Lesson 8: Prevention and Control of Malaria
Contents
Introduction
Welcome to Unit 8 on the prevention and control of Malaria. In the last unit we discussed how to manage malaria in pregnancy. In this unit we shall learn about the various ways of preventing and controlling this disease.
Human efforts at controlling malaria dates back many years during the early Grecian and Roman times. This continued right through to 1930 when Mussolini did extensive work aimed at malaria control. In 1899 Ross’s anti larvae measures were introduced in Sierra Leone and later in 1902 he started an anti mosquito campaign in Somalia. Other notable developments were those by Le Prince who started a large-scale demonstration of mosquito control in Cuba, and later together with Gorgas, an anti mosquito campaign in Panama canal zone.
Since then a lot more has taken place. In the 1970s measures to immunize humans against P. falciparum and P. vivax were introduced. At the moment there is massive renewed interest in malaria activities following the world declaration on the control of malaria by the Ministerial conference held in Amsterdam in October 1992. This Renewed interest is further attested by the Roll Back Malaria (RBM) Initiatives which is a partnership approach to malaria control. RBM movement was launched in 1998 as joint initiative between WHO, UNICEF UNDP and the World Bank. RBM promises to halve the World’s malaria burden by the year 2010.
|
Lesson
Principles of Prevention and Control of Malaria
In the prevention and control of Malaria, it is important to combine measures aimed at breaking the “man-vector” contact cycle of transmission and curing the infected population. The control of malaria therefore involves education, vector control and control of parasites in man. The most effective control measure however is the one that breaks the “man-vector” contact cycle of transmission.
Next, let us look at methods of prevention and control of Malaria in our community.
Methods of Malaria Prevention and Control
There are various methods through which the prevention and control of Malaria can be achieved. Many of them can be done in your community. Before you read on, do activity 1, it should take you about 5 minutes to complete.
Confirm your answer as you read the following discussion.
The prevention and control of malaria can be prevented through the following ways:
- Controlling mosquito breeding;
- Preventing mosquitoes from biting people;
- Killing adult mosquitoes before they bite people;
- Killing malaria parasites in the blood before they can cause malaria. This is referred to as chemoprophylaxis;
- Early diagnosis, timely and adequate treatment of all Malaria cases.
Before you read on, do activity 2. It should take you about 5 minutes to complete.
Confirm your answer as you read the following discussion.
Rational use of vector control methods
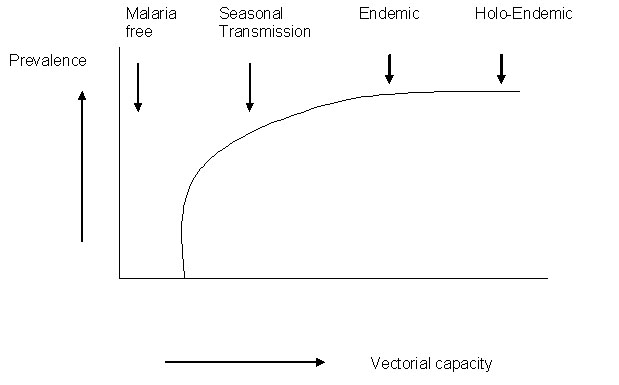
An effective vector control method should be able to reduce the vectorial capacity of mosquitoes. See Figure 8.1 on vectorial capacity of mosquitoes
There are five determinants of the choice of vector control method applied in an area. These are:
- Intensity of the disease transmission or the magnitude of the malaria burden;
- Vector behaviour, human behaviour (KAP) and environment;
- Availability of resources;
- Feasibility of timely and correct application;
- Possibility of sustainability.
Fig 8.1: Vectorial capacity of mosquitoes
Let us look at the methods suitable for different zones.
Malaria Free Zone: In this zone continuous surveillance should be maintained to keep watch of introduction of malaria in such zones.
