone of the message.
Help Others
- Offer your assistance to others that may not be familiar with online learning
- Share information on proper etiquette.
Here are some tips to help you navigate this site.
Across the top of the screen you will see a task-bar that lists each section of the course.
TRY IT:
Put your cursor over the “About” section and see what happens.
Once you get the drop down in each section you can put your cursor over the content area that you want to go to and click with your mouse. This will take you directly to that content.
TRY IT:
You will also see at the bottom of each page “Next.” If you click on this with your mouse, it will take you to the next page automatically.
Throughout the course you will see videos and audio tapes to different topics. You will just need to click the triangle and the video will play.
TRY IT:
Go to “Home” page, scroll down to video and click the to play. Enjoy Judith’s and Sharon’s video!
To participate in the activities you will be asked a question and you are to write your reply in the box provided. REMEMBER: this information is public and can be viewed by everyone!
Getting to Know You
Let’s get to know a little bit about you.
Write a brief statement about yourself, why you are interested in this course.
Complete your statement in the box below at the bottom of the page. Once completed, click on the “Post Comment” button.
Course
In this course you will work through four units:
- The Person
- Living Well
- The Disease
- Tools
Course Goals:
- To demystify the fear of dementia
- Provide knowledge and tools to develop opportunities to live well with dementia through voice and choice
Outcomes of this course:
Participants in this course will:
- learn how to be engaged, participate and have voice in their jorney with dementia
- explore components of a satisfying and fufilled life
- recognize the different stages of dementia that influence the journey.
- use tools to create environments that support living well with dementia.
- enhance their understanding and sense of community.
You are now ready to start your learning journey.
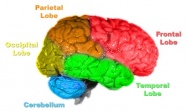
Unit 1 The Person
(Image)
Unit 1: Outcomes
Participants will:
- Explore the definition of person.
- Become familiar with person-centered approach.
- Recognize stigma and how it impacts a person’s life journey.
- Initiate their own life story.
(Image)
Person Centered
![]() Click on the link above and listen to the presentation on what it means to be person centered
Click on the link above and listen to the presentation on what it means to be person centered
 Activity: How Person Centered am I?
Activity: How Person Centered am I?
For a family and health care professional to provide meaningful person centred care they need to get to know me, my likes dislikes, wishes, dreams, etc. For example:
Even though Sharon is Scottish, she hates porridge oats, but
- she loves Blues music
- Personal grooming, especially her hair is really important
- she loves the ocean and spending time there
- she needs lots of light in her room
- she does not like over use of touch (hugs)
In the reply box below or in your notebook, list five things that a carer or health care professional would need to know about you to provide person centred care? Describe why these things are important to you.
Life Story
Lived experience: A story about me
![]() Listen to Mary’s life story. While you are listening, think about the things that would be important to know about her if you were going to provide person-centered care.
Listen to Mary’s life story. While you are listening, think about the things that would be important to know about her if you were going to provide person-centered care.
“The truth about stories is that, that is all we are”
“If we lose touch with the stories that define us and give us meaning we lose touch with who we are”
Thomas King
 Activity: Getting to Know you better.
Activity: Getting to Know you better.
In the following activity you are asked to complete the first two pages of the attached document outlining what is important for people to know about you. It is suggested that you save and print a copy so you can share it with your family when you have it completed. You are also welcome to share a blank copy with your family and friends to complete as well.
Reflection
 Now that we know what being person-centered means and the importance of getting to know the person’s life history, take a minute a jot down some of the things that you have learned in this unit.
Now that we know what being person-centered means and the importance of getting to know the person’s life history, take a minute a jot down some of the things that you have learned in this unit.
You can write in the “reply” box below or in your notebook for future reference.
Resources
Unit 2 Living Well
Unit 2: Outcomes
- Recognize systems that support people living with dementia
- Understand environmental elements/aspects that support people living with dementia
- Locate resources that can support you
- Develop strategies to stay engaged in your community
Unit 2: Part 1
Jim's Story
Jim's Story Dementia Friendly Communities
![]() Press the link above and listen to Jim talk about his journey with dementia.
