Lesson 9: Immunization
Contents
UNIT 9: IMMUNISATION
INTRODUCTION:
Infectious diseases cause much illness, death and may result in disabilities to a child. It is therefore important to protect the child against the common infections which affect young children.
In this Unit we shall look at how the body is assisted by immunization to form chemical substances called antibodies which protect it by increasing body immunity against infections. We shall discuss the six preventable childhood infections, the national immunization schedule and how to provide immunization services.
{{Objectives|
By the end of this unit, you will be able to:
- Define the following terms: immunisation, vaccine, cold chain.
- Explain the different types of immunity.
- Describe the six childhood immunisable diseases.
- Identify and treat or refer where necessary children suffering from any of the childhood immunisable diseases.
- Describe the National immunisation schedule
- Explain the importance of carrying out National Immunisation Days (NIDs).
9.1: DEFINITION OF TERMS
|
Immunisation: Immunisation is the process of introducing weakened or killed germs (vaccines) into the body, which increase body immunity to protect one from a particular disease. These weakened or killed germs stimulate the body to produce antibodies that will fight or weaken any disease organism that attempts to enter the body. Immunity: Immunity is derived from the word “immune” which means that the individual has enough defence mechanisms to fight and kill or weaken micro-organisms. Immunity is therefore the ability of the body to fight against certain disease organisms. An individual whose body has this ability is said to be immune to disease. When micro-organisms (also known as immunogens) such as the measles virus enter the body for the first time, the body produces a special substance known as antibodies. These antibodies fight disease organisms and kill them. If micro-organisms enter the body again the body will recognise them, having met them before, and quickly reproduces the same antibodies to kill them. Each kind of antibody that is produced matches with only one particular organism. This is why antibodies against one disease such as measles do not protect a person against another disease such as Tuberculosis (Tb). Vaccines: Vaccines are substances prepared from micro-organisms (germs or viruses), which are live vaccines (weakened) or killed vaccines. When vaccines are given to someone, he/she develops immunity to particular diseases. There are particular vaccines made to protect against particular diseases, as you will come to learn later in this unit. Examples of live vaccines are the BCG, measles and polio vaccines. While examples of killed vaccines are DPT, Hepatitis B (Hep-B) and Haemophilus Influenza Type B (Hib). Cold chain: Cold chain is the system which keeps viable vaccines potent at the required cold temperatures right from the manufacturer up to the person who receives them (such as a child). |
The success of protecting our children against the six childhood immunisable diseases depends on maintenance of cold chain. If properly maintained, the cold chain system keeps vaccines potent and they are able to do their work properly. You will learn more about the cold chain system later in this unit.
Now that we have defined some of the common terms, we can discuss the different types of immunity.
9.2: TYPES OF IMMUNITY
There are two types of immunity:
- Active Immunity
- Passive Immunity
These are further sub-divided into Natural Immunity and Artificial Immunity.
1) Active Immunity: Active immunity occurs when a person makes his own antibodies against disease. This occurs in two ways.
a. Natural Active Immunity: Natural active immunity occurs when a person contracts a disease and the body makes its own antibodies against that particular disease-causing organism. For example, if a child contracts measles, the child’s body will produce antibodies against the measles virus, and will be immune against other attacks of measles. This is life long immunity.
This is called natural active immunity. It is natural because it occurs in normal course of life without any medical intervention. It is active because the body actively develops antibodies. This type of immunity is also commonly referred to as natural ACQUIRED active immunity.
b. Artificial Active Immunity: Another way to stimulate the body to produce antibodies is by administering either attenuated (weakened) or killed organisms or modified products of an organism. This occurs when a person is given certain types of vaccines.
Advantages of active immunity: Active immunity is the best kind of immunity because it lasts for many years, (such as tetanus) and in some diseases immunity lasts for life (such as measles).
Disadvantages of active immunity: In the case of natural active immunity, which evolves out of suffering from the disease, the disease may be so severe that it may kill the child. Because of the costs of caring for the sick child, natural immunity is expensive to the family health services and the nation at large.
Artificial active immunity (administering the vaccine) takes time to give adequate protection.
2) Passive Immunity: Passive immunity occurs when ready-made antibodies are given to a person. Unlike active immunity, the body does not make its own antibodies. Instead, the body receives ready-made ones. There are two types of passive immunity:
There are two types of passive immunity.
a. Natural Passive Immunity: This type of immunity occurs when a baby receives antibodies from its mother during the time the baby is still in the mother’s womb.
The mothers’ blood contains antibodies to some of the diseases she had during her life. The mother’s blood comes into close contact with the baby’s blood in the placenta. In the process, the mother’s antibodies are passed to the baby in a ready-made form, and will protect the child against these diseases. This immunity is not long lasting, as it disappears within a period of 6-9 months of life. It is therefore reinforced by active artificial immunity.
For example, the measles antibodies that a baby receives from the mother may be much reduced by the time the baby is 9 months old. This makes it necessary to immunise the baby at this age for measles to reinforce the immunity.
Another example: If a pregnant woman is immunised against tetanus with tetanus toxoid vaccine, she makes antibodies against tetanus bacilli which her baby receives as passive immunity against tetanus. These antibodies last for only a few months. That is why the baby is immunised by giving DPT vaccine to reinforce this immunity. You will learn more about vaccines later in this unit.
b. Artificial Passive Immunity: A person gets artificial passive immunity when he/she receives ready-made antibodies in the form of a serum that is injected into the body. Such antibodies are usually drawn from an animal. One example of such serum is the Anti Tetanus Serum (ATS), which is given to patients with tetanus. Another example is the anti-rabies serum that is given to protect against rabies after dog or other animal bites.
Advantages of passive immunity: Antibodies are ready made and a person does not have to wait for his/her body to produce them. This usually takes a relatively shorter period than active immunity, and a person gets immediate protection to fight against infection as the antibodies are ready made. For example, artificial passive immunity is used in treatment of neonatal tetanus when ATS is given to the neonate..
Disadvantages of passive immunity: Passive immunity is short lived. For example, children born to mothers with high antibody levels against polio disease are protected for the first several weeks of life. Since the child receiving the antibodies has not made them himself and there is no antigen (vaccine) to stimulate the body to produce more, the antibodies disappear in a few months of life, and protection is lost.
Also, allergic reactions can sometimes occur. For example, some people have an allergic reaction when they receive Anti Tetanus Serum (ATS). It is advisable to give a test dose of ATS before giving a full dose.
To summarise the advantages and disadvantages of active and passive immunity, we say the following:
- Active immunity lasts longer, but its protection is not immediate.
- Passive immunity provides immediate protection, but it is short-lived and some serums cause allergy.
|
Point to Remember: It is advisable to give a test dose of ATS before giving the full dose, and watch for any reaction.
|
HERD IMMUNITY:
Now that we understand the different types of immunity, their advantages and disadvantages, it is important to discuss the concept of herd immunity. Herd immunity is used to refer to the level of immunity in a community as a whole.
A community is said to have a high level of herd immunity when a high percentage (70% - 80%) of its child population has been protected through immunisation. An infection introduced into a community with a high level of herd immunity will not spread, since most of children have immunity and very few are susceptible.
On the other hand, a community with a high percentage of its child population not immunised, is said to have a low level of herd immunity, and is susceptible to epidemics as the disease will spread quickly among children.
