Lesson 7: Nutrition
UNIT 7: NUTRITION
INTRODUCTION
Welcome to Unit 7 on Nutrition. In the last unit we discussed health education, promotion and counselling. We learned that counselling and health education can influence positive behaviour change, resulting in better health and fewer illnesses among our children.
Good nutrition is one of the factors that can help to promote better health and to prevent disease, illness and low birth weight in newborn babies. Similarly, good nutrition is an important factor in helping a child achieve normal growth and development.
In this unit we will discuss nutrition. We feel that this is an opportune time to discuss nutrition because good nutrition has far reaching consequences on everybody, but more so on children. This is because their bodies are growing rapidly. Good nutrition protects children from many illnesses and ensures that they attain their full potential. We hope that in subsequent units, especially in the unit where we discuss common conditions of childhood, you will be able to see the relationship between poor nutrition and ill health.
The relationship between food, nutrition and health has long been recognised. In most parts of the country we are lucky to have plenty of natural resources, favourable climate and adequate food supply. Despite the apparent abundance of food, however, malnutrition and under-nutrition still exist and are now a major public health problem, especially among children and women of childbearing age.
Malnutrition results from or is the end result of diverse and interrelated factors that may operate singly or in combination. The immediate factors that affect nutrition are food availability and intake, and the state of health of the individual or community. These factors interact and are also affected by socio-cultural, political economic and environmental factors. Collectively, all these factors affect the dietary intake and health status of the population.
For too long, nutrition issues have not been adequately handled. This is because there has been a lack of appropriate information about the magnitude of the problem. There has also been inadequate information about the relationship between nutritional status and socio-economic development. We have tended to only concentrate on treatment and rehabilitation of the very severely malnourished. Finally, the relevant sectors that deal with nutrition have lacked a coordinated approach to nutritional problems.
Adequate nutrition is particularly important during pregnancy and early childhood. During pregnancy the mother must eat enough to supply the nutritional needs of two people – herself and the developing foetus. If a pregnant women fails to take in enough of the right kinds of foods, both she and the baby inside her will suffer. She may become weak and anaemic and the baby may have a low birth weight and a reduced chance of survival.
While a woman is breastfeeding, she needs extra protein and calories to keep her own body strong and to produce enough milk for the baby. Meanwhile, small children require a lot of food because they grow quickly and use a lot of energy in their activities.
In this unit we shall look at how nutrition is a major determinant of health and growth of children.
|
By the time you have completed this unit, you should be able to:
|
7.1 NUTRITION: A DEFINITION
Before beginning this unit, do the following activity:
| 1
Nutrition is a word you have been using now and again in your daily work. How do you define it? Write your definition in the space provided. ………………………………………………………………………………………………… ………………………………………………………………………………………………… ………………………………………………………………………………………………… ………………………………………………………………………………………………… …………………………………………………………
|
|
The World Health Organisation (WHO) defines nutrition as "A process where living organisms utilise food nutrients for the maintenance of life, maturation, and normal functioning of organs and tissues and the production of energy.” |
Having defined the word nutrition, let us discuss foods commonly eaten in our community and their nutrients.
7.2: FOODS AND THEIR NUTRIENTS.
It may sound a little strange or even silly to ask the question “What is food?” But think about it. Can you define food? One possible definition is as follows: Food is any substance that contains a nutrient which, when eaten, nourishes the body.
Is the list of foods you have made exhaustive? If it is, let's ask ourselves "why do we eat? Of course we eat to stop feeling hungry, but this is only part of the answer. The more important reason is that we eat because our bodies need food to keep alive and stay healthy.
Hunger is the message that tells us our bodies need more food. This is not a very good message because it tells us to eat any food, and not food with particular nutrients that we may need such as proteins, carbohydrates etc. In this section we are going to see what nutrients are contained in our food.