Press the link above and listen to Jim talk about his journey with dementia.
Supports to Live Well
Systems that support people living with dementia
- family
- friends
- neighbours
- GP
- recreation centres
- senior centres
- AlzBC
- Handidart
- day centres
- peer support
- churches
- library's
- support groups
Environmental elements/aspects that support people living with dementia
- signage
- natural lighting
- rest areas
- colors
- noise
- familiarity
- others approach to you
Click here to access the dementia mind map
Click Full-Screen, and then click the magnifying glass to get an explanation of each support
 In the “reply” box below or in your notebook, identify the resources in your community that already exist that can support you?
In the “reply” box below or in your notebook, identify the resources in your community that already exist that can support you?
Built Environment
What is a dementia friendly community?
Dementia friendly communities have the power to change the way we think about living with dementia by enabling everyday services, environments and those within them to better engage with people affected by, or living with, dementia.
A dementia friendly community can be defined as a place or culture in which people with dementia and their carers are empowered, supported and included in society, understand their rights and recognise their full potential.
Taken from Alzheimer’s Disease International
![]() Click on the play icon to listen to this presentation.
Click on the play icon to listen to this presentation.
Built Environment for Dementia
Alternate Point of View
In the Reply box below or in your notebook write down the answers to the following questions:
- Should people living with dementia be identified as “disabled”? Why or why not?
- Would this designation increase the stigma of being diagnosed with dementia?
- Are there any benefits to this designation?
Unit 2: Part 2
Keeping Your Brain Healthy
![]() Press the link below and listen to the tips on keeping your brain healthy
Press the link below and listen to the tips on keeping your brain healthy
What Can You Do To Keep Your Brain Healthy?
 Activity: In the reply box below or in your notebook, jot down some changes that you could make to improve your brain health.
Activity: In the reply box below or in your notebook, jot down some changes that you could make to improve your brain health.
Ways that we can provide support
 Activity: click on the link below to get some helpful tips on how we can support someone to live well.
Activity: click on the link below to get some helpful tips on how we can support someone to live well.
12 Top Tips: Working with People with Dementia
Hints for Communicating
Words, Images, Procedures, and Experiences that Harm
Harmful words and images:
- Demented
- hostile
- Dysfunctional
- walking carcass
- Incoherent
- uncooperative
- Empty
- difficult
- Vegetative
- non-compliant
- Babbling
- Dependent
- Confused
- Shells
- nonhuman
Procedures and Experiences that Harm:
- Unnecessary and inappropriate assessments
- Being dismissed
- Being yelled at or scolded
- Using deception
- Not acknowledging remaining abilities
- Being treated like a child
- Being labelled
- Being excluded
- Focusing on the disease
- Being ignored
- Being made fun of, teasing or humiliating
- Being overprotected
- Being invalidated
- Being treated as an object
- Having things done to them without explanation
- Being silenced
- When people don’t listen
| Suggested Communication Strategies | Give an example of how you might use this strategy: |
| 1) Remember the basics of good communication | |
| 2) Understand the person wants to communicate with you | |
| 3) Make a good first impression | |
| 4) Create an environment that facilitates good communication | |
| 5) Treat the person as an adult | |
| 6) Respond to emotional needs | |
| 7) Remember the importance of nonverbal communication- yours and theirs | |
| 8) Remember that their behaviours communicate a message | |
| 9) Do not take the person too literally | |
| 10) Use repetition to facilitate better communication | |
| 11) Do not argue or confront | |
| 12) Speak using positive language | |
| 13) Employ humour in communication | |
| 14) Be in control of the conversation | |
| 15) Don’t take comments personally |
Give an example of how you might use each strategy listed above.
From: The Best Friends Approach to Alzheimer Care
Your Life-Story-con't
 Activity: At this point we would like you to take out the “Life Story” that you started in Unit 1 and complete pages 3 & 4. You can also click on the link below!
Activity: At this point we would like you to take out the “Life Story” that you started in Unit 1 and complete pages 3 & 4. You can also click on the link below!
