Lesson 8: Anaemia
Contents
UNIT 8: ANAEMIA
INTRODUCTION:
Welcome to Unit 8 of this course which deals with anaemia. As you may well know, anaemia is a major source of lowered resistance to illness especially among children in this country. As a result, anaemia contributes to a reasonably high percentage of deaths in children. In this Unit, we shall, therefore look at the major causes of anaemia, its management and how we can prevent it.
Let start by reviewing our objectives for this unit.
|
By the end of this unit you should be able to:
|
8.1: DEFINITION OF ANAEMIA
|
The word anaemia is a Latin word meaning "no blood." It describes a condition where there is lack of heam in the blood. Heam is the oxygen carrying and iron-containing molecule. This is attached to a protein called globin to form haemoglobin (Hb), which is contained in the red blood cells. This haemoglobin is responsible for the red colour of the blood. What is anaemia? It is important that you understand what anaemia is. Anaemia is not a diagnosis. It is a condition whereby there is a reduction in number of red blood cells (RBCs) in the body. |
Depending on the cause, anaemia in children is subdivided into three groups:
- Diminished production of RBCs (a plastic anaemia and nutritional anaemias)
- Blood loss (haemorrhagic anaemia)
- Excessive breakdown of RBCs (haemolytic anaemia)
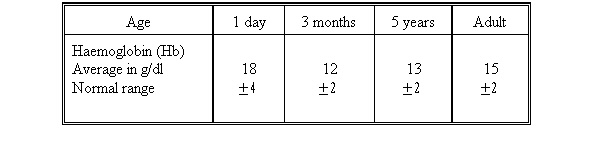
Haemoglobin or Hb is measured in grams per decilitre (g/dl) of blood with 11 g/dl or 70% as the lower normal in children. In a newborn, the lower limit is 14g/dl. This makes anaemia a common symptom. In fact, it is so common that slight anaemia (8 - 10 g/dl) may fail to attract your attention.
However, it should be noted that even slight anaemia is important because it weakens a child's resistance to infections, such as pneumonia.
Table 8.1: Normal Hb Levels in Children and Adults.
8.2: CAUSES OF ANAEMIA
Anaemia is caused by a number of factors. Before you read on do the following activity. It should take you about 3 minutes to complete.
| 1
List 3 causes of anaemia in children.
|
Well done! I am sure your answers included the following causes.
- Improper formation of red blood cells in the bone marrow.
- A deficiency of iron or folic acid in the diet, which are required to form haemoglobin.
- Excessive loss of blood (haemorrhage)
- Premature destruction of the red blood cells, haemolysis.
Certain hereditary diseases may result in improper formation of red blood cells.
Let us look at each cause of anaemia in greater detail.
1) Diminished production of red blood cells.
This is a condition where there is lack of raw materials to make sufficient haemoglobin or red blood cells in which haemoglobin is carried. Examples of this type of anaemia are nutritional anaemias, which are due to a lack of nutrients in the diet, particularly iron and some vitamins like folic acid and B12 and protein.
Alternatively, there could be a failure to manufacture enough red blood cells in the bone marrow. This is called red-cell aplasia or hypoplasia. Aplastic or hypoplastic anaemias sometimes have no obvious cause. In some instances, toxins from within and outside the body cause these anaemias. Examples of external poisons are chemicals such as lead and certain drugs (sulphonamides and chloramphenical) or physical radiation. Those from within the body include chronic infections and illnesses such as nephritis and malignant tumours spreading throughout the bone marrow thus diminishing the bone marrow space.
2) Blood loss.
These include the heamorrhagic anaemias that may be acute or chronic. Newborn babies may lose blood through bleeding from the cord or due to birth injury, either inside the skull (subdural heamatoma) or outside the skull (cephaloheamatoma).
In older children, blood may be lost from accidental injuries, nose bleeding (epistaxis), gastric bleeding or bleeding after uvulectomy or circumcision.