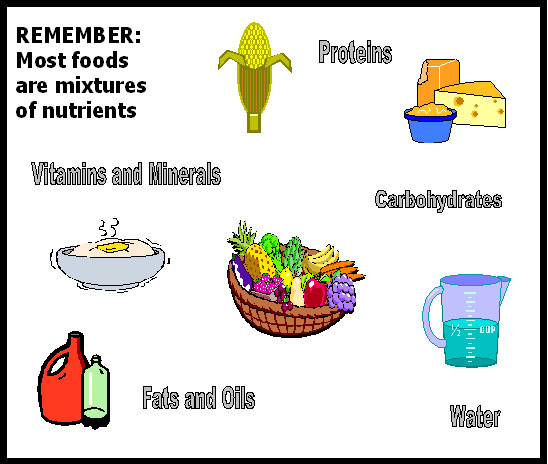
The body uses nutrients in different ways. It is useful to classify foods into groups according to their nutrients:
- Proteins
Carbohydrates
- Fats and oils
- Vitamins
- Minerals
- Water and fibre
Although most foods are mixtures of nutrients, many of them contain a lot of one nutrient and a little of the other nutrients. Foods are often grouped according to the nutrient that they contain in abundance. Foods that contain a lot of protein are called body-building foods because protein is the most important nutrient in them. Foods that contain a lot of fat or carbohydrates and perhaps only a little protein are called energy foods. Foods in which the most important nutrients are vitamins or minerals are called protective foods.
You are already wondering why we have listed water and fibre as nutrients. This is because they play very essential roles in the body. For example, the importance of fibre lies in keeping up the bulk of the contents of the intestinal tract and binding them in the large intestine into a soft faecal mass that can be properly expelled. So, water and fibre are known as non-foods.
| 3
Now that you know about nutrients, go back to the list you made of common foods in your community. Categorise the foods you have listed.
|
If children are to stay healthy they must eat a mixed diet of different foods which contain the right amount of nutrients. Let us now discuss each of the above nutrients in detail.
1) PROTEINS:
Proteins are known as body building foods because they build and repair the body. When a child is born, the body, and especially the brain, goes on growing. The cells of a child's body also wear out, so a child needs protein for repair as well as for growth. In order for a child to grow fast she/he needs plenty of protein food. In the first six months of life the baby gets all the protein from the mother's milk. The baby should have exclusive breast feeding from the age of 6 months onwards the mother introduces other foods to the baby's diet. In these foods the mother always adds some protein. For example, the mother adds milk to the porridge, and milk is a protein food.
Pregnant women need protein nutrients to build their bodies an that of the babies and placentas, and to make extra blood and storage of fat. Breastfeeding mothers need these nutrients to make breast milk.
Now that we know why we need protein, the next thing to think about is the kind of food that contains it. Proteins are derived from two sources: plant and animal origin.
The plant foods that give us protein are:
- Legumes: Soya, all types of beans, groundnuts, all types of peas, ndengu etc.
- Cereals: such as maize, millet, sorghum, and rice (have very little proteins).
The animal foods that give us protein are:
- Milk, especially mother's milk.
- Fish of all kinds - whether fresh or dried.
- Eggs.
- Meat of all kinds.
- Blood, liver.
- Chicken.
- Insects, including grasshoppers, locusts, white ants, etc.
All animal foods contain more protein than plants and are usually better sources of body building foods. Even though plant proteins are usually not as good for body-building as animal proteins, they can become better by mixing them. We shall also see that they are very important because they are cheaper and much easier to grow.
| 4
Where do most people in your area get their protein? …………………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………………… …………………………………………………………………………… Why do they eat these particular kinds of protein? ……………………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………………… ……………………………………………………………………
|
2) CARBOHYDRATES:
Carbohydrates are referred to as energy giving foods. They provide the energy in the form of calories the body needs for work and other functions.
Children need energy for growing. A pregnant mother needs energy to give to her child who is growing in her womb. A nursing mother needs energy to put into the milk to give to the child at her breast. Children of all ages need energy with which to grow, to run and play and to walk to school.
We have already seen that most foods contain a mixture of nutrients. Further, some foods contain higher concentration of one nutrient, for example meat has more protein than it has other nutrients, and that is why it is classified as a body building protein food.