Healthy Brain Quiz
 Activity: click on the link below to access a short, informative quiz about Healthy Brain:
Activity: click on the link below to access a short, informative quiz about Healthy Brain:
Reflection
 Reflection: what would you suggest needs to happen to for your community to be more dementia-friendly?
Reflection: what would you suggest needs to happen to for your community to be more dementia-friendly?
Answer in the reply box below, and then click ‘Post Comment.’
Resources
Click below to access full list of resources available:
Resources for people with dementia living at home(figure out how to put document)
Click here to access resources from Dementia Centre "Outdoor Spaces"
Article
Access article here:The Dutch Village Where Everyone Has Dementia
Engagement
Access Document:Meaningful Engagement Document
Unit 3 The Diseases
Unit 3: Outcomes
- Understand stage of Alzheimer disease and how it influences ones life journey
- Articulate the common signs and symptoms- each journey is unique
- Be familiar with Alzheimer’s disease and other related dementias
- Be aware of changes in the brain with Alzheimer disease
- Consider lifestyle and risk factors
- Recognize the importance of early diagnosis
Unit 3: Part 1
Dementia to Me
Looking for New Ways to Solve Alzheimer's
![]() What Dementia is To MefromKreativityonVimeo
What Dementia is To MefromKreativityonVimeo
Dementia
Dementia Facts
Dementia Facts: In this activity you are to read the statement and decide whether you think it is Fact or Fiction.
Write your answers in the reply box below.
| Did you Know? | Fact or Fiction? |
| 1. 564,000
Canadians are currently living with dementia |
Fact _____ Fiction______ |
| 2. 937,000
The number of Canadians who will be living with the disease in 15 years |
Fact _____ Fiction______ |
| 3. $10.4 billion
The annual cost to Canadians to care for those living with dementia |
Fact _____ Fiction______ |
| 4. $293 billion
The cost of dementia in 2040 |
Fact _____ Fiction______ |
| 5. $1000 The cost per day for elder in hospital
$ 130 The cost per day for care in facility $ 55 A day for care in the home care |
Fact _____ Fiction______ |
| 6. 45%
The greater your risk of developing dementia if you smoke |
Fact _____ Fiction______ |
| 7. 65%
Of those diagnosed with dementia over the age of 65 are women |
Fact _____ Fiction______ |
| 8. 16,000
The number of Canadians under the age of 65 living with dementia |
Fact _____ Fiction______ |
| 9. 25,000
The number of new cases of dementia diagnosed every year |
Fact _____ Fiction______ |
| 10. 56,000
The number of Canadians with dementia being cared for in hospitals even though this is not an ideal location for care |
Fact _____ Fiction______ |
| 11. 1.1 million
The number of Canadians affected directly or indirectly by the disease |
Fact _____ Fiction______ |
Taken from alzheimers.ca what is dementia
For answers, see next page:
Dementia Facts Answers
The answers are all facts!
Taken fromAbout Alzheimer
Forgetfulness: Normal or Not?
Free subscription:Alzheimer weekly
Keep your Memory Sharp
- Keep a routine
- Organize information (keep details in a calendar or day planner)
- Put items in the same spot (always put your keys in the same place by the door)
- Repeat information (repeat names when you meet people)
- Run through the alphabet in your head to help you remember a word
- Make associations (relate new information to things you already know)
- Involve your senses (if you are a visual learner, visualize an item)
- Teach others or tell them stories
- Get a full night’s sleep
- Learn more about what you can do tomaintain your brain healthand strengthen your memory
Normal aging vs dementia
Normal aging vs dementia
ALZHEIMER’S DISEASE AND OTHER DEMENTIAS ARE NOT A PART OF NORMAL AGING.
Almost 40 per cent of people over the age of 65 experience some form of memory loss. When there is no underlying medical condition causing this memory loss, it is known as “age-associated memory impairment,” which is considered a part of the normal aging process.
In the reply box below make a list of some of the memory issues that you may be experiencing
Look at the list provided in previous page and see if the issue is normal aging or signs of something else.