Seasonal Transmission Zone:The most cost effective control method includes the use of Indoor Residual Spray (IRS). This includes epidemic prone areas. However, the coverage of IRS should be about 80% for high impact.
Endemic And Holoendemic Zone: In such areas the most cost effective method of control is the use of Insecticide Treated Nets (ITNs). The coverage must be in more than 80% of the community members for it to have impact.
Before you read on do activity 3, it should take you about 5 minutes to complete.
I hope your list included the following indications of vector control:
- Prevention of malaria epidemics;
- Elimination of foci in malaria free areas;
- Prevention of seasonal peaks of malaria transmission;
- Control of transmission in high-risk situations (non-immune immigrants);
- Reduction in transmission in areas of high drug resistance;
- Control of endemic malaria (LLINs and other ITMs, Environmental management).
Vector Control methods
There are various methods used in malaria vector control. These include:
*Targeted methods: these target the life cycle in water for mosquito larvae or the life cycle on land for adult mosquitoes;
*Zone specific methods:
- These depend on the intensity of transmission. Here the use of ITNs/LLINs with at least 80% is most suitable in all areas
- Use of IRS is most suitable in unstable transmission or epidemic prone zones for control of epidemics.
*Cost effective methods:for example, Indoor Residual Spray (IRS) is the most cost effective vector control method in epidemic zones.
*Methods that aim at reduction in Vector density: these are activities that result in the reduction of mosquito breeding sites and proliferation of mosquitoes. The activities include:
- Source reduction, such as larviciding, environmental management (modification & manipulation, biological control (e.g. predators and Bacillus thuringiensis Israeliensis (Bti);
- Spraying, such as, Space, Indoor Residual Spray (IRS)
*Reduction of man-vector contact: This can be achieved through the following activities:
- Barriers – Insecticide Treated Nets (LLINs/ITNS), House screening
- Repellents, fumigants and long sleeved clothing
All these methods have two main goals: to control mosquito breeding as well as prevent mosquitoes from biting people. Let us now look at how we can achieve these two goals.
Controlling mosquito breeding
Mosquitoes like to lay eggs in places with stagnant or slow flowing water. Thus, in order to control mosquito breeding, you need to marshal the concerted efforts of all members of the community. You need to work together with them, discuss and plan activities with them during your outreach programmes.
Now do activity 4, it should take you five minutes to complete.
| 4
1. List down the examples of stagnant water in your community. ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ……………………………………………………………………………… 2.Mention the methods you could use to eliminate stagnant water in your community. ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………
|
Examples of Stagnant or slow flowing water include:
- Open streams with very slow-flowing water along their banks;
- Pools of water left on the riverbed after rains have ended or as a result of poor water management;
- Swamps;
- Rice fields;
- Reservoirs; (Water tanks for storage of water (when left open);
- Small ponds;
- Pools;
- Borrow – pits;
- Canals;
- Ditches with stagnant water in and around villages;
- Animal hoof prints filled with water;
- Other objects that may collect water e.g plant pots, old car tires, empty tins, and plastic containers.
These stagnant water sites can be avoided by constructing settlements at least 2 Km away from them. Others sources such as pits, animal hoof prints, small ponds, potholes, etc, can be eliminated by:
- Using sand/soil to fill them.
- Removing all discarded containers that might collect water.
- Covering water tanks (cisterns) with mosquito mesh or lids.
- Repairing leaking taps, water pipes or drains that may provide a place to breed.
The second goal of mosquito control measures is to prevent mosquito from biting people. Let us briefly consider how this can be done.
Preventing mosquitoes from biting people
Because it is difficult to destroy all mosquito breeding sites, we need to have a alternative ways, of preventing Malaria. Adopting an alternative approach does not mean abandoning our goal of destroying breeding sites. This should remain a continuous process so that we can reduce the adult mosquito density and longevity (life span).
Before you read on, do Activity 5, it should take you 5 minutes to complete.