Loss of blood may be chronic particularly, especially if it occurs in the gastro-intestinal tract due to peptic ulcers, hookworm disease, chronic dysentery and haemorrhoids. Hookworms are the biggest cause of gastrointestinal bleeding. The more the hookworms the more severe the loss of blood thus resulting in severe anaemia.
TAKE NOTE: Anaemia in a child can be due many causes.
Hereditary disorders called Haemophili which is rare in Kenya can be the cause of bleeding in boys even following small cuts and during circumcision.
3) Excessive breakdown of red blood cells.
These are called haemolytic anaemias that are due to damaged and destroyed red blood cells. There are three major ways by which red cells can be damaged or destroyed:
- Toxic substances can weaken the red blood cell membrane. These include drugs and chemical poisons;
- Circulating antibodies as in erythroblastosis and auto-immune haemolytic anaemia.
- Congenital abnormalities of the red cells as in hereditary spherocytosis, sickle cell disease and thalassaemia.
Now, compare your answers as you read the following discussion.
It is important to remember that anaemia in children is best corrected if the actual cause is established although it may not be easy.
When taking history, we should always find out the age of the child because it helps us rule out certain causes. For example, hookworm anaemia is rare in children under 1 year of age. In malaria areas, malaria anaemia is most common between the age of 3 months and five years. And sickle cell anaemia is not common in children under three months old.
In older children, find out about their walking and playing habits as well as the general sanitation of their environment. This is because their environment could expose them to hookworm infestation. You should also find out the type of foods the child eats after weaning may be lacking iron and folic acid or proteins and vitamins. Lastly, pain in the abdomen, arms and legs may signify sickle cell anaemia.
| REMEMBER! ANAEMIA IS A SIGN NOT A DIAGNOSIS. SO TREAT THE CAUSE |
8.3: CLINICAL FEATURES OF ANAEMIA
The main symptom of anaemia is tiredness, and this symptom is common to all varieties of anaemia. Loss of appetite and irritability may develop. There is an increased vulnerability to infection and breathlessness. Rapid pulse and oedema are seen only in the most severe cases of anaemia.
The symptoms are most obvious if a child develops anaemia due to sudden loss of blood (e.g. in severe bleeding), because the body has had no time to adjust to the sudden change. However, in chronic anaemia where the blood loss is gradual, low levels of Hb is tolerated because of the body is able to gradually adjust to the anaemia.
Physical signs are minimal, pallor often being the only sign. The assessment of this feature must be made from an examination of the mucous membranes. You should look for pallor in the conjunctiva, the lips, the gums, the tongue, and the palms and soles of the feet. This is often useful especially in babies and coloured children. Fast pulse and fast breathing are also common signs of anaemia.
| PALLOR MAY NOT BE OBVIOUS, SO MILD ANAEMIA IS OFTEN MISSED. |
In severe anaemia, children will also show signs of heart failure such as:
- Breathless at rest;
- Swelling of the ankles (oedema);
- Fluid in the base of the lungs (crepitations);
- Enlarged liver, which is usually soft, smooth and tender;
- Raised veins in the neck;
- Rapid heart rate (rapid pulse rate)
8.4 HOW TO DIAGNOSE ANAEMIA
The diagnosis of anaemia is aimed at determining the severity of anaemia and classifying the severity into mild, moderate and severe anaemia. This is based on clinical assessment. Look for pallor in the palms of the hands, soles of the feet, nail beds, mucous membranes in the mouth, the gums, the lips and the tongue. You should also assess the conjunctiva of the eyes for pallor. The dark colour of the skin prohibits the assessment of pallor in the African child’s skin.
- The severity of and confirmation of anaemia is determined using laboratory investigations. Here the parameters most used are the haemoglobin (Hb) and haematocrit levels. Table 8.2. below indicates Hb lower limits in various individuals. The level of severity of anaemia (i.e. is mild, moderate and severe) is determined by how depressed the haemoglobin is from the normal level.
