Section 6.6: Control and Prevention of Malaria in the Community
6.6 CONTROL AND PREVENTION OF MALARIA IN THE COMMUNITY
As a health worker, you must have realised how dangerous malaria is. It causes a lot of absenteeism in school and in work places. I suppose you have also experienced how difficult it can be to manage a child with severe or complicated malaria. Worse still, malaria can kill. It is therefore important that we try to control malaria transmission and if possible prevent it. At the beginning of this unit, you learnt that malaria is transmitted by a mosquito. There are over one hundred different species of mosquitoes in Kenya. Only four species, however, transmit malaria. Only the Anopheles mosquitoes transmit malaria. To distinguish Anopheles from nuisance mosquitoes, look at how the mosquito rests on the wall. The Anopheles holds its abdomen in the air and flies soundlessly. This is important because when you see many Anopheles mosquitoes, you should inform the Public Health Officer or Public Health Technicians so that appropriate action can be taken. Remember that the number of cases of malaria is related to the number of malaria transmitting mosquitoes. The number of mosquitoes, too, depends on the temperature, rainfall and mosquito control activities such as spraying.
For breeding, mosquitoes need water. This is why the rainy season is so important for transmission of malaria. During the dry season, there is little surface water for mosquitoes breeding.
From the records in your health unit, calculate the percentages of malaria occurring in each month for the past one year. On a separate piece of paper, plot this on a bar chart. Which months have the highest transmission? Which months have the lowest transmission? When is the rainy season? When is the dry season? What is the relationship between malaria and the seasons of the year?
From your bar chart, you may have noticed that malaria peaks at the beginning and the end of the rainy periods. You should note that very heavy rainfall tends to wash away the immature stages of the mosquito. You should use this information to help you plan your malaria control activities at the health facility and in the community. For example:
• You can order enough stocks of antimalarials for the health unit depending on the period of the year, if your local climatic conditions do not vary much from year to year. You also learnt earlier in this unit that epidemics of malaria occur in the highlands of this country. This is because malaria is affected by altitude. High altitude is usually associated with low temperatures that do not favour mosquito breeding. Environmental degradation, coupled with climate change in these areas, has raised overall temperatures to levels favourable for mosquito breeding. This mosquito breeding in the highlands has introduced malaria in once malaria-free areas. Communities in these areas are now at risk of having many people suffering from malaria at the same time.
Why is it important to cover water containers or fill the pools of water?
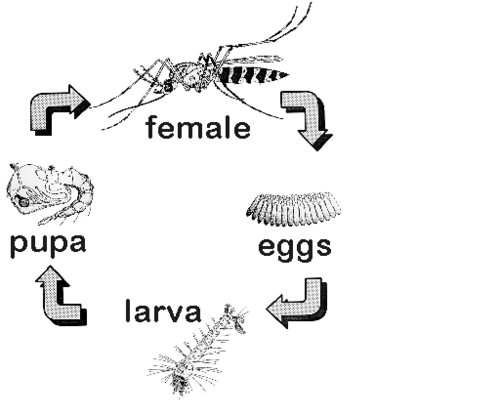
The life history of a mosquito is very short, which is why mosquitoes increase rapidly when it starts to rain. See figure (6.5). The female mosquito lays 40 to 200 eggs in or near clean water. The eggs hatch after 24 hours and turn into larvae. The larvae mature and turn into pupae (4 – 5 days). The adult insect forms inside the pupae. When the adult is ready to emerge, the skin of the pupae ruptures and the mosquito flies away. The whole cycle takes seven days in ideal conditions, although it can take as long as 21 days.
The adult mosquitoes mate immediately after emerging out of the pupa. The female will then seek a blood meal (preferably human) to help the eggs to mature. If she succeeds in feeding on a person, the eggs mature and she will begin laying eggs in 3 days.
Anopheles mosquitoes become infested with malaria parasites by feeding on a person who has malaria. The malaria parasites develop for 10 days before the mosquito can transmit them during the next bite. Therefore, the mosquitoes have to live for 2 to 3 weeks before they can transmit malaria. Spraying of walls and the use of other methods of killing the mosquito adults destroys them before they are able to spread the malaria parasites.
Now that we know the life cycle and habitats of mosquitoes, we can carry out certain control measures directed at killing the immature stages and the adult mosquitoes. We can also prevent mosquitoes from biting people. This can be done by an individual, a household, or the community.
What can the individual do?
1. An individual can prevent mosquitoes from biting him/her and his/her family by: • Wearing protective clothing to minimize the exposure of the skin to the mosquitoes • Using mosquito nets, insecticide treated or not • Netting especially of the windows • Indoor spraying • Use of insect repellents such as mosquito coils • Limiting outdoor activities from dusk to dawn, the time when transmission mostly occurs
2. An individual can also seek treatment early to destroy or eliminate the malaria parasites.
What can the community do?
A community can:
1. Fill in potholes, drain swamps, remove water containers (cans, tyres, etc), control water weeds and improve water courses to prevent or reduce the breeding of mosquitoes.
2. Destroy the larvae of mosquitoes in possible breeding sites by applying larvicides. This can be done in towns or urban centres but it is not cost effective in rural areas.
What else can be done?