We hope your list included the following methods which are used to prevent mosquitoes from biting people:
- Sleeping under a mosquito net, especially an insecticide treated mosquito net;
- Applying Indoor Residual Spray (IRS). This is done by trained persons and involves spraying all walls inside a house or building with high-pressure spray pumps. The effect of this spray can last for up to 6 months. It is suitable for buildings which house many people, such as, boarding schools, hospitals, barracks and hotels. IRS is the method recommended in epidemic prone areas.
- The insecticides suitable for IRS should have a residual effect ( the longer the residual time the better)
- Should be safe (low toxicity- WHO class III).
- Should have leave stains on the sprayed surfaces
- Commonly used insecticides are pyrethroid but organophosphate (not preferred) may be used. Examples of pyrethroids commonly used include:
- Deltamethrin, lambdacyhalothrin, cypermethrin, permethrin etc
- Other methods include:
- Wearing protective clothing that covers the arms and legs, especially in the evenings;
- Applying chemical mosquito repellant cream on exposed body surfaces;
- Covering doors and windows with wire or nylon mesh/nets to prevent mosquitoes from entering the house;
- Using mosquito coils, particularly when sitting outdoors during the evenings that release smoke to keep mosquitoes away or kill them when they fly through the smoke;
- Spraying rooms with insecticide before going to bed every evening. The sprays are only effective for a few hours and so this method only protects people from mosquitoes if the doors and windows are screened;
Before you read on, do Activity 6, it should take you 5 minutes to complete.
Confirm your answer as you read the following discussion.
Indoor Residual Spraying (IRS) is a specialized vector control method recommended for housing units in epidemic prone areas and specialized settings such as hospitals, schools and other institutions. IRS deposits a specific quantity of insecticide on the wall and ceiling surfaces of a house using specialized compression spray pumps. It is important to familiarize yourselves with details of the process. The equipment recommended for Indoor Residual Spray includes the 10 litres capacity compression spray pumps with a pressure gauge such as the:
- Gloria TG series
- Hudson X-pert
The nozzle or spray tip is the most important part of the sprayer – yet the most neglected component of any spray programme. The nozzle is designed to deliver a precise volume of liquid per minute at a given pressure and to maintain a uniform spray pattern and swathe width.
RECOMMENDED STANDARD NOZZLE:
WHO recommends the use of Tee-jet 8002 for spraying absorbent surfaces such as mud or cement plaster. 80 in the Tee-Jet 8002 represents spray angle i.e., 80s, while 02 describes flow rate i.e. 0.2 US gallons or 757 ml per minute at 40 Psi.
The performance of spray pumps is determined by how well the spray man
- takes care of the pump;
- maintains the nozzle which is the most important component;
- Cleans the pump after each spraying session.
NOZZLE CALIBRATION - 8002 NOZZLE TIP
You should spray water into a measuring cylinder for 30 seconds at a pressure 40 psi. Measure the amount discharged into the measuring cylinder. The spray tips are considered excessively worn if the flow rate exceeds the flow rate of a new tip by 10%. The interpretation of nozzle condition can be determined by the guidelines given in the table below.
Table 1: Guidelines for Nozzle Condition
| Psi | Seconds | Volume measures | Interpretation (Nozzle |
|---|---|---|---|
| 40 | 30 | 380 | Normal |
| > 380 | Worn out but still serviceable | ||
| > 418 | Discard and replace |
Before you read on, do Activity 7, it should take you 5 minutes to complete.
A spray pump must be cleaned every day after spraying because:
- Active ingredient may break down;
- Wettable powder will settle and block filters;
- Chemical may damage pump components;
- Spray mix is a health hazard.
OPERATING PRESSURE AND FLOW RATE
The target dosage rate is calculated according to a specific pressure range. The following specific air pressure must be maintained:
| Psi | Kpa | Bar | |
|---|---|---|---|
| Minimum | 25 | 170 | 1.7 |
| Maximum | 40 | 276 | 2.7 |
Minimum -25 psi (170 Kpa) Maximum -40 psi (380 Kpa)
Higher pressure increases:
- the volume flow rate and hence run-off;
- rate of wear of nozzle aperture;
- spray bounce-off;
- Produces smaller droplets (do not impact on surfaces).