If you have any concerns about you list, make an appointment with your Dr. to discuss
Activity: SAGE Test
 In this activity, you can complete an early diagnosis test.
In this activity, you can complete an early diagnosis test.
First of all, read the terms and conditions, you can download the test.
Once you have completed it, share the results with your family doctor to help you interpret the results.
NOTE: THIS TEST DOES NOT REPLACE MEDICAL ADVISE.
Download here:SAGE Test
3D's
- Speed of onset
- Delirium
- Acute/fast
- Depression
- Slow but can be triggered by life events
- Dementia
- Slow
- Delirium
- Signs and Symptoms
- Delirium
- Inattention
- Hyperactive/hypoactive
- Worse at night and early morning
- Symptoms fluctuate
- Perception distorted have delusions and hallucinations
- Easily distracted
- Lethargic or
- hyper vigilant
- Depression
- Sadness
- Feeling blue
- Loss of interest and pleasure
- Lack of self care
- Decrease in appetite
- withdrawal
- Dementia
- Memory loss
- Gradual impairment of ADL skills, communication,
- Change in behaviour
- Slow steady decline
- Often worse in the morning
- Delirium
- Treatment
- Delirium
- Treat the cause
- Provide environmental support
- Can resolve in hours to one month
- Depression
- Anti-depressants
- Cognitive therapy
- Dementia
- Medication in early stages can slow progress in some people
- Irreversible no treatment
- Delirium
- Prognosis
- Delirium
- Good if treated early
- Depression
- Usually mood can be improved
- Dementia
- Gradual worsening of condition until death
- Delirium
Adapted from: 3D's
Unit 3: Part 2
What is Alzheimer's?
To view video, click red start button, and then click the box in the lower right corner of the video to view full-screen.
Understand Alzheimer's Disease in 3 Minutes
Alzheimer's and Other Dementia
WHAT IS ALZHEIMER'S DISEASE?
“Alzheimer’s disease is a disease of the brain where abnormal proteins collect in brain cells. Alzheimer’s disease causes symptoms of dementia such as memory loss, difficulty performing daily activities, and changes in judgement, reasoning, behaviour, and emotions. These dementia symptoms are irreversible, which means that any loss of abilities cannot come back.
Alzheimer’s disease is a common form of dementia; however, there are many others. Other irreversible dementias include vascular dementia (due to strokes), Lewy Body disease, frontotemporal dementia, Creutzfeldt-Jakob disease, Parkinson’s disease, and Huntington’s disease.
These conditions can have similar and overlapping symptoms, and many of them can only be diagnosed with certainty by autopsy of the brain.”
OTHER DEMENTIAS
“Other dementias” resemble Alzheimer’s disease in that they also involve a progressive degeneration of brain cells that is currently irreversible. There are many different types of dementia, although some are far more common than others.
- Young onset dementia
- Mild Cognitive Impairment
- Vascular dementia
- Mixed dementia
- Frontotemporal dementia
- Lewy body dementia
- Creutzfeldt-Jakob disease
- Down syndrome
- Rarer forms of dementia
A small percentage of dementias are reversible, occurring as a secondary development in treatable conditions. Toxic reactions to prescription or over the counter medications are the most common cause of reversible dementia. Others include dietary or vitamin B12 deficiencies, infections, tumours, alcoholism, inflammatory states, hormonal dysfunction, environmental toxins, drug abuse, and depression.
Stages of Alzheimer's disease
IMPORTANT TO REMEMBER THAT THE DISEASE AFFECTS EACH PERSON DIFFERENTLY
Early Stage Signs and Symptoms
- Short term memory loss
- loss of focus/concentration
- Disorganized
- Taking longer with normal daily tasks
- Trouble handling money/paying bills
- Difficulty walking
- Depression
Middle Stage Signs and Symptoms
- Increase memory loss
- Increase loss of focus
- Does not recognise family and friends
- Disorientation to time and place
- Difficulty with language and problems with reading, writing and numbers
- Personality changes
- Inappropriate outbursts
- Loss of inhibition
- Repetition of movements/statements
- Bowel and bladder incontinence
- Disrupted sleep patterns
- Visual-spatial problems
- Sadness or depression
Late Stage Signs and Symptoms
- Dependent for all care
- Totally incontinent
- Inability to communicate verbally
- Weight loss
- Increased sleep
- Difficulty swallowing
Treatment
Drug Treatments for Alzheimer's Disease
How to Reduce Risk
Click here to learn more about how to reduce your risk of Alzheimer's disease.