One of the intentions of the Kenyan Expanded Programme on Immunisation (KEPI) is to attain high levels of immunisation coverage of all children eligible for immunisation, so as to control and eradicate childhood immunisable diseases.
SUMMARY
Before we discuss the next topic, let us remind ourselves of what we have so far covered.
In the first two sections we defined the terms immunisation, immunity, vaccines and cold chain. We also discussed different types of immunity, such as active immunity and passive immunity. We learned that these types of immunity are further subdivided into a natural and artificial category. We examined the advantages and disadvantages of each category of immunity. Finally, we discussed the concept of herd immunity. I hope you enjoyed the topic and you can now explain what you have learned to your colleagues at work.
In our next topic we shall discuss those childhood diseases that Kenya, and indeed the World Health Organisation all over the world, are targeting with immunisation. This way we hope to protect children below five years of age against these diseases
9.3: CHILDHOOD IMMUNISABLE DISEASES:
Before continuing, do the activity below.
| 3
What is the name of the organisation that co-ordinates immunisation services in Kenya ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… List the six childhood immunisable diseases: ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
I am sure you got the answers right. The Kenya Expanded Programme on Immunisation (KEPI) is the organisation that co-ordinates immunisation services in Kenya. It was established with the aim of preventing immunisable diseases that cause high mortality, morbidity and disability among our children.
The six childhood immunisable diseases targeted by KEPI are:
- Tuberculosis (TB)
- Poliomyelitis (Polio)
- Diphtheria
- Pertussis (Whooping cough)
- Tetanus
- Measles
|
It is now routine practice to immunise against Hepatitis B and haemophilus Influenzae type B in Kenya.
|
The above diseases were selected because:
- The vaccines for their immunization are available, cheap and effective and give long term immunity. In some cases, the immunity is life long.
- These diseases are among the highest cause of death (mortality) and constant sickness (morbidity) among children below 9 years of age, the under-five children.
- The diseases are immunisable and it is cheaper to immunise children than to treat them when they fall sick.
- The diseases are highly transmitted (spread easily) among children hence leading to epidemics. Yet, if many are vaccinated a community may develop herd immunity thus reducing the spread of diseases.
Target Groups for KEPI:
KEPI targets specific groups for immunization,namely::
- Infants (under one year)
- Children 1 - 9 years (under five)
- Women of child bearing age (19-49)
- Pregnant mothers
|
NOTE: Women of child-bearing age, including pregnant mothers, are given Tetanus Toxoid (TT) vaccine to protect their unborn babies against Tetanus
|
We shall now look at each of six diseases targeted by KEPI in turn. This will help you understand why they were selected and how to manage them. You will note that diseases such as TB, measles, and neonatal tetanus are discussed in great detail. This is because they are very common and cause a lot of ill health and death.
1) TUBERCULOSIS:
Tuberculosis, commonly abbreviated as TB, is a chronic infection that may affect any parts of the body, mainly the lungs and is caused by bacteria. It is a common cause of illness and death in children, if not properly treated. It spreads easily from one person to another through the infected person’s droplets (from coughing) that contain Mycobacterium Tuberculosis. It is important to note that because of HIV?AIDS, TB incidence is on the increase.
Children catch TB from adults who are sick and who cough out TB bacilli into the air. When a child breathes in the bacilli, he/she slowly develops the disease.
Although TB bacilli are spread in droplets by adults, who cough them in their sputum, children are very rarely infectious. We say that adults have sputum positive or open tuberculosis when their sputum contains tubercle bacilli. When an infected adult holds a child, and coughs out the TB bacilli into the air, the chances of the child getting infected are very high. We know that overcrowding and poor house ventilation facilitate the spreading of this disease. We can therefore understand why infants can easily get infected because of the way they are held.
Since we know that children get TB from adults, it is important to find out which children are at risk of getting the disease, so as to prevent it. The first group at risk are those children whose mothers suffer from TB. The next group is comprised of those children who get frequent attacks of infection such as malaria, measles, diarrhoea and acute respiratory tract infections.
Other children likely to get TB are those who are malnourished or who are HIV positive, since these children already have lowered immunity. Children can also get TB from milk contaminated with bovine tubercle bacilli, though this is less common.
Now that we have learnt how TB is transmitted, let us discuss the signs and symptoms.
Signs and symptoms of TB:
| 4
What would you look for in determining whether or not a child has TB? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Compare your answer with the following.
When a child is brought to you in a clinic or Health unit, take a good history, examine the child and carry out the relevant investigations. We discussed how to do this in the first unit of this course. Once you have ruled out all other causes, you might suspect that he/she has TB if you find any of the following:
- Chronic cough (cough which lasts for more than 30 days).
- Enlarged lymph nodes in the neck.
- Fever which comes and goes.
- Loss of weight (wasting), often with loss of appetite.
- When a child with Pneumonia or other type of acute cough does not get better after two weeks of treatment. This is especially true when there is fever and weight loss.
Now do the following activity.
| 5
If you get a child with the above signs and symptoms at a rural Health unit, what should you do? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Diagnosis and Treatment: A child who presents with the above signs and symptoms should be suspected of having TB. If this child is in a rural health unit, you should REFER him/her to the hospital for further investigations and treatment.
Before you refer the child, however, you should give him/her some drugs to soothe the throat and reduce the cough. You should also explain clearly the purpose of the drugs given, then advise the caretaker to take the child to the hospital for further investigations as per IMCI guidelines. Remember to give the caretaker some referral notes about the child.
Explain clearly that it is for the child’s benefit that she/he be investigated, as the problem may be serious. Explain also that although TB is serious, it is also curable, especially when treated early. Let the caretaker know that the reason you are referring the child is because you do not have adequate facilities for treatment.
If during history taking you discover that there are others in the family with a persistent cough, explain the importance of all of them going for investigation. Reassure the caretaker that the child will be well if the problem is discovered early and treated adequately. Stress the importance of following instructions, feeding the child and taking him/her for immunisation.
The diagnosis of pulmonary TB is difficult in an acutely ill marasmic child.
If a child is acutely ill with marasmic signs, know that he/she may well die before the diagnosis is confirmed. This is because a tuberculosis test will likely be negative – in a marasmic child there is often no AFB in the sputum or gastric contents and the X-ray picture will be non-specific. Further tests will have to be done to confirm TB, and the child is already sick and weak. So, if you see an acutely ill marasmic child and you suspect TB, go ahead and start him/her on penicillin and chloramphenical and refer immediately. Remember that pulmonary TB can progress into pneumonia.
In a child whose natural immunity is compromised by malnutrition, the infection can spread into the pleura as tuberculosis pleurisy, and the pressure of hilar glands on bronchi may cause collapse of a part or whole of a lobe (atelectasis). Lymphogenous or Haematogenous spread miliary tuberculosis may occur, causing TB meningitis, abdominal TB or TB of the bones or renal TB. This is why the start of antibiotics will be helpful before you transfer the child.
As we have said, to confirm the diagnosis of TB, there are investigations that should be carried out. We said that you need to refer this child. In hospital, the following investigations can be done:
- Tuberculin test. There are three:
- Mantoux test which is done by introducing tuberculin (0.1 ml of 1: 1000 or 1:2000 through an intradermal infection.
- Heat test, which is when tuberculin is introduced through a special heat gun.
In all cases a tuberculin reaction will indicate whether a child has TB infection. The test, however, cannot be used alone.