Similarly, energy foods have a higher concentration of carbohydrates compared to other nutrients. Take the example of maize. Although maize contains a little protein, its major nutrient is carbohydrate. However, even though protein is not an energy food, the body can convert it into energy if need arises. For example, if you eat too much protein, the excess is converted into energy. Also, if you do not eat any energy foods, again the body converts the protein into energy.
Sources of carbohydrates are:
- Sugar
- Wheat flour from which chapati, bread and biscuits are made.
- Cereals maize from which ugali is made, rice, millet, sorghum etc.
- Sweet potatoes
- Plantains (Matooke)
- Irish potatoes
- Yams
- Cassava
3) FATS AND OILS:
Fats and oils are a concentrated source of calories and so are important nutrients for young children who cannot eat large meals. Fats also make meals more tasty and satisfying.
Fat is present beneath the skin as an insulation against cold and it forms a supporting tissue for many organs such as the heart and intestines. It must be remembered that the fat in the body is not necessarily derived from fat that has been eaten. Excess calories from a carbohydrate source such as maize, cassava, or banana can be converted into fat in the human body.
Sources of fats and oils
- Palm oil, simsim oil, groundnut oil.
- Lard, cooking fat, fat from animals.
- Butter, margarine.
Fats and oils are the best energy foods there are, but they are also so expensive that many families cannot afford them.
It is important to remember that carbohydrates and fats provide mainly energy. They cannot be used for bodybuilding because they contain no amino acids. For example, if a child is fed only on almost pure carbohydrate foods like cassava, he will not grow. This is because the cassava will provide give the child energy to run about and play, but will not build and repair her/his body.
Good staple food such as wheat, maize, rice and millet contain about 8% protein and are thus much better than staples like bananas and cassava which only contain about 1% of protein. People who have high protein food, as staples are usually better nourished than those who have low protein foods as staples. For example, Masai have milk as the staple food as compared to the Luo whose staple is ugali.
4) VITAMINS:
Vitamins are organic substances present in minute amounts in foodstuffs and are necessary for metabolism. Vitamins are also called protective foods. They are grouped together not because they are chemically related or have similar physiological functions, but because, as their name implies, they are a vital factor in the diet.
In our society the most important vitamins to know about are Vitamins A, B, C and D. If people eat too little of any of them, they get certain diseases.
Vitamin A and its deficiencies will be explained more in the section on common nutritional problems. Vitamin B is another important vitamin. There are various types of Vitamin B, such as Vitamin B1 (thiamine or aneurine), Vitamin B2, (Riboflavin), and Vitamin B12, (cyanocobalmim), nicotinic acid and folic acid. If a person does not have enough nicotinic acid in her/his food, she/he will get a disease called pellagra. Pellagra is common in places where people eat only maize. It is also common in adults who drink a lot of beer and do not eat enough food. Patients with pellagra have diarrhoea and bad skin. They may also go mad. (Three Ds i.e. Diarrhoea, Dermatitis and Dementia)
Folate is one of the B vitamins. People need folate to make healthy red blood cells, to help some body processes to happen, and for growth Lack of folate is a common cause of anaemia among pregnant women, people who have malaria often and sometimes, young children. Deficiency of Vitamin B2 (riboflavin) causes angular stomatitis, sore cracked lips, and glossitis. Lack of Vitamin B1 (thiamine or anevrine) is usually associated with polished rice diet. The disease is called beriberi. Important sources are dark green leafy vegetables, livers, kidneys, whole meal cereals, legumes, citrus fruit and fish.
Vitamin C is found in many fruits such as oranges, lemons, guavas, and tangerines and in green vegetables. If one does not have enough vitamin C she/he gets a disease called scurvy. Blood capillaries become weak and break easily. The gums swell up and bleed. Scurvy is common in people who cannot grow or afford fresh fruits and vegetables for long periods. It is also common in old people who find difficulty buying or eating fruits and vegetables.