Lower pressure reduces the spray angle which results in reduced spray coverage (under dosing)
Table 2: Comparative wear life of different nozzle materials
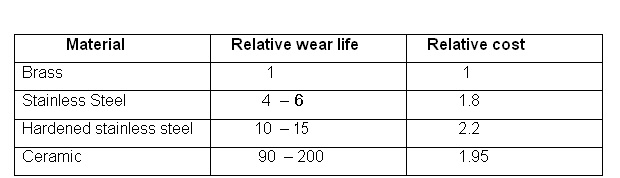
INTERPRETATION OF LIFE TIME OF DIFFERENT NOZZLE MATERIALS
Nozzle tips are made up of the following materials:
- Brass;
- Stainless Steel ;
- Hardened Stainless Steel;
- Ceramic.
Nozzle tips are subject to erosion, especially when used with water dispersible powder formulations. The degree of erosion depends on the material that the nozzle tip is made of. It also depends on the physical properties of the formulation and the amount of insecticide which has been sprayed through the tip. The most durable nozzle tip is the one made up of ceramic. We hope you are now familiar with the application of Indoor Residual Spray (IRS). Next, let us look at another common and easier method of preventing mosquitoes from biting people. This is through the use of Insecticide Treated Nets.
Insecticide Treated Nets/Long Lasting Insecticide Treated Nets (ITNs/LLINs)
Before you proceed do activity 8, it should take you about 5 minutes.
| 8
Have you heard of the following abbreviations used to refer to mosquito nets? Describe each and explain their difference. LLIN……………………………………………………………………………………………………………………………………………………………… ITN…………………………………………………………………………………………………………………………………………………………………… UTN…………………………………………………………………………………… Name three (3) effective application of LLINs/ITNs for malaria control ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………
|
Confirm your answer as you read the following discussion.
Of all the methods of preventing mosquito bites, sleeping under a mosquito net is probably the most effective. The preferred nets are the Long Lasting Insecticide Treated Net (LLIN) or ordinary Insecticide Treated Net (ITN), however, if used and maintained properly, untreated Nets (UTN) may be useful. The nets are now easily available, reasonably priced, and when used properly can be very effective. LLIN refers to a new technology of making ready-to-use pre-treated mosquito net s that do not require further treatment during its expected life span (4 – 5 years). There are two types of LLINs:
• TYPE 1 LLIN whereby the insecticide is inco-orporated into the resin which coats the net fibre during net manufacture; eg PermaNetR and OlysetR etc.
• TYPE 2 LLIN eg K-OTAB 123R treatment kits which containing a binding agent which forms a film around the net fibres, thereby keeping the Deltamethrin bound to the net fibres and protecting the molecules against the impact of washing detergents. The technology renders the insecticide to be effective for a long period even when nets are subjected to about 20 washes. ITN refers to Insecticide Treated Nets. This is a mosquito net which is treated with an insecticide with residual effect that lasts for three to six months.
For ITNs to be an effective method of malaria control, the following needs to be done:
- Acquisition or ownership of a net ;
- Regular re-treatment of nets with insecticide;
- Correct and consistent use of nets.
LLINs/ITNs reduce human contact with mosquitoes by killing them if they land on the net or by repelling them. This keeps mosquitoes away from where people are sleeping.
|
Un treated mosquito nets (UTNs) can also reduce the transmission of Malaria but are definitely less effective than LLINs/ITNs |
The following are the advantages of LLINs/ITNs over UTNs. They
- provide a high level of protection against mosquito bites hence reduce Malaria;
- kill or repel mosquitoes that touch the net while UTNs only acts as physical barrier against mosquitoes;
- reduce the number of mosquitoes in the house killing or repelling them when they try to reach the host;
- kill other insects like lice, fleas, bedbugs etc.