Life Story Activity
 In this activity you will answer the following questions to add to your life story:
In this activity you will answer the following questions to add to your life story:
- What things do you do in your life that you think could increase your risk of developing dementia? Think about modifiable and non-modifiable risks.
- List three lifestyle practises that help you to maintain your physical and mental health?
- What would be some practises that you could adopt to reduce your risk for developing dementia and Alzheimer’s disease?
Signs & Symptoms Quiz
 Click on the link below to access the quiz about stages and related signs and symptoms.
Click on the link below to access the quiz about stages and related signs and symptoms.
Reflection
 What dementia facts stood out for you?
What dementia facts stood out for you?
Resources
CLICK TO ACCESS: Dispelling Myths
Progression
Please click on each topic below, and read about each of the stages.
Dispelling Myths
Visit the link here to know more about dispelling myths!
Unit 4 Tools
Unit 4: Outcomes
- Develop approaches that are effective when communicating with someone with dementia
- Care of self, dealing with stress
- Professional support
- The time when care is required
Unit 4: Part 1
Tips for Caregivers
10 Simple Tips
1) Start with a Good Feeling Each Day
Caregivers have a profound influence on the emotional state of individuals with Alzheimer’s
2) Enjoy Reminiscence Therapy
| “Reminiscence Therapy” in dementia takes advantage of strong long-term memories in people with early or mid-stage dementia. Steering clear of short-term memories and reinvigorating long-term memories in Alzheimer’s patients takes advantage of powerful and emotional ties to the past. |
3) Communicate More
- Center yourself. As soon as you start to get upset or frustrated, stop and concentrate on taking deep, slow breaths while focusing on something that makes you feel calm and collected
- Use empathy. Using empathy to connect includes focusing on the experience of your loved one with memory loss. It is important to connect with their feelings, rather than the context of their words.
- Ask open questions. Use open-ended questions to redirect the conversation and to show that you’re interested in exploring what is important to them. For example, if your loved one is insisting on visiting their deceased mother, rather than reminding them that she passed away, ask her to tell you about her mother and listen with empathy as she expresses her feelings
- Try asking the extreme. Asking the extreme means that you ask the person to tell you the best or worst thing about what they are expressing.
- Enter their reality. Unless your loved one is in the very early stage of memory loss and wants to be reminded of a date, time or other reality based topic, join their journey rather than force reality on them.
4) Add Bright Lights
A down-to-earth Alzheimer’s trial provided 4 weeks of tailored light therapy.
The therapy significantly increased sleep quality,efficiency & total sleep duration. Daytime light therapy also significantly reduced rates of depression & agitation.
5) Prepare Midnight Munchies
People living with dementia often have the need to be awake at night. This can cause great concern for safety issues for caregivers. Ie: about falls, leaving the house
A facility in NY found the solution. Giving a nutritious snack allowed the person to calm and relax and return to bed
6) Ask Medication Questions
People with Alzheimer’s take a lot of medicine. Some boost memory and cognition. Others help mood, behavior and other conditions. Ensure medication is taken safely and correctly!
Learn the Basics
Know each medicine (prescription & over-the-counter).
Ask the doctor or pharmacist:
- Why is this medicine being used?
- What positive effects should I look for? When?
- How long will the person need to take it?
- How much should he or she take each day?
- When does the person need to take it?
- What if the person misses a dose?
- What are the side effects? What can I do about them?
- Can this medicine cause problems if taken with other medications?
7) Diet Right
| DR. JAMES DUKE, FORMER U.S. DEPARTMENT OF AGRICULTURE(USDA) CHIEF OF MEDICINAL PLANT RESEARCH.