Vitamin D is important in the formation of bones in the body it helps calcium to be deposited in the growing bones of the children. Deficiency of the Vitamin causes rickets, a disease of the growing bones. The clinical features of rickets are many. They include delay in teething and delay in closure of the anterior fontanelle. Children with rickets also have big heads referred to as bossing of the skull. The ribs have knobs where the cartilage is joined to the hard bone. The chest too gets deformed with caving in at the lower end. The lower ends of the long bones at the wrists and ankles tend to become enlarged. Generally the child with rickets is weak as the muscle has no much strength. Their abdomen is enlarged and the affected children become constipated. These children too have repeated attacks of pneumonia. The dietary sources of Vitamin D include milk and other dairy products as well as fish.
5) MINERALS: Minerals have a number of functions in the body. One of these is developing body tissues and for metabolic processes. The minerals that are of most importance in human nutrition are calcium, iron, iodine, and fluorine. Iron is discussed in Unit 10 Section 5 on Anaemia. Iodine is discussed under the common nutritional deficiencies.
Calcium is needed in the body to make bones. Pregnant and nursing mothers need calcium to make their child's bones. Many foods, especially milk, millet and dried fish contain calcium.
Fluorine is found in water and helps to build strong teeth. When there is no fluorine in the water, many people get cavities in their teeth. However, too much fluorine in the water causes brown patches in the teeth.
6) WATER AND FIBRE: Water is used in our daily life.
| 5
What is water? …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… …………………………………………………………………………………………………… Why is water important? ……………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………… ……………………………………………………………………………………………
|
Earlier in this section we said that water is a non-food. However, water is essential for life. We need water for a number of reason:
- For the body to make cells and fluids such as tears, digestive juices and breast milk.
- For the body to make sweat for cooling itself.
- For essential body processes - most take place in water.
- For keeping the lining of the mouth, gut, eyelids, lungs etc. wet and healthy.
- For the production of urine which carries waste from the body.
Fibre is composed of material that is not usually digested so that it passes through the gut nearly unchanged. Some of the foods rich in fibre are leafy vegetables and fruits.
7:3 FOOD PRODUCTION AND SECURITY
If a child is to grow s/he must eat enough of the right food. This food must come from somewhere. Foods like maize and groundnuts are grown in fields and gardens. Cows are milked and are later slaughtered for eating. Fish are caught in rivers and lakes. All these foods have to get to a child's body from the fields and gardens where they are grown.
As a health worker you play an important role in up lifting the nutritional status of your people. You have to make sure that you improve the quantity and quality of food eaten with the aim of ensuring an adequate diet at all times in every household.
In order to achieve this, you need to advise members of the community in the following areas.
- Increasing and improving food production.
- Improving food and crop storage.
- Improving food distribution.
- Improving food processing.
As you can see, most of those areas are the responsibility of extension agents from the agricultural livestock or fisheries departments. However if you want your nutritional programme to succeed, you will have to work hand in hand with them. You can involve extension agents by:
- Referring needy families to them.
- Telling them about families who need help.
- Inviting them to talk to groups at clinics, schools etc.
| 6
Think and write the answer to the following question: What do people in your community do in an attempt to increase food production? …………………………………………………………………………………………………………… …………………………………………………………………………………………………………… …………………………………………………………………………………………………………… ……………………………………………………………………………………………………………
|
There are many things that communities can do to increase and improve food production. As you read the following section, see whether your answers includes them.
To increase and improve food production a farmer needs to grow plenty of food as well as a wide variety of crops in order to meet the family's dietary requirements. In order to achieve this, you as the health worker, with the help of extension workers, need to advise farmers on the following:
- Farmers must observe good farming practices. They must dig the earth and sow good seeds at the right time and the right way. There must be enough rain and no insects must harm the crops while they are growing. This needs intervention of agricultural officer.
- Farmers must be healthy and strong to be able to work hard in the fields. A sick farmer who is down with malaria may delay in planting because he is too weak to clear his field. Similarly, a malnourished farmer may only plant cassava instead of maize because he doesn't have the energy to work hard. Thus you need to provide curative services, helping farmers to stay strong and healthy.
- They need to increase the production of plants that are good sources of protein. Every household should have enough beans, groundnuts, etc.