Table 8.2: Hb Lower Limits of Normal Range (below which patient is anaemic)
| Age | heHaemoglobin g/100 mls |
|---|---|
| Infants under 6 months | 11.0 |
| Children 6 months to 11 yrs | 11.0 |
| Adolescents | 12.0 |
| Pregnant women | 10.0 |
The severity of anaemia is classified as follows:
- mild anaemia = 5 – 7 g/100mls
- moderate anaemia = 7 – 9 g/100mls
- severe anaemia = less than 5g/100mls
| YOU CAN ONLY DIAGNOSE MILD ANAEMIA BY MEASURING THE HAEMOGLOBIN AND HAEMATOCRIT LEVELS. |
How to Assess for Pallor?
It is important that we know how to assess and classify anaemia. When examining a child for pallor, pull down the lower lip or one of the eyelids. If the child is older, ask him/her to put out the tongue. Look at the palms of the hands. Are all these parts paler than normal?
If you examine many children you will learn what a normal tongue, conjuctiva or palm looks like. You can diagnose moderate or severe anaemia like this.
We shall now describe conditions or diseases which cause anaemia.
8.5. CONDITIONS WHICH CAUSE ANAEMIA
8.5.1: Iron Deficiency Anaemia
Iron deficiency anaemia is a common condition worldwide but most prevalent in the developing countries. Iron is a most abundant micronutrient occurring in a variety of foods yet its deficiency occurs with far reaching public health consequences. As health workers, we need to control and prevent this condition in order to avert these bad consequences.
Role of iron in Formation of Haemoglobin
As we mentioned earlier, in this Unit, iron plays an important part in the formation of haemoglobin. It plays a particular role in the formation of the haem part, while the globin part is contributed by protein, thus forming haemoglobin. Haemoglobin plays the essential role of carrying oxygen from the lungs to various body tissues. When iron is deficient it means that the haemoglobin formed is not enough, hence there is insufficient transportation of oxygen from the lungs to the tissues. In addition, haemoglobin gives the red colour of the blood. When enough haemoglobin is not formed, there is pallor, which is seen and can be detected in the tissues as described earlier.
Sources of Iron
Before you read on, do the activity below. It should take you 5 minutes to complete.
Now check if the foods you listed fall under the ones listed below.
The iron needed by the body comes from the diet, mainly from the following sources:
- Leafy green vegetables
- Meat – beef, fish and poultry
- Cereals – sorghum, and millet
- Breast milk
Causes of Iron Deficiency Anaemia
Iron exists in the body as:
- Haemoglobin
- Body tissue iron (haemoglobin)
- Transit iron transferring
In iron deficiency anaemia, the body iron stores are depleted first, followed by reduction in transport iron and finally reduction of haemoglobin. These occur when there is reduced dietary intake of iron. This means that the child is not being offered the following:
- Adequate breast milk
- cereals
- meat
Unfortunately cereals, which may provide iron, also have a substance, which lowers absorption of iron thus making dietary iron not to become available to the body.
Breast milk is a good source of iron during infancy. The iron in breast milk is easily absorbed and utilized by the child. However, cow’s milk and fortified formula milk do not have adequate iron.
Common infections which are prevalent in the children precipitate iron deficiency. Although the main mechanisms are unknown, the following infections are suspected to precipitate iron deficiency:
- Infections which reduce appetite therefore food intake;
- Infections which may reduce iron absorption;
- Infections which cause iron to be lost from the diet through vomiting and diarrhoea;
- Infections that depress the bone marrow functions formation of haemoglobin;
- Infection that divert iron from the bone marrow and cause it to be deposited in other body tissue.
| ANAEMIA PREDISPOSES TO INFECTION AND INFECTION IN TURN CAUSES ANAEMIA, THUS SETTING UP A VICIOUS CYCLE |
The other causes of iron deficiency anaemia include blood loss due to any bleeding disorder. However, hookworm infestations are the major causes of iron deficiency anaemia. You will learn more about hookworm infestations in Unit 15 on Helminthiasis.