A diet that keep your heart healthy will also keep your brain healthy. Many Doctors, Dieticians and Scientists recommend a Mediterranean diet.
There is also growing evidence that the use of Rosemary can have to same benefits of the drug Aricept. It has several antioxidants that prevent the breakdown of the neurotransmitter, acetylcholine, that is crucial to send messages from nerve cell to another. |
8) Air Out that Guilt
| DR. PETER RABINS, AUTHOR, MD, MPH, JOHNS HOPKINS HOSPITAL:
Caregiving for people with chronic diseases is challenging no matter what the illness. One of the unique aspects of caring for someone with Alzheimer’s disease is that caregivers almost always feel guilty in some way. Here are some suggestions to help |
|
9) Care for Yourself to Care for Them
| Take care of yourself. it is one of the most important things to do as a caregiver.
Ask family members or friends to help out, do things you enjoy, use adult day care services, or get help from a local healthcare agency. These actions can bring some relief. It also may help keep from getting ill or depressed 9 Ways You Can Take Care of Yourself
|
10) When You Tried Your Best,
Know You Did the Best.
Adapted from National Institute on Aging, National Institutes of Health
https://www.nia.nih.gov/health/infographics/make-yourself-priority-too-tips-caregivers
Communication Framework
Communication is multi-facited and to be effective must consider all the following:
- Self Awareness:Be mindful! Think about your communication style, who you are speaking to, your choice of verbal and non-verbal and be sensitive to how the other person is receiving you communication.
- Verbal Communication:Choose words that will increase your listeners understanding of what you are trying to communicate
- Non-Verbal Communication:Includes all communication other than words. The most influential part of communicating. People will believe more of what yo do than what you say.
- Listening and Responding:We spend most of our communication time listening. Need to be in the moment, listen for meaning and not to respond. Try to understand the other’s perspective when listening-be other oriented
- Adapt Your Skills:Adjust your communication including both what you are communicating and how. Your intended receiver will determine your choices.
Communication and Dementia
Click to see a list on Alzheimer's Communication
Responsive Behaviours
Click on the arrows below to navigate the slides.
Click here to access the Responsive Behaviours powerpoint
Communication Activity
 In this activity you are required to read the scenario and consider the best ways to responds. You can use the “Reply box below or write your answers on a separate piece of paper.
In this activity you are required to read the scenario and consider the best ways to responds. You can use the “Reply box below or write your answers on a separate piece of paper.
From: The Best Friends Approach to Alzheimer Carebestfriendsapproach.com
1.Coping with forgetting:
Resident states: “I just can’t remember anything! What are my grandchildren’s names?
What are helpful things to say?
2.Hallucinating:
A woman with Alzheimer’s disease comes up to her son in the family room looking upset, claiming. “There’s a big cat in my bedroom. He may hurt me!”
What are helpful things to say?
3.Wanting to go home:
A wife is perplexed that her husband wants to go home, even though he is at the house he has lived in for 40 years. He cannot imagine why he feels like a stranger in his own home.
What are helpful things to say?
4.Being Overwhelmed by questions
A family who cares for their grandfather at home finds most of the days pleasant and easy. Yet old friends who are not sensitive to Alzheimer’s disease come by several times a week and often ask a string of difficult to answer questions. The family notices increased anxiety and restlessness in the grandfather after the friends’ visit,
What are helpful things to say?
5.Wanting to stay busy
Many older adults remember a time when the workdays were long and the paychecks were small. Despite these conditions, the work ethic was strong. One woman with Alzheimer’s disease always want to keep busy—clean the house, sweep the porch, .and fold clothes. The nursing facility activities staff found themselves growing impatient and exasperated at times because their planned activities did not interest her.
What are helpful things to say?
6.Confusing past and present
Because of the failing memory and confusion that accompanies dementia, often the person will become confused about past and present. A mother might say to her daughter, “I’m waiting for Manuel. I’m sure he’ll be home any minute,” despite the fact that he is long deceased.