- They should increase and improve production of animal protein by:
- Better animal husbandry
- Increased poultry keeping.
- Increased and improved methods of catching and preserving fish.
- The construction of village and household fish pounds.
- Extensive use of small animals, especially pigeons and rabbits for food.
- People should increase vegetable and fruit production to ensure adequate intake of Vitamins C by:
- Encouraging backyard vegetable gardens.
- Allocating land for growing food in towns.
- Establishing school gardens, community gardens and orchards, etc.
IMPROVING FOOD DISTRIBUTION:
Food should be equitably distributed, not only between communities, but within families as well. More equitable distribution can be achieved by:
- Improving communication to ensure that excess stocks in one area reach another area short of that commodity.
- Better trading facilities, i.e. by more food markets and shops.
- Fair distribution within the family to ensure a fair share of protein-rich and other foods for children.
- Instituting mid day meals for day-school children, encouraging children to take food to school, supplying milk at school, improving meals at boarding schools.
- Making special foods available for young children.
- Encouraging better family budgeting.
IMPROVING FOOD STORAGE AND PROCESSING AND CROP PROTECTION:
People never eat a good percentage of all food produced. Instead, it gets spoiled by fungi or is eaten by insects, rats, mice, and other pests. Here you can involve an agricultural field worker to advise people on how to:
- Build better food stores.
- Control rats by trapping, poison, and rat-proofing grain stores.
- Control insects by use of insecticides, better food stores and use of airtight food containers.
- Control fungus and food rot by storage of food in as dry a state as possible and by use of better containers.
- Control birds, especially in millet, rice and wheat growing areas.
- Protective measures against monkeys, baboons, etc.
Proper food processing should include the following:
- Better methods of food preservation in the home, such as drying or smoking meats or fish.
- Preservation of fruits and vegetables.
- Better cooking, such as preparing special food for infants.
- Supply of properly processed milk products at reasonable cost.
- Iodisation of salt to prevent goitre.
- Fluoridation of community waters supply
As we mentioned earlier, some of the activities necessary to ensure food production and security need the involvement of an agricultural officer. However, as you are well aware, there are some communities that produce enough food with good variety, yet they have many children who suffer from malnutrition. This is where your direct involvement comes in. As a health worker there are several things you can do to make sure that once food is produced, it is properly eaten. These are:
- Providing good curative services. From your experience you know that when children are sick, e.g. with malaria, they can refuse to eat. Further, there are certain diseases, such as worm infestation, that stops the body from using food properly.
- If sick children are not treated in good time, their nutritional status can suffer and this can result in malnutrition.
- Take an opportunity within your community to give nutrition education in schools, clinics, wards, etc. You can do this through asking government and respected leaders to include the topic in their speeches.
- Distribute pamphlets and posters, and publicise nutrition facts through radio broadcasts, etc.
- Offer demonstrations of the preparation and cooking of food, especially food suitable for children. The health workers, community development workers or science teachers can do this at clinics or schools.
- Use a team approach through village committees.
- Encourage and carry out growth promotion monitoring of children in your community.
- Carry out preventive measures such as immunisations, etc.
- Conduct investigations and surveys to ascertain food hygiene. The survey should also ascertain the types and extent of malnutrition in the community. The results of these will enable you to give sound advice on remedial measures.
- Study local feeding practices and customs related to food and feeding.
- Take an active role in team activities designed to improve nutrition.
- Keep notes and records relating to nutrition.
- Encourage prolonged breastfeeding.
Having gone through this section of food production and security, you should now recognise that if children are going to eat enough of the right kind of food, the community must know how to increase and improve food production, distribution storage and processing. Proper methods of processing and preparation of food at home should be emphasised. When all this is done, you can be assured of a sound nutritional status of your community.
7.4: BREAST FEEDING AND WEANING
<kaltura-widget kalturaid='101380' size='L' align='R'/>
Breastfeeding is the process of feeding a child with milk from the mother's breast. A child can be breastfed exclusively, without the introduction of other foods or liquids, until he or she is 4 to 6 months of age. Then other foods can be added to the child's diet in addition to breast milk.