There are also factors surrounding pregnancy and delivery that can predispose an infant to iron deficiency anaemia. Ordinarily a foetus is a very successful parasite of the mother’s iron during pregnancy, particularly during the third trimester. However, if the mother has iron deficient mother the newborn baby may not have acquired enough iron from the mother during the third trimester. Such a baby will develop iron deficiency anaemia during infancy. Also a child born before term (preterm) may not have acquired enough iron from the mother during the third trimester. Such a preterm infant may develop iron deficiency anaemia as they grow rapidly during infancy.
Finally, in addition to the causes we have discussed above, the deficiency of other micronutrients can cause iron deficiency anaemia. For instance, the deficiency of other micronutrients such as of vitamin A, vitamin c, vitamin b12 and folic acid, may decrease the initialization of iron in the formation of haemoglobin and thus lead to iron deficiency anaemia.
Clinical Features of Iron Deficiency
The main clinical features of iron deficiency anaemia are described under section 8.3 above. In addition there is wasting, spade-shaped and easily breakable nails and a smooth tongue.
In severe case with Hb below 5g/dl there may be cardiac failure with tachycardia (rapid heart rate above 160/minute), oedema of the feet and an enlarged tender liver
Effects of Iron Deficiency Anaemia
Iron deficiency anaemia has far reaching consequences. In its severe form, it impairs physical growth leading into wasting whereby the individual child becomes thin. It also lowers immunity thus leading or contributing to infections and the vicious cycle we described above. On brain development iron deficiency anaemia in its severe form impairs learning due to reduced attention span thus leading into lack of concentration and poor academic performance and achievement.
Achievement of Iron Deficiency Anaemia Diagnosis
The diagnosis of iron deficiency anaemia follows three levels:
- Detailed history,
- Clinical assessment and
- Laboratory investigations.
These three levels not only help to determine the underlying causes of iron deficiency anaemia as we discussed earlier but also how to diagnose anaemia.
History Talking
In history talking you should make sure you go through in details all the possible causes we discussed earlier. Enquire about the child’s diet to check if it is rich enough in iron and how long the child was breastfed. Look for evidence of blood loss through bleeding and find out the sanitary conditions where the child lives to evaluate whether hookworm infestation could be the cause. In addition, you should determine the nutritional status of the mother during pregnancy. Establish if the child was born premature; whether the child has developed normally physically and in activities, and whether the child has suffered from any infections. Remember to enquire about the presence of those clinical features related to anaemia which we discussed earlier.
Management
The treatment of iron deficiency anaemia consists of
- Correcting the anaemia ;
- Treating the causes of iron deficiency;
- Treating any adverse effects of anaemia;
Iron deficiency is corrected by
- Administering iron in the form of ferrous sulphate
- Giving ferrous sulphate orally and checking Hb every two weeks to monitor the response.
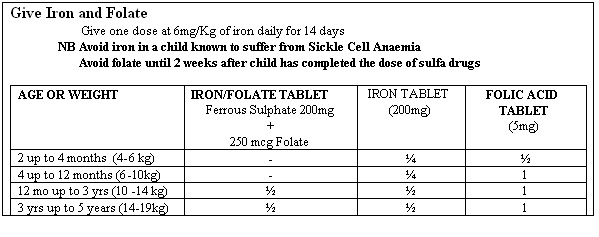
- Giving iron and folic acid according to the guidelines in Table 8.3 from the Ministry of Health.
Table 8.3: Management of Iron Deficiency: Source MOH IMCI guidelines
- Continuing with ferrous sulphate and folic acid for a duration of 2-6 weeks after Hb has come to normal. This helps in replenishing iron stores in the tissues;
- Administering Vitamin C to help in increasing iron absorption;
- Correcting the diet and treating infections such as hookworms infestation.
In severe anaemia with cardiac failure a blood transfusion can be done. However, remember that a blood transfusion should only be carried out in a health facility where proper clinical assessment can be made and where procedures for collecting, grouping, cross-matching, screening and storing blood can be carried out.