- Are safe for people to use.
Availability of LLINs/ITNs.
LLINs/ITNs can be obtained from public or private sources, such as:
- General merchandise shops;
- Drug shops;
- Pharmacies;
- Super markets;
- From trained health staff in public health facilities, e.g. District Medical Offices, Ministry of Health (MOH) Malaria control programme;
- Community Health Workers (CHW);
- Village Treatment Agents;
- Non Government Organizations (NGOs) such as African Medical Research Foundation (AMREF), World vision etc;
- Work places.
Treating mosquito nets with insecticides
Factory pretreated mosquito nets (e.g. PermaNet, Olyset, Duranet, smart nets etc) remain effective for about 20 washes, while nets that have been dipped with self – treated kits will remain effective for about 6 months. After the 20 washes 6 months for self-treated nets, you should either retreat the nets with approved insecticides before the rainy season or replace them all together.
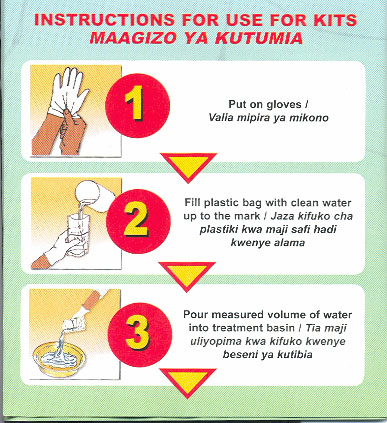
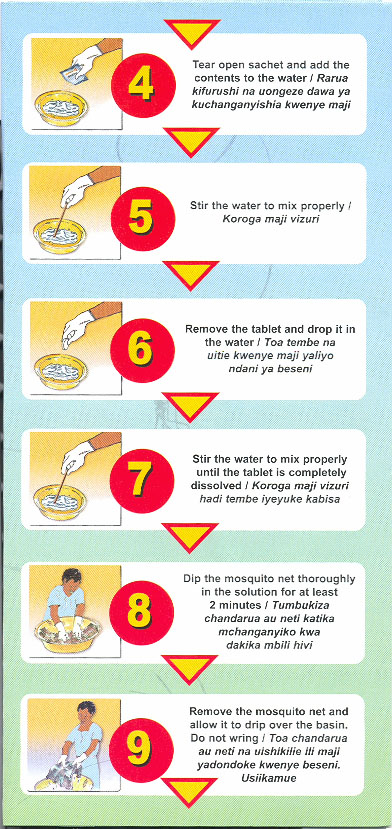
The following are some of the requirements and procedures you should follow when treating nets with insecticide.
REQUIREMENTS:
- Insecticide treatment kit.
- Mixing container (Basin, plastic basin, bucket).
- Water.
- Measuring jar (may improvise with beer or soda bottle).
*PROCEDURE:
- Select a well-ventilated area for treatment;
- Ensure that the mosquito net is clean, dry and unfolded;
- Put on protective gloves (polythene bags) on both hands, and avoid getting insecticide on your face;
- Mix the insecticide with water according to the manufacturer’s instructions;
- oak the net in solution thoroughly until all material is wet;
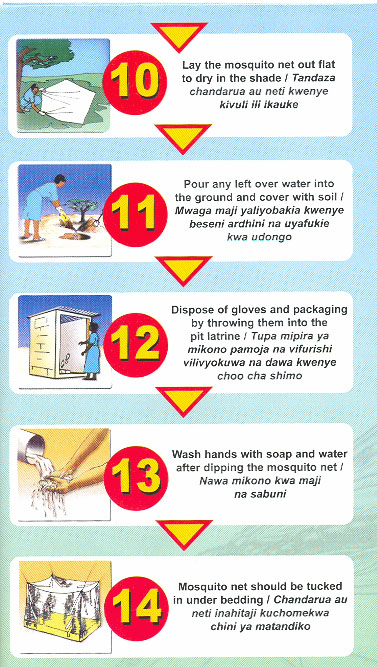
- Lift the net, and if necessary, allow it to drip over the basin. Do not wring;
- Keep wet nets away from children;
- Place the wet net to dry flat on a clean surface out of direct light;
- Dispose the excess insecticide into the ground and cover with soil or into a pit latrine.