The Ministry of Health recognises the importance of breastfeeding for the healthy growth and development of infants. Therefore, the Ministry is committed to the promotion, protection and support of breastfeeding in Kenya. The goal for the MOH is that all women in this country be empowered to practice exclusive breastfeeding. This optimises maternal and child health and nutrition. The goal will be achieved through the “Baby Friendly Hospital Initiative” (BFHI). (This concept will be discussed later.)
What is exclusive breastfeeding? Exclusive breastfeeding is when a baby is fed on breast milk alone without giving any other foods or liquids for the first six months of life.
Why should you encourage mothers to breastfeed their babies? You should encourage mothers to breastfeed their babies because of the multiple benefits to the child, to herself, to her family and to society.
Breast milk provides many health benefits for the baby. When babies are exclusively breastfed, these benefits are highest. Overall, there is less illness requiring health care among exclusively breastfed babies. Exclusive breastfeeding provides the best infant nutrition and growth. With continued growth other foods are added when the child is 6 months old. Now let’s talk about specific benefits:
Benefits to the child:
- Breastfeeding provides protection against infection. Breastfed babies have less diarrhoea, and fewer gastrointestinal and respiratory infections.
- Breast milk is a complete balanced diet for the newborn baby.
- Breast milk alone is enough for the needs of the baby for up to six months.
- It is perfectly clean and hygienic.
- It is available whenever baby needs it. No preparation needed, such as to boil water or sterilise bottles.
- It is always at the right temperature.
- It promotes social bonds between the mother and child.
Health benefits to the mother:
- Oxytocin, a hormone that is released while breastfeeding, contracts the uterus and helps to stop bleeding after delivery. This is why it is so important that breastfeeding begins immediately after birth and continues frequently.
- Breastfeeding women are energy efficient. They can produce milk even with limited caloric intake.
- Frequent breastfeeding delays the return of menses in some women and helps to protect against another pregnancy. Thus helps in spacing children.
- There is a lower risk of breast and ovarian cancer.
Other benefits of breastfeeding:
- Postpartum depression is reduced.
- The workload of infant feeding is reduced.
- Emotional bonding results in less child abuse and neglect.
- Breastfeeding makes night feeds and travel convenient.
- There is no worry about milk getting spoiled or running out of supplies.
- There is no worry about infant formula shortages due to poor distribution, drought or crises.
Benefits to society:
Did you know that there are also breastfeeding benefits to the society?
- The cost of an adequate diet for the mother is less than the cost of feeding a baby with artificial formula.
- Mothers can use food money for other family members. There is no need to purchase breast milk substitutes or feeding equipment, and no need for extra fuel or water.
- The costs of medical consultation, medicine, laboratory tests and hospitalisation are reduced because mothers and babies are healthier.
- Thus breast feeding is economical.
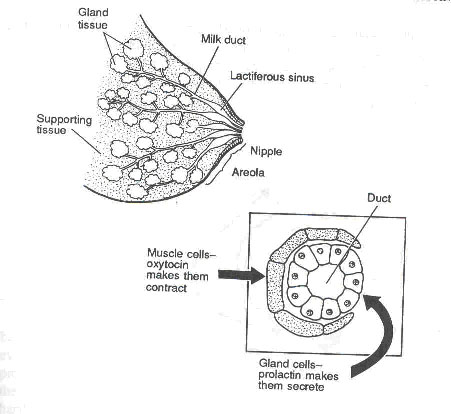
Remember the anatomy of the breast:
How milk is produced:
Milk is produced as a result of the action of hormones. Immediately after delivery, hormonal changes make the breasts begin to produce milk. When the baby begins to feed, two hormones make the milk come in the right quantity and at the right time. It is important for you to know these hormones so that you can advise mothers and help them to produce enough milk.