Prevention
- Treat all pregnant mothers who have iron deficiency;
- Give iron supplement to children born prematurely;
- Encourage use of breastfeeding exclusively for six months;
- At six months of age, children should be given leafy vegetables and cereals;
- The community should use latrines to prevent hookworms infestations;
- Where possible meat should be given to children as it has high iron content;
- Follow up anaemia cases every 1-2 weeks until the haemoglobin level is normal.
Continue to give iron and folate supplements for a further 3-6 months. The haemoglobin level should rise roughly 1g/dl every 7-10 days, although children recover faster.
FAILURE TO RESPOND MAY BE DUE TO SEVERAL CAUSES:
|
If the child fails to respond to treatment, the child should be referred for better management, which may involve blood transfusion if the symptoms are very severe.
In case of other serious causes of anaemia such as leukaemia, sickle cell disease or bleeding tendencies, specific diagnosis for each should be followed and action taken appropriately.
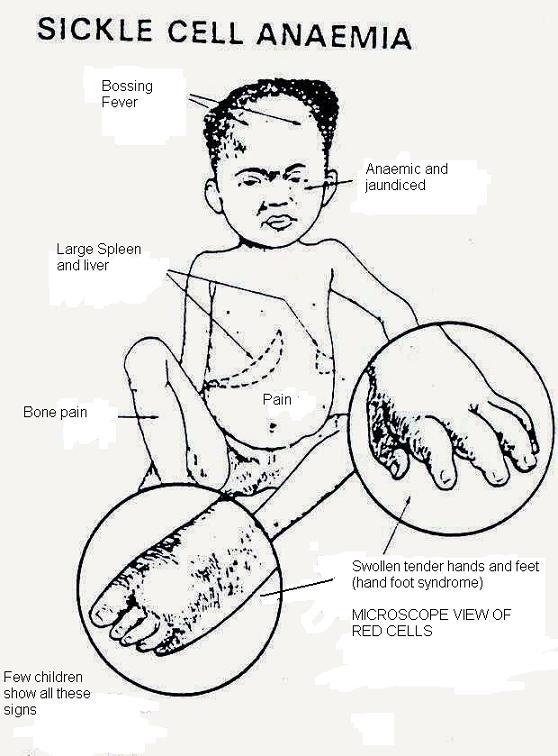
8.5.2 Sickle Cell Anaemia
This is an inherited disease in which the haemoglobin is abnormal. Normal haemoglobin is called haemoglobin A. Abnormal haemoglobin is called haemoglobin S. The red cells with abnormal haemoglobin form sickle or crescent shapes when they are de-oxygenated (i.e. when oxygen is reduced). Because of this shape, sickled red blood cells can not squeeze through small blood vessels as easily as the normal cells. They thus block the blood vessels and stop the oxygen from getting through to where it is needed. The bone marrow also becomes hyperactive trying to keep up with the increased breakdown of blood cells which occurs.
Very often the clinical features of the disease are provoked by an infection. This may be due to the inability of the bone marrow to cope with the increased breakdown of the cells (haemolysis).
There are many forms of sickle cell disease, depending on the type of haemoglobin contained in the child's blood. Some children are born with haemoglobin S and A. This means that the child got haemoglobin S from one parent carrier and A from the other parent. In such a child, half the red blood cells will have haemoglobin S while the other half will have haemoglobin A. The haemoglobin in the blood will therefore be a mixture of A and S, and we therefore say that the child is A-S. Such a child has sickle cell trait and is a carrier of abnormal haemoglobin S.