- Sputum examination. Sputum is taken for microscopic examination. Gastric content aspirated early in the morning could also be used, as it contains sputum.
- Blood test to check Hb. A check for erythrocyte sedimentation rate (ESR) can also be done. Hb will be low in an active TB and there will be high erythrocyte sedimentation rate.
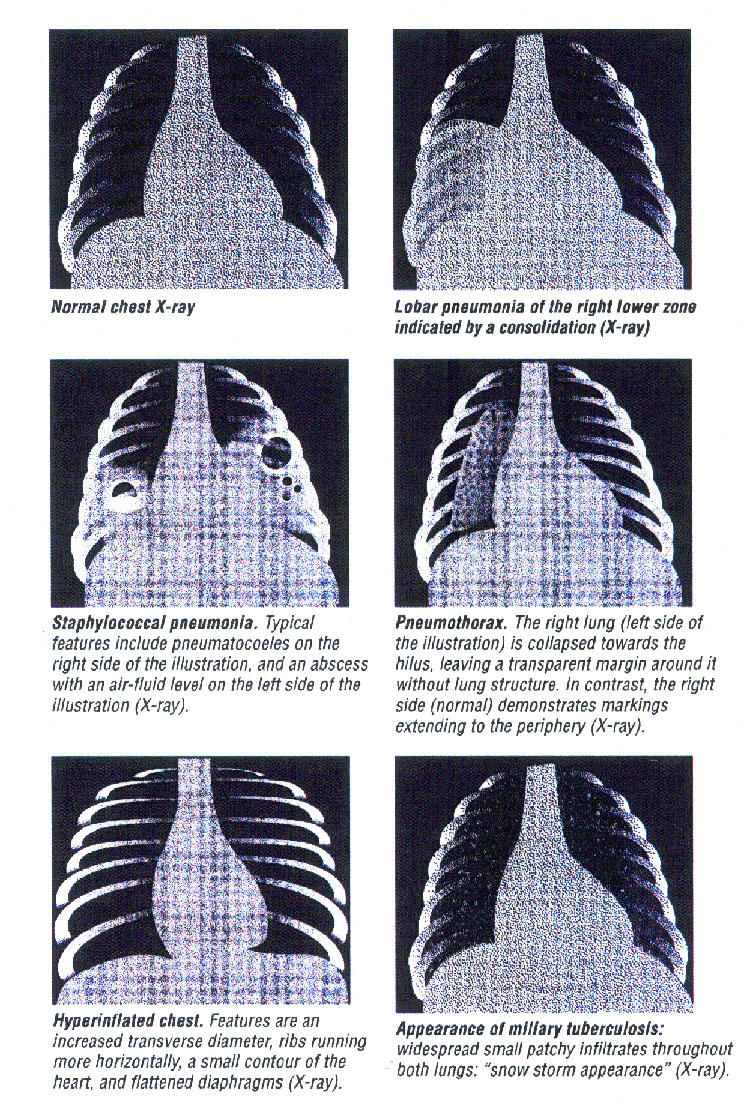
- The chest X-ray is another important investigation.
.
Let us now see how this child will be treated once TB is confirmed.
Treatment: If you recall, we said that a child gets TB from an adult, most likely the mother because of close contact. There is, therefore, more to be done than just treating the infected child. In the management of a child with TB, it is important to reassure the parent or adult who infected him/or her. It is equally important to check if other children in the family are also infected. This is called contact tracing.
Treatment of a child with Pulmonary TB is in two phases: initial phase of 2-3 months on possibly 3 drugs, Isoniazid (H), Rifampicin (R), Ethambutol (E). Streptomycin (S) may be added for a period of two months. Continuous phase of 4-6 months using HER.
A visibly ill child will often have pulmonary TB. If so, he/she should be put on streptomycin, isomacid, Rifampicin and pyrazinomide or ethambutol (4 drugs) daily, if possible, or the streptomycin 2 x per week for 2 months. Then isomiazid and rifampicin, or if HIV is suspected ethambutol and pyrazinamide for 4 months.
TB meningitis or advanced miliary TB is treated like extrapulmonary TB, but this time the duration of treatment is 10 months, and prednisolone 2mg/kg/day is added. If the child is HIV positive, the treatment should continue for an additional 3 months, or 13 months total.
Now that we can see how just serious TB is, and we have seen some of the drugs needed to treat it. Let us turn to how it can be prevented.
Prevention:
Before going on with the reading, complete the activity below.
| 6
How can you prevent tuberculosis in your community? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
You can prevent the spread of TB in your community by doing the following:
- Immunising all children at birth or first contact with BCG vaccine.
- Encouraging the community through IEC, which we discussed in Unit 3, to avoid overcrowding and to have houses properly ventilated.
- Encouraging good nutrition in the community.
- Identifying and referring all suspected TB patients to hospital for early diagnosis and treatment.
- Early diagnosis and treatment of all TB patients
- Investigation of family members and close contacts of a case.
2) POLIOMYELITIS (Polio):
Have you ever seen a person infected with polio? Before going on with the reading, complete the activity.
| 7
What causes polio? Write your answer in the space provided: ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… How is polio transmitted? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
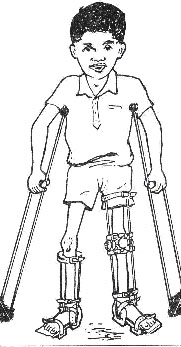
Poliomyelitis, commonly referred to as polio, is a highly infectious disease that is caused by a virus that affects the motor neurones of the spinal cord and sometimes the brain, resulting in paralysis. It commonly affects the muscles of the limbs (arms and legs).
There are three related types of polio virus. These are Types 1, 2 and 3. All three types cause paralysis, but the most frequent cause of epidemic polio is polio Type 1.
Almost all the under-five children in Kenya who have not been immunised have a risk of getting polio infection. However, only in a small proportion of these children can the infection result in paralysis. The disabilities it causes vary and can sometimes cause death.
The polio virus is highly communicable. An infected child will probably infect all other non-immune children, especially where sanitation is poor.
Mode of transmission: Polio Virus is mainly spread through faeces and by droplet infection. The latter is a rare route of transmission.
When an infected child passes the virus in stools, it spreads from child to child through contaminated water, food, utensils and hands. After being swallowed, the virus multiplies in the throat and intestines and may spread to the child’s nerves through the blood stream. However, polio virus does not affect the sensory nerves.
Complete the activity below before continuing with the reading.
Key signs and symptoms:
| 8
What are the key signs and symptoms that would make you suspect a child is infected with polio? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Do your answers agree with the following?
Key signs and symptoms of polio infection include:
- Weakness and paralysis of one or more limbs.
- There is no sensory loss. The sense of pain and touch remain normal.
- The paralysis only affects the muscles (Flaccid paralysis).
.
Fig. 9.1: A child with polio
Although the above are the key signs and symptoms of polio, the disease may start out with the following signs, which are common with other diseases.
- Fever and general malaise
- Nausea and vomiting
- Headache
- Abdominal pain
The incubation period for polio is 10 - 21 days.
If you come across a child presenting with the above signs and symptoms you should refer to the hospital for further assessment, management and rehabilitation. You should also inform the District Medical Officer immediately. Currently there is polio eradication initiative which requires that every child with Flaccid Paralysis (AFP), have his or her stool collected and investigated for polio virus. Make sure you report any AFP cases to your surveillance team
Treatment
No specific treatment is available. However, the following are principles of management that are a general guide.