*EFFECTIVE USE OF LLINS/ITNS.
For any ITN to effectively reduce the number of mosquitoes in the house, it must be used correctly. The following are tips for using an LLIN/ITN:
- Have the LLIN/ITN above the bed or sleeping mat.
- Use the net every night and all year and not just when mosquitoes are bothering you.
- When using the net lay it so that it covers the entire bed or sleeping mat and tuck it under the mattress or mat.
- During the day, tie the net out of the way so that it is not damaged by children playing with it.
- If using factory-pretreated nets (e.g. smart net), retreat after about 20 washes. If using self treated nets, retreat every 6 months because washing reduces the concentration of the insecticide.
|
Factory pretreated nets have the advantage of retaining the insecticide longer than self-treated nets. |
*CARING FOR MOSQUITO NET
For a mosquito net to last longer, it must be cared for correctly. The following are some tips for the care of a mosquito net:
- Handle your net gently so that it does not tear;
- Regularly inspect your net for holes and repair them;
- Wash net once every three (3) months;
- Do not smoke or use fire near it as it might catch fire.
We have learnt ways for using and maintaining LLIN/ITNs. Let us now turn to yet another method of malaria prevention and control that is, kills the malaria parasites before they cause malaria. Besides the use of LLINS/ITNS other material treated (ITMs) with insecticides e.g. curtains, wall mats, cloths etc could be used to prevent mosquito from bitting.
Killing Malaria parasite before they cause Malaria
As you well know, the methods of preventing mosquitoes from biting people may sometimes fail. That is why researchers have come up with the method of killing the parasites as they enter the blood. It is popularly known as chemoprophylaxis.
Chemoprophylaxis is only effective if a person has the adequate amount of the drug in their blood that is needed to kill the Malaria parasites. Drugs used as Chemophrophylaxis include Proguanil, Doxycycline, and Mefloquine. Mass chemoprophylaxis is not recommended in malaria endemic regions because
- It may not be sustainable - Logistic and economic constraints make it difficult to provide the treatment
- The choices of drugs for use are limited and
- Fear of drug resistance – e.g. Chloroquine resistant Malaria parasites are on the increase. In recent years resistance to Fansidar has also increased;
- Many people do not take the full course of the drugs and those who take may have undesirable side effects;
However, chemoprophylaxis is still vital for the following categories of people:
- Sicklers. These are people with sickle cell disease;
- Children below age of 5 years who have anaemia or other illnesses for whom immediate bout of Malaria would worsen their situation;
- Travelers coming from non-malarial regions to Malaria endemic areas;
- Pregnant mothers especially primi-gravidae (IPT);
- People with known lowered immunity.
Other methods of malaria control involve early diagnosis and prompt treatment of cases and killing of adult mosquitoes. Let briefly look at them.
Early diagnosis and prompt adequate treatment of all Malaria cases
You can make a definite diagnosis of Malaria from your knowledge of the history of the disease, by examining the patient and checking a blood film for parasites.
You should treat all confirmed cases with appropriate drugs according to the National Guidelines. This should be given in adequate dosage, administered through correct route, and the correct period of time recommended by certified authority. We have learnt the different methods of preventing and controlling Malaria. Let’s now turn to your role as a health worker in the prevention and control of Malaria.
The Role of Health Workers in Malaria Prevention and Control
As a health worker, you play a very essential role in the fight against Malaria. Apart from your crucial responsibilities in the management of this disease, you have an important role to play in giving health education and counseling the community about malaria. In this section we shall concentrate more on this role so that you can pass effective messages to community on malaria control and prevention.