However, if the child inherits S from each of the parent who are carriers (AS), the child ends up with haemoglobin SS. Such a child will get severe disease called sickle cell anaemia.
| NOTE: NORMAL INDIVIDUALS HAVE HAEMOGLOBIN AA. |
Clinical Features:
Sickle cell anaemia may present with a fever, anaemia, jaundice, pain in the arms or legs, abdominal pain, abnormal childhood growth or as dactylitis (inflammation of fingers or toe). An SS baby is usually well until about 3 to 6 months old. He or she then has attacks of fever, mild jaundice and anaemia. The liver and spleen become enlarged. At an older age, the spleen may become small again. Sometimes a young child has warm, swollen, painful hands or feet, fingers or toes. This is caused by lesions called "dactylitis." The child may have dactylitis of the hands and feet at the same time. We call this "hand-feet syndrome". This is most common in the first year of life. These lesions last one to two weeks and then heal themselves.
At about two years of age, bony swellings start to form at corners of the skull (occipital and temporal regions). This is called "bossing." Dactylitis and bossing are typical features of sickle cell Anaemia and are very helpful for making a diagnosis.
| OSTEOMYELITIS IS COMMON IN CHILDREN WITH SICKLE CELL DISEASE |
Sometimes the child's disease gets much worse and we call this a “crisis". There are several kinds of crises.
- Pain in the arms and legs because the blood vessels in the bones are blocked by abnormal blood red blood cell;
- Swollen liver and spleen plus abdominal pain. This may be so severe that you may think the child has an acute surgical abdomen. There may also be tenderness and guarding in the abdomen. The child may suddenly become very anaemic because many red blood cells are damaged or because the bone marrow stops making new red blood cells. In such a circumstance, the child should be transfused with blood.
- Sudden haemolysis (haemolytic crisis) or a breakdown of red blood cells. A haemolytic crisis causes severe anaemia with jaundice.
Diagnosis:
Diagnosis of sickle cell anaemia depends on:
- The clinical signs of hand-foot syndrome, recurrent anaemia with jaundice (haemolytic crisis), abdominal pain and presence of bossing of the skull;
- The history of other children in the family who have the above signs or who die of such clinical features;
- Laboratory test: one which looks for sickle cells on blood smear of the patients and the other called haemoglobin electrophoresis. The latter separates the haemoglobin thus showing the presence of haemoglobin SS that confirms the presence of the disease.
- Estimation of Haemoglobin level to determine the severity of the anaemia.
Management
In the management of sickle cell the following measures can be taken:
- Managing a crisis when it occurs. The pain and swelling of hand-foot syndrome should be treated with paracetamol and in severe cases codeine or pethidine;
- Daily prophylaxis against malaria and daily folic acid should be given;.
- Infections such as pneumonia, malaria or others should be diagnosed early and treated appropriately. If you are not sure refer to next level with a letter according to IMCI strategy;
- Severe anaemia should be treated by blood transfusion in a hospital according to IMCI strategy. Hence determined the severity, explain to the mother and refer to the next level with a referral letter.
Educating the Parents:
The parents and caretakers of a “sickler” in the community should be educated in the care of the disease. It is important that they are told about:
- Hand foot syndrome (crisis);
- Early symptoms of an haemolytic crisis: they should look out for pallor and jaundies;
- How to correct any fluid loss quickly in diarrhoeal disease using ORS;
- How to treat pain with paracetamol or codeine;
- To bring the child to hospital or health centre early if they see signs of malaria or other infections;
- To attend the clinic for sickle cell anaemia regularly where they are given anti-malarials and folic acid;
- That when there is severe anaemia the child needs blood transfusion;
- To be warned that SS children die from crises infections and severe anaemia and thus they should ensure that they are managed promptly.
In acute sickle cell disease, especially in infants, blood transfusion is an emergency and therefore such a child should be admitted.
| THERE IS NO CURE FOR SICKLE CELL DISEASE. THE BEST WAY TO HELP THEM IS TO KEEP THEM ON THE ROAD TO HEALTH AND PREVENT INFECTIONS. |
I hope you now understand how to diagnose and manage sickle cell disease. Next, let us look Leukaemia, another condition which causes anaemia.
10.5 Leukaemia
Leukaemia is described as a cancer of the blood or bone marrow which is characterised by production of abnormal blood cells, usually white blood cells or leukocytes.