- The patient is strictly advised to rest in bed.
- Avoid any injections as these pave the way to (Precipitate) paralysis.
Prevention: The good news is that polio can be prevented. Poliomyletis is mainly prevented by immunisation using Oral Polio Vaccine. OPV effectively prevents polio. Since the polio virus is highly communicable, especially where sanitation is poor, it is important to advise the community to improve general hygiene and sanitation in their homes as a preventive measure against poliomyelitis.
|
The case definition for suspected polio is: ANY CASE OF FLACCID (floppy) PARALYSIS FOLLOWING A RECENT FEVER, USUALLY AFFECTING A LIMB/LIMBS NOT PRIMARILY CAUSED BY INJURY. |
Polio Eradication: The polio virus can be eradicated from the face of the earth like smallpox. Experience in the Americas, where polio has been eliminated since August 1991, demonstrates the possibility of eradication.
Currently there is a global and national effort to combat the virus and Kenya has joined this struggle with the support of WHO, UNICEF and Rotary International. You will learn more details about this eradication initiative later in this unit.
Before continuing with the reading, complete the activity below.
| 9
What causes diphtheria? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… What are the signs and symptoms of diphtheria? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
3. DIPHTHERIA:
Diphtheria is an acute infectious disease of the throat and tonsils, caused by bacteria. These bacteria produce typical lesions on the mucous membranae of the upper respiratory tract. Toxins released from the lesions cause severe general symptoms that can damage the heart and peripheral nerves. The incubation period is 2 - 9 days. It is spread by droplet infection, but contaminated milk and dust can also carry the disease.
Diphtheria is a rare disease in Kenya, but due to its severity and high cause of death it should be prevented.
Key signs and symptoms of diphtheria
The following are the things to look for in deciding if a child has diphtheria.
- The child has fever and is acutely sick and toxic.
- The neck is enormously swollen – more swollen than you see in tonsillitis (Bullneck).
- Sore throat with hoarseness and difficulty in swallowing.
- Grey membrane at the back of the throat that spreads past the tonsils. The membrane looks like small piece of a dirty cloth stuck to the child's throat.
Complications: A child with diphtheria may develop the following complications:
- Myocarditis - the local lesion’s toxins attack the heart muscle, causing signs of cardiac failure.
- Respiratory paralysis.
- Nerve involvement, causing paralysis of the limbs.
| 10
How would you manage a child that comes to your health facility with diphtheria? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
A child with diphtheria is very ill. This child should be referred to hospital for admission and careful nursing.
Prevention: Diphtheria can be prevented by:
Immunisation using the Pentavalent vaccine which is given as described later in the section on the immunization schedule.
Health advice: Health advice should be given to parents with children suffering from Diphtheria to:
- Take the child to hospital for careful nursing.
- Bring all other children under age five for check up and immunisation.
- Give the child bed rest for four weeks or until the child feels well.
4) Whooping Cough (pertussis):
Whooping cough, which is also known as pertussis, is an acute respiratory tract infection commonly found in children. There is no protection against pertussis from maternal antibodies.
| 11
What causes whooping cough? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… What would make you suspect that a child has whooping cough? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
See if your answers include the following.
Whooping cough is caused by a bacterium called Bordetella pertussis. Coughing spells ending in a whoop is characteristic of the disease. Sometimes vomiting follows the whoop. The whoop may be absent in children who are under 6 months of age.
Whooping cough is transmitted by droplet infection. The incubation period is 7-10 days. A child with whooping cough will often lose weight or fail to gain weight due to decreased appetite and vomiting.
Signs and symptoms of whooping cough: The signs and symptoms of whooping cough vary with the age of the child. Most children under 6 months of age may have a cough that does not end with a whoop. If a child is under 6 months of age, he/she will present with:
- Fever
- A cough that lasts more than three weeks.
If a child is six months of age or more, he/she will present with:
- Fever
- Sneezing, watering of eyes and irritation of the throat.
- Paroxysms of coughing followed by a whooping sound at the end of long coughing spells. This whooping sound begins within one to two weeks of the start of the chronic cough. Talking, coughing or crying can precipitate the paroxysms of cough.
- The under side of the tongue may become sore and ulcerate.
- Attacks are more frequent at night and the cough can last several weeks.
Complications: Like any other diseases, whooping cough has complications. These include the following:
- Pneumonia
- Convulsions and brain damage
- Malnutrition due to vomiting and loss of appetite
Management of a child with whooping cough:
| 12
How would you manage a child with whooping cough at your health facility? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
See if your explanation agrees with the following:
In managing a child with whooping cough you need to do the following:
- Encourage the mother to give nutritious food to prevent malnutrition.
- Encourage breastfeeding or the drinking of plenty of oral fluids immediately after a coughing attack to prevent dehydration.
- Avoid giving sedatives or cough suppressants because they may make the illness worse.
- Refer the child to hospital immediately for further management.
Prevention: Whooping cough in your community can be prevented by:
- Giving Pentavalent vaccine (immunisation) to all children below 9 years of age according to the immunisation schedule described earlier..
- Healthy children should avoid contact with children who are suffering from whooping cough.
- Sending all suspected cases of whooping cough for treatment in the hospital.
Key messages to mothers of children with whooping cough
- Give small and frequent feeds to the child to avoid vomiting and thus prevent malnutrition.
- Take children who have not been immunised for immunisation.
5) NEONATAL TETANUS:
Neonatal Tetanus is tetanus infection of the newborn (less than one-month-old infant) acquired after delivery. Tetanus is caused by a spore-forming bacterium known as clostridium tetanae.
In the newborn it enters the body through the umbilical stump which may be contaminated during cutting, tying and dressing, or through other cuts. The disease usually presents with muscle spasms and a failure to breastfeed in a baby who was otherwise born healthy. Nearly all cases of neonatal tetanus occur within 4-10 days after birth. Most newborns with this disease unfortunately die.
It is thus very important that the disease be prevented.
Mode of transmission of Neonatal Tetanus
| 13
Explain how neonatal tetanus is transmitted: ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Compare your explanation with the following:
Tetanus bacteria live in the intestines of grass eating animals such as cattle, sheep, goats and donkeys. The ground where they pass their faeces becomes heavily infected for a long time. In Kenya, the umbilical cord is the commonest site of bacterial entry in the newborn. The infection occurs when the umbilical cord is either cut with a contaminated instrument such as a knife or razor blade, or when the wound is treated with cow dung or soil (as it is done in some communities). Delivery in a dirty environment can also lead to infection with tetanus.
Once the bacteria gain entry in the baby’s body, they multiply and cause signs and symptoms of the disease.
| 14
How can you detect neonatal tetanus in a baby? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Read on to see if you have got it right.
A baby with neonatal tetanus presents with the following key signs and symptoms:
- The baby stops sucking the breast.
- Muscle rigidity and spasms occur with the head bent backwards, known as opisthotonus posture.
- False smile. The baby looks as if he/she is smiling, yet he/she is not (Risus sardonicus). This is due to muscle spasms.
Complications:
A child with Neonatal Tetanus may develop the following conditions if not treated early.
- Fracture of the vertebrae due to spasms.
- Brain damage due to lack of oxygen supply to the brain which occurs during spasms
- Failure to breathe, which leads to death.