Here are some of the messages you can pass on to your community:
- ITNs help prevent Malaria;
- It is cheaper and long lasting to prevent Malaria than to treat Malaria;
- Use LLINs/ITNs for the prevention of mosquito bites;
- Use LLINs/ITNs properly and effectively;
- Seek medical help promptly whenever a family member is sick;
- Control mosquito breeding sites;
- Use a combination of methods to eliminate mosquitoes and reduce man- mosquito contact.
CONCLUSION
You have now come to the end of this unit. In this unit, we learnt about the prevention and control of Malaria. We saw that for any prevention or control method to be effective, it should aim at breaking the man-vector contact cycle for a sustained period of time. Some of the methods we discussed included those that eliminate mosquito breeding, those that prevent mosquitoes from biting people and others such as early diagnosis and correct treatment. We also learnt that our role as health workers is to manage all Malaria cases properly and to pass on effective messages to the community.
You should now review the learning objectives outlined at the beginning of this unit. Have you achieved all of them? If not, go to the relevant section that you are not sure about and read it again. If you feel confident that you have achieved all the objectives, complete the attached Tutor Marked Assignment. Do not forget to do the practical activities outlined in our things to do.
| THINGS TO DO IN THIS UNIT
1. Instructions: A. ITNs/LLINs
2. In view of the above findings identify appropriate information, education and communication messages for your community. 3. Give these messages to the community. B. IRS (Only for those in epidemic prone areas)
4. Resources:
4. Feedback:
|
GLOSSARY
.
|
AMREF DIRECTORATE OF LEARNING SYSTEMS
Student Name __________________________________ StudentNumber:_________________________________ Student Postal Address: __________________________ __________________________
DISTANCE LEARNING COURSE ON MALARIA
Unit 8: Prevention and Control of Malaria
1. You as a health worker has been involved in management, control and prevention of Malaria. What are the five ways by which Malaria can be prevented? …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… 2. You are a manager of the NMCP. Vector control is one of the intervention measures in the National Malaria Strategy for malaria control. What criteria will you use to justify the choice of vector control?
3.What are the most cost effective methods of vector control in: •Unstable/Epidemic prone areas: ……………………………………………………………………………………… …………………………………………………………………………………… ……………………………………………………………………………………… •Endemic/Holoendemic areas …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… 4.List down six (6) indicators of vector control …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… 5.A health worker visited his community and found out that they were using untreated nets (UTNs), He however insisted that they should use insecticide treated nets (ITNs/LLINs). (a Give reasons why the health worker insisted on the use of ITNs/LLINs and not UTNs. …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… (b How can ITNs/LLINs be used effectively? …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… 6.After a year the HW visited the same community. He enquired whether the ITNs had been re-treated since his last visit. He was informed of the shortage of treatment kits and the community’s inability to afford them. Name the new net technology for malaria control ……………………………………………………………………………………… …………………………………………………………………………………… 7.List down the sources of ITNs/LLINs …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… ……………………………………………………………………………………
8.How would you as a health worker help the community to control and prevent Malaria? ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… 9.What is Indoor Residual Spray (IRS)? ……………………………………………………………………………………… ………………………………………………………………………………………
10. Name the equipments recommended for IRS …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… 11. Give 4 reasons for cleaning a spray pump after every day’s work …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… ……………………………………………………………………………
………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… b) Why is mass chemoprophylaxis discouraged? …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… c) List down the drugs commonly used for chemoprophylaxis in (4a) above. …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… …………………………………………………………………………… Congratulations! You have come to the end of this assignment. Post it or bring it in person to AMREF. If you have experienced any problems in this unit or assignment, please write to us. Your tutor will be happy to give you relevant responses to enable you cope with the course. Time spent doing the assignment: Hours …………………. Minutes …………..
|