Such abnormal cells can occur in the bone marrow or in the blood. These cells are both abnormal in quality and quantity such that they fail to perform their normal duties of fighting germs. Thus a child with leukaemia has a tendency to get recurrent infections.
The abnormal cells also replace the other cells usually produced in the bone marrow, such as red blood cells and platelets. The lack of red blood cells results in anaemia and the lack of platelets results in bleeding tendencies. These abnormal cells may also occur in the liver spleen and lymph glands, causing their enlargement.
THE SPECIFIC CAUSE OF LEUKAEMIA IS NOT KNOWN
Clinical Features
The patient usually presents with non-specific "flu-like" symptoms or vague malaise and tiredness. There may be marked anaemia, and enlarged spleen and liver, particularly when the disease is advanced. Bleeding tendencies and other infections may manifest, such as mouth ulcers, herpes labialis and sorethroat. Bleeding gums, purpura and epistaxis may also occur.
Management
All children suspected to have leukaemia should be sent to hospital for a bone marrow examination and further investigations. Leukaemia is treated with specific anticancerous drugs. Such drugs are very expensive and are not available in health facilities lower than a referral hospital. It is important to note that the majority of children who have been treated and have not had a relapse within five years can be expected to be cured. That is why it is very important to diagnose leukaemia correctly and refer to a hospital that is able to deal with the disease as soon as possible.
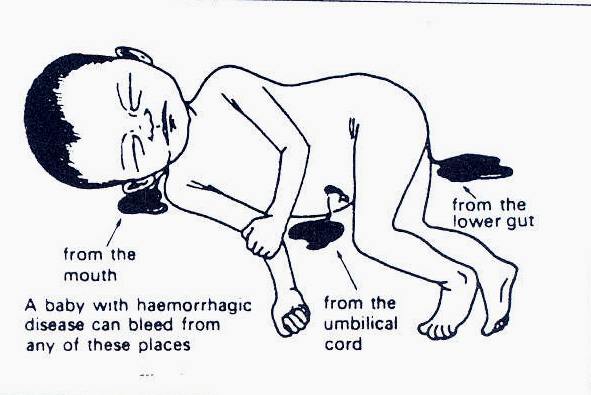
10.6 Bleeding Tendency
Bleeding tendency or haemorrhagic disease is a condition in which blood is lost from any part of the body, with or without cuts. It is common in newborn babies, although older children may develop a bleeding tendency such as nose bleeding and blood in vomitus and faeces. In newborn babies, blood may appear from the mouth, umbilical cord and the lower gut.
There is no specific cause of bleeding tendency, although it can be related to a deficiency of factors normally involved in the clotting of blood and the sealing-off of injured vessels. Common factors associated with bleeding include:
- Lack of thrombocytes - this can occur temporarily after infections in infancy but is also seen in leukaemia and other blood diseases;
- Lack of "clotting factors" such as prothrombin;
- Abnormal vessels - these may occur in scurvy cases. Abnormal blood vessels are also common in premature infants whose blood vessels are so delicate that they can be damaged during a difficult delivery and rough handling.
Management
Bleeding tendency is managed according to the identified or suspected cause.
Newborns: Any bleeding in the newborn should be treated with 1 mg of vitamin K intramuscularly. This can be repeated once. Old blood may continue to ooze from the stomach or stools but fresh bleeding should stop within 6 hrs. If not, refer.
| DO NOT GIVE MORE THAN 2 mg of VITAMIN K. IT DOES NOT HELP AND MAY CAUSE JAUNDICE |
Children with general bleeding tendency or continuous bleeding from one place only should be referred to hospital for investigations and diagnosis;
Nose bleeding in older children can be stopped by seating the child quietly. The child should bend forward, and then pinch his/her nose. He/she should also bite on something soft such as cork, cotton ball or bandage so that he/she cannot swallow. If the bleeding does not stop in an hour, refer to the hospital.