Management of a baby with neonatal tetanus:
A baby with this disease is likely to die if not managed properly and quickly. The moment you diagnose neonatal tetanus, do the following:
- Give a dose of rectal diazepam.
- Clean the infected umbilicus with diluted 0.09% chlorohexidine solution (Hibitane).
- Refer to hospital for further management having explained to the mother the need for such referral as per IMCI guidelines.
Prevention:
You can prevent neonatal tetanus in the community by doing the following:
- Immunising women of childbearing age (19-49yrs) and pregnant women with Tetanus Toxoid vaccine.
- Delivering mothers in clean environment.
- Avoiding putting anything on the umbilical stump except antiseptic methylated spirit.
- Cutting the cord with sterile equipment such as sterile scissors or sterile razor blade.
- Tying the cord with sterile ligature, cloth, or clean thread.
- Tetanus toxoid schedule for pregnant women.
NEONATAL TETANUS CAN BE PREVENTED by immunisation of mothers, proper umbilical cord care, and a clean delivery.
6) MEASLES:
Measles is a very infectious and dangerous disease caused by a virus. Its incubation is 10-14 days. It commonly occurs in children and has high morbidity and mortality among children under 1 year of age.
Mode of transmission of measles: Measles is spread very rapidly by droplets. This means that a child infected with measles spreads the virus by releasing very fine droplets into the air through coughing, sneezing, or crying.
Measles usually occurs in epidemics among children 7 to 9 months old. Before that age the young baby is fairly well protected by the antibodies from the mother. By the age of 9 years almost all children have been in contact with measles virus.
The mortality is high, particularly in malnourished children, due to complications such as those of the respiratory tract. If the child survives the infection, there will be life long immunity and he/she will not get measles again. Remember that is called natural active immunity.
Signs and symptoms of measles: As a Health worker you may have seen a child with measles. You can attempt to answer this question.
| 15
How do you decide that a child is suffering from measles? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
The key signs and symptoms of measles are:
- High fever, usually above 38.9 degrees centigrade before the rash appears.
- Cough, possibly with running nose before the rash appears.
- Rash all over the body, lasting about seven days;
- Conjunctivitis (red eyes)
Apart from the above key signs and symptoms you might also see:
- Rash starting from the head and neck
- Koplik spots – white spots on a red background on the mucous membranes of the mouth, inside the child’s cheeks.
- Diarrhoea and vomiting.
- Refusal to feed
Measles and nutrition:
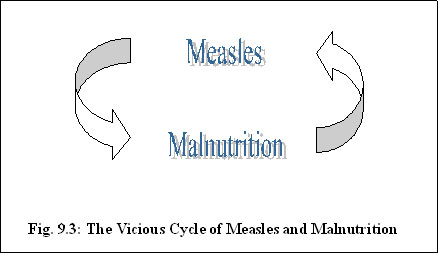
Measles interferes with the nutrition of the child.
- When a child has measles his/her food intake is reduced, particularly when the child has sore mouth or is too sick to take enough food and fluids and has loss of appetite.
- Because of the diarrhoea that accompanies measles, the child loses a lot of protein leading to protein energy malnutrition. This can progress to kwashiorkor or marasmus.
- Specific deficiencies of Vitamin A may occur during measles, leading to the damage of the corneal epithelium and blindness.
- High fever increases breakdown of food and body protein, ending in malnutrition.
- Traditional beliefs can interfere with the nutrition of the child. One dangerous traditional belief is that a child with measles should not eat eggs, meat, fish, or drink milk. This denies the child of proteins and energy.
- Measles is more severe in children with malnutrition and in whom complications occur more frequently causing death.
Fig. 9.2: A child presenting with measles. Measles interrupts nutrition and reduces the immune status of a child. A child with measles develops sores and is sometimes too sick to take enough food. A child also develops persistent diarrhoea and will experience inadequate food absorption due to the disease and its complications. In the above circumstances a child ends up developing malnutrition.
When a child already has malnutrition, his/her resistance to infection is lowered. When exposed to the measles virus, the disease is severe. The interaction of measles infection and malnutrition in this case becomes a vicious cycle.
Complications: If measles is not diagnosed and managed early the child may develop the following:
- Underweight with other signs of malnutrition.
- Severe diarrhoea leading to dehydration.
- Otitis media (inflammation of the middle part of the ear).
- Stomatitis (sores in the mouth).
- Infection of the conjunctiva.. This is a complication if there is eye pus discharge.
- Pneumonia.
- Laryngo-tracheo-bronchitis (LTB).
- Acute bronchitis.
Management of a child with measles
Complete the following activity before continuing with the reading.
| 16
What would you do to manage a child with measles at your health facility? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
There are no drugs that can be used to treat or cure the measles virus. All treatment is for symptoms. When managing a child with measles in your health facility, you should do the following:
- Lower the body temperature by tepid sponging.
- Give plenty of fluids such as fruit juice, ORS, or soup to prevent dehydration.
- Clean the eyes and apply tetracycline eye ointment 1% at six-hour intervals for seven days to prevent conjunctivitis.
- Give Vitamin A supplement, 100 000 iu capsules once daily for three days.
- Give frequent nutritious feeds to prevent malnutrition.
If a child presents with the following conditions you should refer to hospital immediately. These include:
- Severe dehydration
- Laryngo-trachea-bronchitis
- Severe pneumonia
- Severe malnutrition
Prevention of measles: Measles can be prevented by:
- Immunisation: Immunisation at 9 months of age or at any visit of an un-immunised child under five years of age will protect them against measles,
unless the child has already suffered from measles.
- Giving nutritious food. This will boost the immunity of the children.
- Exclusive breastfeeding of infants up to 6 months.
- Encourage good weaning practices
Health advice to parents of children infected with measles: Mothers of children who have measles should be given the following advice. Parents should:
- Maintain the hygiene of the child by cleaning the eyes and mouth.
- Provide plenty of fluids.
- Provide nutritious foods.
- Take the child to the hospital if the child develops complications.
SUMMARY: We have looked at the causes of six immunisable diseases, transmission, key signs and symptoms, complications, management and how they can be prevented. I hope you are now conversant with this topic and you can provide appropriate advice and services to parents in your community.
9.3: NATIONAL IMMUNISATION SCHEDULE:
Kenya Expanded Programme on Immunisation (KEPI) has a plan it follows to administer vaccines. This plan clearly shows the vaccines that are given, the dosage, the time interval between doses and the site of administration. This is called the National Immunisation Schedule. This standard plan provides a guide to all health workers in the country involved in immunisation. The immunisation schedule varies from country to country and can change from time to time, depending on scientific discoveries.
As a health worker who participates in the immunisation of children, you should carefully study the National immunisation schedule and always use it as a reference guide whenever you are providing this service. Let us now discuss the vaccines used by KEPI and how to administer them.