1. In collaboration with other relevant actors, the health worker can plan educational programmes to make the community aware of the measures they can take.
2. CHEMOPROPHYLAXIS is very effective but is not a replacement for the above measures. The current situation in Kenya is that:
• There is no need for a person who has always lived in a malaria area to take chemoprophylaxis. This lowers his resistance to the disease. • People who travel from malaria free areas to malaria infested areas must take either mefloquine, atovaquin-proguainil or doxycylene .( See Tables 6.6, Table 6.7 and Table 6.8 for dosages) • Children with sickle cell disease should be given chemoprophylaxis with proguanil, available under the brand name Paludrine, for life
(see Table 6.9 )
• Patients with tropical splenomegaly (hyperimmune malaria splenomegaly) should also take proguanil • In the endemic areas, intermittent preventive treatment should be given to the pregnant women at the beginning of the 2nd and third trimesters as discussed earlier.
Below are the formulations and dosage schedules of the chemoprophylactic agents.
Mefloquine is available in two formulations: mefloquine hydrochloride 274 mg containing 250 mg of the base and mefloquine hydrochloride 250 mg containing 228 mg of the base. Mefloquine is administered once weekly at a dose of 5 mg/kg body weight to a maximum of 250 mg (see table 6.6). Mefloquine is started 2-3 weeks before departure, taken during the whole stay in the malaria endemic area and continued for 4 weeks after leaving the malaria endemic area.
Table 6.6 Dosing schedule of mefloquine.
Image:Dosing.PNG
| 2-4 | 5-7 | 8-9 |
| bet | yui | koj |
| Weight | Age | No of tablets per week |
|---|---|---|
| <5 kg | 3 months | Not recommended |
| 5-12 kg | 23-23 months | ¼ |
| 13-24 kg | 2-7 years | ½ |
| 25-35 kg | 8-10 years | ¾ |
| 36 and above | 11 years and above | 1 |
The most common side effects of mefloquine include nausea, vomiting, abdominal pain and diarrhoea; these side effects are dose related and self-limiting. Central nervous system related side effects include dysphoria, dizziness, ataxia, headache, some visual and auditory disturbances, sleep disturbances, nightmares and convulsions. Mefloquine is contraindicated during the first trimester of pregnancy and in infants less than 5 kg. Atovaquone-Proguanil Atovaquone-proguanil is available in two formulations. The adult tablets are film coated and contain 250 mg of atovaquone and 100 mg of proguanil hydrochloride. The paediatric tablets contain 62.5 mg of atovaquone and 25 mg of proguanil hydrochloride.
Atovaquone-proguanil is taken daily starting 1 day before departure to a malaria endemic area, taken throughout the stay and continued for 7 days after leaving the malarial area (see Table 6.7 for dosage).
Table 6.7 Dosage of atovaquone-proguanil 62.5 mg and proguanil 25 mg tablets . Weight Number of tablets Daily dose Atovaquone(A)+proguani(P) <11 kg Not recommended 11-20 kg 1 62.5mg A+ 25 mg P 21-30 kg 2 125mg A + 50 mg P 31-40 kg 3 187.5 mg A+ 75 mg P
Atovaquone-proguanil should be taken with food or milk at the same time daily. Its side effects include abdominal pain, nausea, vomiting, diarrhoea, headache, anorexia and coughing. Atovaquone-proguanil is contraindicated in pregnancy, in persons with hypersensitivity to atovaquone and or proguanil and caution is indicated in patients with renal failure.
Doxycyclene Doxyclene is available in two formulations: tablets containing 100 mg of doxycylene hydrochloride and capsules containing 100 mg of doxyclene hydrochloride. Doxyclene is taken daily starting 1 day before departure to a malaria endemic area, taken throughout the stay and continued for 4 weeks after leaving the malarial area (see 6.8)
.Table 6.8 Dosing schedule of doxyclene.
Weight in kg Age in years No of tablets <25 <8 Contraindicated
25-35 8-10 ½
36-50 11-13 ¾ 50 and above 14 and above 1
Proguanil
Proguanil is available in tablets of 100 mg of proguanil hydrochloride containing 87 mg of proguanil base. It is taken daily at a dose of 3 mg/kg starting 2 days before travel and continued for 4 weeks after leaving the malarial area. In sickle cell disease patients proguanil is administered for life. Table 6.9 shows the dosing schedule of proguanil.
The side effects of proguanil, when given at low dose, are most commonly nausea, and diarrhoea and rarely hair loss and mouth ulcers. At high doses, proguanil may cause abdominal pain, vomiting, and haematuria.
The use of proguanil is contraindicated in patients with liver or kidney dysfunction. Antiacids, for example, magnessium trisilicate, decrease the absorption of proguanil.
Table 6.9 Dosage schedule of proguanil.
Weight Age Number of tablets per day 5-8 kg <8 months ¼ 9-16 kg 8 months-3 years ½ 17-24 kg 4-7 yrs ¾ 25-35 kg 8-10 yrs 1 36-50 kg 11- 13 yrs 1½ 50 + kg 14+ yrs 2
Chemoprophylaxis and other preventive measures are not 100% effective. Therefore, malaria is a possibility in people who develop fever within 3 months of travel to an endemic area. These people should seek medical care immediately.