What are helpful things to say?
7.Coping with inappropriate sexual behavior
One of the most upsetting experiences to a caregiver is when the person makes an inappropriate sexual advance. What should happen if a man with Alzheimer’s disease makes a sexual advance toward his daughter?
What are helpful things to say?
8.Handling angry outbursts
Because of the confusion and frustration that can accompany Alzheimer’s disease, person may sometimes become angry and even strike out at caregivers. This can be very upsetting, perhaps even placing the caregiver at risk for injury. However, anger often has an identifiable cause. If the person is being bathes for example, and becomes angry it might be out of fear (e.g. fear of being undressed by someone the person may not remember, fear of drowning)
What are helpful things to say?
9.Coping with repetition
People with Alzheimer’s disease often repeat questions or requests. This can, of course, be extremely annoying to caregivers and can cause caregivers to lose their temper. A typical situation might be when the person asks, “When do we have lunch?’ over and over again.
What are helpful things to say?
Unit 4: Part 2
Rights
Click to see a list of Cargiver Bill of Rights
Caregiving & Stress
 Activity: take the Caregiving Stress Test: https://worksmartlivesmart.com/vulnerability-to-stress-test/
Activity: take the Caregiving Stress Test: https://worksmartlivesmart.com/vulnerability-to-stress-test/
18 Tips for Dealing With Stress and Tension(Canadian Mental Health Association)
Stress and Tension are normal reactions to events that threaten us. Such threats can come from accidents, financial troubles and problems on the job or with family.
The way we deal with these pressures has a lot to do with our mental, emotional and physical health.
The following are suggestions to get you started on managing the stress in your life.
- Recognize your symptoms of stress
- Look at your lifestyle and see what can be changed — in your work situation, your family situation, or your schedule
- Use relaxation techniques – yoga, meditation, deep breathing, or massage
- Exercise – Physical activity is one of the most effective stress remedies around!
- Time management – Do essential tasks and prioritize the others. Consider those who may be affected by your decisions, such as family and friends. Use a check list so you will receive satisfaction as you check off each job as it is done
- Watch your diet – Alcohol, caffeine, sugar, fats and tobacco all put a strain on your body’s ability to cope with stress. A diet with a balance of fruits, vegetables, whole grains and foods high in protein but low in fat will help create optimum health. Contact your local branch of the Heart and Stroke Foundation for further information about healthy eating
- Get enough rest and sleep
- Talk with others – Talk with friends, professional counsellors, support groups or relatives about what is bothering you
- Help others – Volunteer work can be an effective and satisfying stress reducer
- Get away for awhile – Read a book, watch a movie, play a game, listen to music or go on vacation. Leave yourself some time that’s just for you
- Work off your anger – Get physically active, dig in the garden, start a project, get your spring cleaning done
- Give in occasionally – Avoid quarrels whenever possible
- Tackle one thing at a time – Don’t try to do too much at once.
- Don’t try to be perfect
- Ease up on criticism of others
- Don’t be too competitive
- Make the first move to be friendly
- Have some fun!! Laugh and be with people you enjoy!
Community Resources
Click here for a list of resources: Resources for people with dementia living at home(Upload a document here)
Click on link below to access a map of resources in the local community:
https://uploads.knightlab.com/storymapjs/ea693130fb5a2e3dab5d1443bc54a756/home-sweet-home/index.html
Transitioning into Care
Home to me
In front of the mirror
Startled by what I see
A sombre old lady
An unknown face to me
I am to leave this old house
They say it was my own
Unfamiliar surroundings
Was it really my home
For the best mum is what I hear
Fear in their eyes
Sadness in their tone
The squeak of the door with the turn of the key
A familiar sound I think
Is my hearing deceiving me
Time to go now
One last look in the mirror
They say it is me but can it be
Smiling faces await
They are happy to see me
A sigh of relief
This is home to me
Author: Sharon Leitch MSN, RN
 REFLECTION: What does this poem say to you? Reply in the box below!
REFLECTION: What does this poem say to you? Reply in the box below!