Before continuing with the reading, complete the activity.
| 17
What are the vaccines used by KEPI? List them: ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
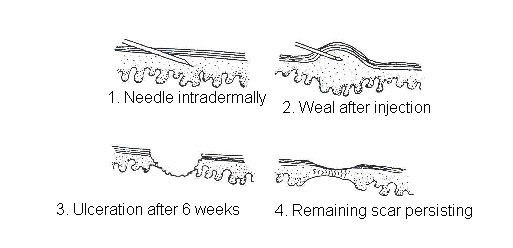
1) BCG (Bacillus Calmette-Guerin ) Vaccine:
This is a live attenuated (weakened) bacterial vaccine. It is used in the immunisation programme to protect the child against Tuberculosis (Tb). BCG vaccine is given in a single dose at birth or first contact. The vaccine is very sensitive to light and loses much of its potency when exposed to light. It is given by injecting the child intradermally (in the skin) at the right upper arm. The amount of 0.09mls is recommended for children up to eleven months of age, and 0.1 ml for children after eleven months of age.
2) Polio Vaccine:
Polio vaccine is a live attenuated (weakened) virus, used in the immunisation programme to protect children against poliomyelitis. The Sabin type is given orally (by mouth) in Kenya. Some countries use another type, called Salk vaccine, which is given by injection.
Oral polio vaccine is given four times beginning at birth (polio 0); at 6 weeks (polio 1); at 10 weeks (polio 2); and at 14 weeks (polio 3); respectively. Two drops in the mouth are recommended for each dose. It should be noted that booster doses are sometimes given to all children below five years of age in the entire country regardless of immunisation status. This is done during National Immunisation Days (NIDs), whose primary objective is to eradicate poliomyelitis. You will learn more about NIDs later in this unit.
Polio Immunisation Schedule:
- Polio 0: Birth or first contact
- Polio 1: 6 weeks
- Polio 2: 10 weeks
- Polio 3: 14 weeks
3) Pentavalent Vaccine:
Pentavalent has five vaccines which include DPT and HepB and Hib. The DPT vaccine is commonly referred to as Triple Vaccine because it is used to prevent three diseases: namely, diphtheria, pertussis and tetanus. The diphtheria and tetanus parts of the vaccine are made from the respective toxins, while the pertussis vaccine is made of a killed bacterial antigen. It has become necessary to add Hepatitis B (Hep B) and Haemophilus Influenzae type b (Hib) vaccines to DPT to form what is now known as Pentavalent vaccine (five vaccines)
The Pentavalent vaccine is given by injecting the child intramuscularly (in the muscle) at the left upper thigh. It is given three times, beginning at 6 weeks), at 10 weeks and 14 weeks respectively. A dose of 0.9 ml is recommended at each time it is given.
Pentavalent Immunsiation Schedule:
- DPT + Hep B + Hib I - 6 weeks
- DPT + Hep B + Hib II - 10 weeks
- DPT + Hep B + Hib III - 14 weeks
4) TETANUS TOXOID VACCINE:
This is a toxoid vaccine used in the immunisation programme to prevent children against neonatal tetanus. KEPI targets all women of childbearing age (19-49 years) and pregnant mothers for Tetanus Toxoid (TT) vaccination.
|
It is better and safe to give two doses of Tetanus Toxoid (TT) vaccine to any pregnant woman if you are not sure she has had TT in a previous pregnancy.
|
The aim is to use the TT Vaccine to provide passive immunity for unborn babies, through transfer of the mother’s antibodies (natural passive immunity). This type of immunity reduces with time and is normally boosted by giving the child Pentavalent at six weeks after birth.
Tetanus Toxoid Vaccination Schedule: Every woman of child bearing age (19-49years), including pregnant women, should get 9 doses of Tetanus Toxoid (TT) vaccine. The schedule is as follows:
- First dose (TT1): At first contact or as early as possible during pregnancy.
- Second dose (TT2): At least 4 weeks after first dose.
- Third dose (TT3): At least 6 months after second dose.
- Fourth dose (TT4): At least 1 year after third dose.
- Fifth dose (TT9): At least 1 year after fourth dose.
Now that we have looked at the vaccines used by KEPI and briefly discussed the schedule of each vaccine, you should carefully study the national immunisation schedule illustrated in Table 1 below so as to understand more about this topic.
Table 1: National Immunization Schedule
| Age | Vaccine |
|---|---|
| At birth | BCG
Oral Polio |
| At 6 weeks | DPT + Hep B + Hib
Oral Polio I |
| At 10 weeks | DPT + Hep B + Hib
Oral Polio II |
| At 14 weeks | DPT + Hep B + Hib
Oral Polio III |
| At 9 months | Measles |
Let us now discuss the administration of these vaccines in more detail.
Killed vaccine or the Pentavalent vaccine. Killed vaccines are given three times because they do not stimulate the body to produce antibodies as well as the live vaccines. When the second and the third doses are given, the body’s memory of the earlier dose quickly leads into production of more antibodies.
It is nice to remember that Polio vaccine is made up of three polio viruses and the oral polio vaccine is given three times to enable each of the three viruses to stimulate the production of antibodies.
Immunzation coverage should be high to reduce disease transmission. As health workers we should aim to achieve an Immunization coverage of over 80%. All children should be immunised at every opportunity. There is no contraindication for immunisation. If immunisation is done daily, this improves immunisation coverage. Children with minor illnesses should be immunised. Misconception that sick children should not be immunized should be discarded. Very seriously sick children admitted to hospital should be immunised on discharge. Malnourished children should also be immunised. The danger of a vaccine of any given type to the malnourished child is much less than the infection itself. For children with HIV/AIDS, BCG can sprad rapidly and thus should be treated as opportunistic infection
Administering Vaccines: Vaccines used in the immunisation programme (KEPI) are in different forms. Some vaccines are in powder form and must be dissolved in the diluent supplied with them, while others come in liquid form and will not need a diluent. Therefore, there is a need to prepare some vaccines before immunisation. Here is the way to prepare each vaccine. We shall start with polio vaccine.
• Preparing Polio Vaccine: To prepare this vaccine you should do the following.
- If a dropper is separate, attach it securely to the vial (bottle).
- Keep polio vaccine shaded from sunlight during the immunisation session.
- Place the vial on a frozen ice pack or place it in the hole of the sponge placed at the mouth of a vaccine carrier, which is provided for this purpose to maintain the temperature.
• Preparing BCG and Measles Vaccines: To prepare these vaccines, you should do the following:
- Use the diluent provided for each vaccine. Diluent should be cold: +4 - +8 degrees centigrade.
- Use different 9ml syringes for mixing measles and BCG vaccines.
- Draw up the full, required amount of the diluent provided as per instruction on the vial.
- Inject diluent into vial.
- Draw and expel mixture back into the bottle three times or until the vaccine is mixed.
- Do not shake the vial.
- Measles and BCG vials should be placed on a frozen ice pack or use the sponge in the vaccine carrier for maintaining the correct temperature.
- Draw 0.9ml of measles vaccine (recommended dosage).
- Draw 0.09ml of BCG vaccine for babies up to 11 months old, and 0.1ml for babies above 11 months (recommended dosage)
• Preparing DPT and TT vaccines: DPT and TT vaccines come in liquid form. You will not need to dissolve or mix them.
- Remove metal top from the vial
- Draw 0.9ml into the sterile syringe
- Remove bubbles
- Keep the vaccines shaded from light.
Important points to remember:
- Never take two vials of the same vaccine out of the vaccine carrier at the same time.
- Do not mix vaccines until mothers and children are present.
- Mix one vial of a particular vaccine at a time
- Keep opened vials of polio, measles, and BCG vaccines on a frozen ice pack or use the sponge in the vaccine carrier. Their temperature must be carefully maintained.
- Do not keep vials of DPT and TT vaccines directly on the frozen ice pack.