Prevention
In order to prevent bleeding of the newborn give all babies an injection of vitamin K at birth. If you cannot give this to all babies, give to the very smallest babies and to those babies who have had a difficult birth.
Having looked at conditions that cause anaemia, let us now proceed to learn how we can prevent this condition.
8.6: PREVENTION OF ANAEMIA IN THE COMMUNITY
From our discussion so far we hope that you now know that anaemia is a sign and not a diagnosis. We also hope that you now understand that anaemia is caused by various factors and underlying causes. However, with correct diagnosis and investigation, anaemia can be traced to its root cause or causes in an individual child.
Likewise, the common causes of anaemia in any given community can be established through studies. You can do this for your community over a period of time by proper record keeping and analysis of all anaemia cases you see at your health facility. Wherever possible, a one time study could be done on the existing anaemia cases in the community.
Generally, prevention of anaemia in a community can be carried out through health education in order to boost their awareness of its causes and possible solutions.
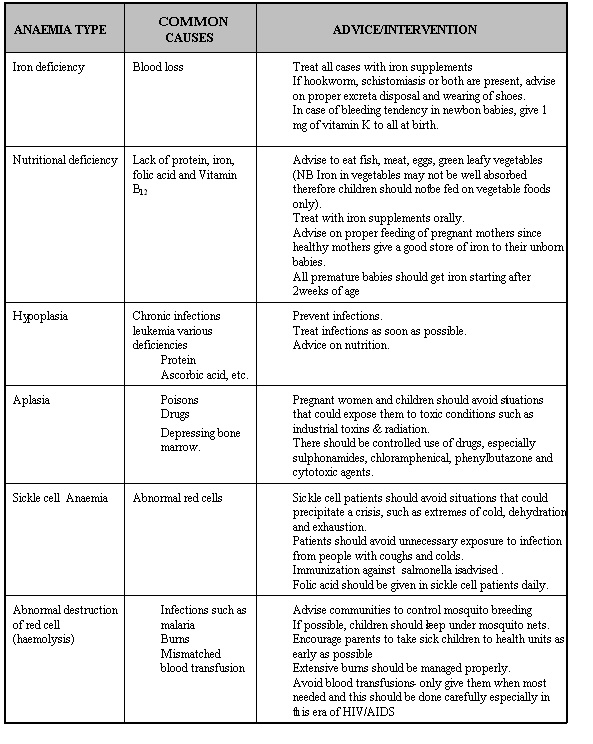
You can use the information in Table 8.3 to create health education opportunities for your community.
Table 8.4: Types of Anaemia, Causes and Interventions
SUMMARY
You have now come to the end of this unit. In this unit we have discussed anaemia in children, its common causes, clinical signs and symptoms, risk factors and how you can to prevent and control it in your community. It is important to note that the causes of anaemia are not the same everywhere. For example, while iron and folic acid deficiencies are common in most districts, malaria and sickle cell anaemia is only found in a few districts. So depending on the community you serve, you will need to care for anaemic children bearing in mind the prevailing conditions and factors that may predispose children there to anaemia.. If you are not able to diagnose the cause of a child’s anaemia, remember to refer. Always do your best to save lives.
Best wishes.
|
AMREF DIRECTORATE OF LEARNING SYTEMS DISTANCE EDUCATION PROGRAMME TUTOR MARKED ASSIGNMENT
Name:__________________________________________ Address_________________________________________ _____________________________________________
CHILD HEALTH COURSE TUTOR MARKED ASSIGNMENT
Answer all the questions and send the completed assignment for marking. It will be returned to you with comments together with the next units.
1.List the main symptoms common to all varieties of: a) Moderate anaemia b) Severe anaemia
3. What is sickle cell Anaemia?
4. What factors cause bleeding tendency?
5.A 7 year old boy is brought to your clinic because of bleeding from the gums and nose for a period of two months. You examine him and find him to be pale with enlargement of spleen and lymph nodes. a) What would be the likely cause of this condition?
c) What advice would you give concerning its management?
|