Emotions
Common Emotions Experienced by Families During Transitions
From: MAREPhttps://uwaterloo.ca/murray-alzheimer-research-and-education-program/
Ambiguity and ambivalence
- Uncertainty surrounding what to expect during the process
- Uncertainty surrounding what life will be like for the loved one following the move
Guilt and a sense of failure
- Families blame themselves for the move
- A sense of failure in not being able to continue to provide care for the person with dementia
Anxiety and stress
- Making arrangements for the move may be stressful, and pressure to make a move quickly or before the family is ready may exacerbate this stress
Grief, loss and sadness
- Families feel these emotions related to hat they themselves are losing, as well what they see their loved one losing because of the move
Powerlessness
- Families experience a loss of control and disempowerment when they are not included in decison-making process
Loneliness and a sense of isolation
- Families feel they are alone during the transition process
Anger and resentment
- Families may prefer to continue to care in the community, but may be unable to receive needed supports to do so
- Families may not understand the process or have too much expected of them during the transition process
Feelings of relief and peace of mind
- Families experience these emotions knowing that their loved one is now going to be caed for in a safe and secure environment.
End of Life
Lets talk end of life care DOCUMENT
Living well till the end
For end-of–life care to be meaningful to the person who is living in the terminal phase of their illness we must know their goals of care. Total pain needs must include physical, psychological, social and spiritual needs. ….
Bereavement
My Life Story
If Not Now
Reflection
 Is there a resource you would like to recommend? If so, please write in reply box below.
Is there a resource you would like to recommend? If so, please write in reply box below.
Resources
You’re doing your best: Alzheimer’s Weekly
Free subscription:http://www.alzheimersweekly.com
The Team
Judith DeGroot
Judith DeGroot has completed her Master’s degree at the University of British Columbia and is presently teaching in the Health Care Assistant program at KPU. Her main areas of interest are in gerontology, Dementia and Dementia care, and the development of Open Educational Resources. She is presently working with the City of Surrey, exploring the development of a Dementia Friendly Community that will support individuals to live satisfied, productive and fulfilled lives in their own homes and communities.
Sharon Leitch
Sharon Leitch has worked in a variety of health care settings and in diverse roles through the continuum of Health Care. Her passion in nursing has evolved over the years from the adrenaline rush of ICU to the peace and tranquility of Hospice care. She holds a Master of Science in Nursing, graduating from the University of British Columbia in 2007. Her philosophy of teaching has evolved from seven years of experiential experience as a faculty instructor at KPU. Her overarching aspirations as a teacher are threefold:
- to facilitate learning that is meaningful to each individual student;
- to provide a safe learning environment for all;
- to inspire self growth and a foundation for lifelong learning.
Her research interest is focused on what it means to be a “dementia friendly community.” She is engaged in examining how communities can best support the diverse needs of people living with dementia and their care providers. She aspires to become a practical resource for people living with Dementia and health care professionals who hope to provide person centered care that is meaningful.
Harj Randhawa
Harj Randhawa is a third-year student in the Bachelors of Science in Nursing at Kwantlen Polytechnic University (KPU). Her passion is to make a difference in the lives of others experiencing acute or chronic health issues through providing nursing care that is person-centered. Her areas of interest include Emergency and Critical Care. She also has a keen interest in technology, and supported the development of the OER course by designing the website, and making sure it is easy to navigate.
Aimee Fauteux
Aimee Fauteux is a Research Impact Coordinator at Kwantlen Polytechnic University (KPU) who is responsible for supporting KPU’s knowledge dissemination and exchange activities between faculty, student researchers and the broader community. She produces a variety of plain language materials online and offline for diverse audiences (both internal and external) by synthesizing results of research, research impact stories, public communications, website content, background for media requests, and content to support revenue development activities. She is also currently completing her MA in Intercultural and International Communication at Royal Roads University.
Contact
Your feedback is important to us, let us know how you found this course to be! Feel free to ask any questions or inquiries you may have as well.
This course is a replication of the info found on this website:https://dementiavoiceandchoice.com/