- Open the vaccine carrier only when necessary.
NEVER SHAKE VACCINE VIALS!!!
After preparing vaccines, the next step is to administer them. Before administering vaccines you should always remember the following important points.
REMEMBER:
- Use one sterile syringe and needle per vaccine (antigen) per child or mother.
- Avoid holding loaded syringes in your hands for long so as not to expose vaccine to heat or direct sunlight.
- Inform each parent what type of vaccine you are giving the child, the possible reactions to it, what to do about the reactions, and when to bring the child back for more immunisation.
- Listen to parents and encourage questions.
- Remove any child’s clothes that are in your way when vaccinating
| 18
What steps should you take during immunisations? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
During immunisation you should:
- Ask the mother to hold the child firmly to restrict his/her movement during immunisation.
- Administer the vaccine.
- Give specific health information about each vaccine.
Now let us discuss how each vaccine is administered.
1) Administering BCG vaccine:
| 19
Explain how to administer the BCG vaccine to a child: ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Follow these steps when administering BCG:
- Clean the skin with cotton wool soaked in clean water and let it dry.
- Hold the middle of the child's upper right arm firmly with your left hand.
- Hold the syringe by the barrel with the millilitre scale upward and the needle pointing in the direction of the child's shoulder. Do not touch the plunger.
- Point the needle against the skin, barrel turned up, about 3cm above your thumb. Gently insert its tip into the upper layer of the skin.
- Make sure that the needle is in the skin (intradermal) and not under the skin, as shown in Fig. 9.4. If the needle goes under the skin, take it out and insert it again. If you bend the needle, replace it with another sterile one.
- Holding the barrel with your index and middle finger, put your thumb on the plunger.
- Holding the syringe flat, that is, parallel to the surface of the skin, inject the vaccine intradermally. For children above 11 months of age, inject 0.1 ml. For children under 11 months of age, inject 0.09 ml.
- If the vaccine is injected correctly into the skin, a wheal, with the surface pitted like an orange peel, will appear at the injection site. An indication that the vaccine has been injected incorrectly is that the plunger will move much more easily when the needle is injected under the skin than when it is injected in the skin.
Fig. 9.4: Needle Position and Depth of Insertion
9. If there is no local reaction, re-immunise the child.
10. Give the mother health information about BCG. This is what you should say:
- In 9 to 7 days a small sore will appear at the place where the injection was given.
- The sore might ooze a bit and will last for 6 to 8 weeks.
- Keep the baby's arm clean with soap and water.
- Do not put medicine or dressing on the sore.
- The sore will not hurt, and it will heal by itself.
11. Change the syringe and needle after each antigen (vaccine) and each child.
12. Fill in the Immunisation Tally Sheet in BCG section.
13. Administer the next antigen.
2) Administering DPT vaccine
How is the DPT vaccine administered?
| 20
These are the steps to follow when administering DPT vaccine: ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
- Ask the mother to hold the child across her lap so that the front of the child’s thigh is facing upwards. Then ask her to hold his/her legs to keep him/her from moving.
- Clean the site to be injected with a cotton swab moistened with clean water, and let it dry.
- Place your thumb and index finger on each side of the place you intend to inject. Stretch the skin slightly.
- Quickly push the needle deeply into the muscle, as shown in Fig. 9.4 (intramuscular). Pull the plunger back. If there is blood in the syringe, withdraw the needle and discard the vaccine. DO NOT use that syringe and needle again until they have been sterilised. Obtain a sterile syringe and needle and new vaccine.
- If no blood appears in the syringe, inject 0.9 ml. of vaccine.
- Withdraw the needle.
- Rub the injection spot quickly with a clean piece of cotton swab.
- Give health advice about DPT. Tell the mother that:
- DPT may cause some tenderness at the place the injection was given.
- This tenderness will go away after a few days.
- DPT may cause fever but the fever will subside in 24 hours.
- Teach the mother how to care for a child with fever.
- Fill in the Immunisation Tally Sheet appropriately.
- Use another needle and syringe to vaccinate the next child.
3) Administering Oral Polio Vaccine:
When administering Oral Polio vaccine these are the steps to follow:
- Ask the child's mother whether the child has diarrhoea. If "yes" note this on the child's card and tell the mother that this dose of polio needs to be repeated after one month.
- This child (with diarrhoea) should have a total of 4 to 9 doses of Polio vaccine, depending on whether the child got Polio 0 or not.
- Use the dropper or device supplied with the vaccine.
- If the child will not open his mouth, gently squeeze his cheeks to open his mouth.
- Put 2 drops of vaccine on the child's tongue.
- Fill in the Immunisation Tally Sheet appropriately.
Note that every child below 9 years of age should receive an extra 2 doses of Oral Polio Vaccine (OPV) each year during National Immunisation Days (NIDS) whether he/she was immunised before or not.
4) Administering Measles Vaccine
When administering measles vaccine, this is what you should do:
- Use a sterile syringe and needle for each injection. Use a sterile syringe to draw 0.9 ml dose of the mixed measles vaccine.
- Ask the mother to expose the child's left upper arm and hold the child firmly to restrict his movement
- Clean the injection site with a cotton swab moistened with clean water, and let it dry.
- With the fingers of one hand, pinch the skin on the outer side of the upper arm.
- Hold the syringe at an acute angle to the child's arm.
- Inject the vaccine subcutaneously.
- To avoid injecting vaccine into a vein, pull the plunger back slightly before injecting the vaccine. If blood is drawn into the syringe, withdraw the needle and discard the vaccine. DO #NOT use the syringe and needle again until they have been sterilised. Obtain another sterile syringe, needle and vaccine. Press the plunger gently; inject 0.9 ml. of vaccine.
- Withdraw the needle. If a drop of blood appears, wipe it off with a cotton swab.
- Fill in the Immunisation Tally Sheet appropriately.
- Give the mother health advice about measles. Tell her that
- Some children have a mild rash after 7 to 10 days of getting measles vaccine.
- This rash is mild and it will show that the vaccine is working very well.
- Use another sterile needle and syringe to vaccinate the next child.
5) Administering Tetanus Toxoid Vaccine (TT):
The following are the steps to take when administering TT vaccine:
- Give TT injection intramuscularly on the outer side of the upper arm or outer aspect of the thigh, whichever of the two sites the woman prefers.
- Fill in the Immunisation Tally Sheet appropriately.
- Give health advice about TT to women. Tell them that Tetanus Toxoid can cause some fever for a few hours and some tenderness at the site where the injection was given for a few days.
|
NOTE: Do not use detergents to clean injection sites during immunisations because detergents can destroy the vaccines.
|
Specific health advice during immunisations: It is important that parents or guardians are given health advice when they bring children for immunisation. This is what you should tell them:
- The name of the vaccine you are giving the child. In case of a pregnant or non-pregnant woman, you should tell her the name of the vaccine you are administering.
- The name of the disease the vaccine prevents.
- The possible side effects and what to do about them. For example, a child may develop fever and a sore leg or arm. Tell the caretaker that if this happens, to give the child a tepid sponge bath and extra fluids to lower the temperature. The parent can give Paracetamol if the temperature is still high after tepid sponging, to lower the temperature and reduce pain.
- The return date for additional vaccines.
9.4: STRATEGIES FOR ERADICATION OF CHILDHOOD IMMUNISABLE DISEASES.
In this section we shall discuss the globally recommended strategies for eradication of childhood immunisable diseases. We shall look at the Global and National Polio Eradication initiative and the role of health workers in National Immunisation Days (NIDS) for polio eradication.
| 21
What do you understand by the term eradication? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Compare your answer with this one: "Eradication" means to get rid of something. It has been proven that the six childhood immunisable diseases can be drastically reduced and that some of them can completely be wiped out of the globe. You should remember that small pox was completely eradicated from the globe following effective immunisation.
To achieve this, there are certain strategies that have been recommended by WHO. The following are some of these strategies:
- Strengthening of routine immunisation activities to achieve and maintain the highest levels of coverage for all antigens.
- Mass vaccination of children within the shortest possible time through National Immunisation Days (NIDS)
- Strengthening EPI target disease surveillance system such that every case of any of these diseases is reported, fully investigated and contacts of positive cases protected.
- Conducting "mopping-up" immunisation when the diseases are reduced to focal transmission.
Although Kenya has been carrying out immunisation to prevent the six childhood diseases with over 79% immunisation coverage for some antigens, there is yet a number of children who are still infected because they were not immunized. There is therefore a need to improve on our immunisation coverage and eradicate these diseases..
Routine immunisation needs to be strengthened so as to achieve over 99% coverage, and other strategies like mass immunisation should be adapted to supplement routine immunisation.
Global and National Initiative for Polio Eradication:
The polio eradication initiative (PEI) is a global collaborative effort. WHO, UNICEF, Rotary International, the U.S. Center for Disease Control (CDC), prevention governments and non governmental organizations (NGOs) are strongly committed to the initiate. Their generous financial and technical support has been critical in achieving the tremendous progress made to date.
Kenya has joined the rest of the world to wipe out poliomyelitis from the face of the earth. In addition to encouraging routine immunisation, Kenya has adapted the National Immunisation Days (NIDs) as a supplementary activity to achieve this goal.
| 22
What are National Immunisation Days? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
National Immunisation Days are special days when Oral Polio Vaccine (OPV) is given to all children up to 99 months (below 9 years) of age in the entire country, regardless of their immunisation status. NIDs occur as two rounds, four to six weeks apart, during the low season of polio virus transmission.
The doses of OPV during NIDs are considered EXTRA doses that supplement and do NOT replace doses given during routine immunisation services. Children must continue to receive their routine immunisations.
| 23
What, do you think, are the objectives of NIDs? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
The Primary objective of NIDs is to interrupt the transmission of and thereby eradicate the wild polio virus. You have already learned that polio is caused by a wild virus. You can refer to the section on the six childhood immunisable diseases.
Why polio eradication?
Poliomyelitis still remains a major crippling affliction in children throughout the developing world, including Kenya. It is estimated that it affects over 100,000 children annually.
The global initiative, support, and wild polio epidemiology makes polio eradication more feasible than eradication of other, more common diseases (like malaria, respiratory tract infections, diarrhoea and measles) in Kenya.
Why should fully immunized children receive OPV during NIDs?
There are two main reasons:
- Waning intestinal immunity: Fully immunised children with serologic immunity may have reduced intestinal immunity against polio. Therefore, extra doses will boost this intestinal immunity and decrease the likelihood of these children of being exposed to the polio virus.
- Primary vaccine failure: OPV is approximately 89% effective. Therefore, even fully immunised children may experience primary vaccine failure, and in the absence of natural exposure may not be immune to all three types of polio virus.
When are NIDs conducted?
The first two rounds of NIDs in Kenya were successfully conducted on 14-19 December 1996 and 18-19 January 1997. The second two rounds of NIDs were conducted on 2-3 August and 13-14 September 1997.
NIDS are conducted during the low season of polio transmission
| 24
What are the benefits of NIDs? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
There are many benefits of conducting NIDs. Conducting NIDs in Kenya will:
- Increase the community's awareness about immunisation and health in general.
- Involve community and national leaders, which sets a precedent for their active participation in important health initiatives.
- Give health workers extra training and supervision that can increase motivation and improve skills.
- Strengthen the management of the cold chain.
Do you, as a health worker, appreciate the above benefits? If you do, then attempt to answer the following question.
| 25
What is the role of health workers in NIDs? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Check whether you have got it right.
All health workers are expected to be involved in this noble cause of polio eradication by actively participating in National Immunisation Days. In particular, health workers should:
- Mobilise parents and caretakers! Health workers should inform parents and caretakers of the polio eradication initiative and the need for all children 0-99 months of age to receive a dose of OPV during both rounds of NIDs, regardless of their prior immunisation status.
- Advocate and sensitise the community on the importance of NIDs through meetings, day to day work, social gatherings, etc.
- Provide immunisation services in their clinics during NIDs. Health workers with clinics should encourage their clients to bring children below 9 years of age for immunisation during NIDs.
- Ensure that the community in which they reside or work is completely covered during NIDs.
- Respond to public concerns by providing adequate information on questions raised by the public, such as the many misconceptions about NIDs and HIV.
- Have their own children immunised. Health workers are influential (especially in matters pertaining to health) within their communities. It is very important that they provide a good example to the community by taking their children or relatives who are below 9 years of age for immunisation. This is not only during NIDs, but also during routine immunisation.
SUMMARY
In this section we have learned about the global and national recommended strategies for eradication of childhood immunisable diseases. We looked at the global and national polio eradication initiative through National Immunisation Days. We now know that all children below 9 years of age (0-99months) are the targets for NIDs, regardless of their prior immunisation status.
We have also learned that the doses of oral polio vaccine (OPV) given during NIDs are EXTRA doses required to boost the child's immunity. NIDs does not replace routine immunisation, but should rather strengthen it. Finally, we looked at the role of health workers in the polio eradication initiative.
You have now completed the work for this unit of the child health course. I hope you enjoyed all the sections of the unit. Look back at your answers to the questions and check them. If you are not yet clear with any section, go back and review it.
In the next unit you will learn about malaria control and prevention. As you may be aware, malaria is a dangerous disease commonly found in the tropics which affects both children and adults.
Before you do your the Tutor Marked Assignment, take your well deserved break. Remember that this assignment will be sent for correction and therefore you should make sure that it is complete.
|
DISTANCE EDUCATION COURSE TUTOR MARKED ASSIGNMENT Personal File Number: Name: Address:
UNIT 9: IMMUNISATIONS Answer all the questions. When you have finished, mail it. It will be sent back to you with comments and the next units.
b. Mrs. Mbatia's 10 weeks baby was brought to an immunisation session and it was given polio and DPT vaccines. What type of immunity did this baby get? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… 2. A mother brings her nine month old baby to your clinic. She tells you that she delivered the baby at the hospital where it was given two vaccines at birth. a. What were these two vaccines? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… b. What disease is the baby fully protected against? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… 4. A mother brings a baby of eight months old who is sick to your health facility for treatment. You take a history from the mother, carry out a thorough physical examination, and come to a conclusion that the baby is suffering from measles. a. What has made you conclude that the baby has measles? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… b. Explain how you would manage such a child: ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… 5. Answer these questions about NIDs: a. What is the primary objective of National Immunisation Days (NIDs)? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… b. Explain why fully immunised children should receive oral polio vaccine (OPV) during NIDs. ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… c. List three benefits of carrying out NIDs in Kenya: ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|