Two hormones control milk production: prolactin and oxytocin. The prolactin gland is situated in the anterior pituitary glands. Once a baby sucks at the breasts, the nerve endings in the nipples send messages to the pituitary gland to release prolactin into the bloodstream. The prolactin stimulates the milk glands to secrete milk. The more a baby sucks, the more milk the breasts produce. Therefore, if a mother wishes to increase her milk supply, she should have the baby suck longer and more often. She should not miss a feed to try to “save milk” because that will make her breasts produce less. Prolactin also has the important effects of suppressing the function of the ovaries. That is how breastfeeding helps to delay the return of fertility and menstruation.
The oxytocin hormone is also called the “milk ejecting” hormone. If you watch a woman breastfeeding, you sometimes see fine streams of milk flowing from the nipple. This is called milk ejection. As you know, small muscle cells around the glands of the breasts eject milk. When they contract they squeeze out the milk. Oxytocin makes these muscles contract. In fact, many women feel the squeeze in their breasts – sometimes called the “letdown reflex” – at the beginning of a feed.
Unlike the prolactin reflex, a mother’s thoughts, feelings and sensations influence the oxytocin reflex. If a mother is worried or afraid for some reason, or in pain – especially if breastfeeding is painful – or embarrassed, it can hinder milk ejection. This can result in engorged breasts. However, if she thinks lovely thoughts of her baby, is comfortable during breastfeeding or even hears her baby crying, this may help milk ejection. So to help a mother's milk ejection, we should be kind and supportive, help her not to worry, and reassure her that she can breastfeed.
How do babies suck? Babies have three reflexes to help them suck:
- The rooting reflex: This helps a baby find the nipple. You have seen that if something touches the side of a baby’s mouth, the baby opens the mouth and turns towards it.
- The sucking reflex: When something goes into the baby’s mouth, she/he sucks it.
- The swallow reflex: Once the mouth fills with milk, the baby swallows.
As you can see, the baby has reflexes to find the nipple, suck, and swallow the milk. But there is no reflex to help the baby take the nipple to the mouth. This is where the mother comes in. For a baby to suck effectively, she/he must take enough of the nipple and areola into his mouth. This is called “latching on” to the breast. Sometimes new mothers need to be taught how to get the baby to latch on properly.
Fig. 7.2: A baby sucking in a good position
Have the mother hold the baby close to her and facing her breast. The baby needs a large mouthful of breast in order to remove milk effectively. The baby suckles in a cycle of suck/swallow/breathe. The nipple, areola, and breast tissue together form a teat within the baby’s mouth. The baby’s tongue cups along the sides of the teat, and a wave of compression moves along the tongue toward the back of the mouth. The baby swallows when the back of his mouth is full of milk. Remember that poor positioning of the baby may cause breastfeeding problems such as cracked nipples, infections or breast abscesses.
Always advise mothers to hold their baby in the correct position and to sit or lie in a comfortable position (see Fig. 7.2). A bad sucking position can contribute to many common problems, such as sore nipples, not enough milk, or refusal to feed.
BABY FRIENDLY HOSPITAL INITIATIVE (BFHI): The Baby Friendly Hospital Initiative is a global campaign that gives health care and provides a leading role in the promotion, protection and support of breastfeeding. Any hospital/facility around the world that offers complete and accurate information about the benefits and management of breastfeeding is termed “Baby Friendly.”
How can you initiate BFHI in your health facility? You as a health worker, especially when you are working in a facility with a maternity unit, have an important role to play in protecting, promoting and supporting breastfeeding. This is a world-wide effort to ensure that mothers give their babies the best start in life. The World Health Organisation (WHO) and UNICEF have drawn up some guidelines for health units to follow. They are known as the “Twelve Steps to Successful Breastfeeding:”
TWELVE STEPS TO SUCCESSFUL BREASTFEEDING:
- The health facility first sets up some rules regarding breastfeeding that are to be routinely followed by all health staff.
- Train all health care staff in skills necessary to put these rules into practice.
- Inform all pregnant women about the benefits and management of breastfeeding.
- Help and encourage mothers to start breastfeeding within half an hour after giving birth.
- Show mothers how to breastfeed and how to maintain breastfeeding even if they are separated from their infants.
- Give newborn infants no food or drink other than breast milk for the first 4-6 months of life unless medically indicated.
- Practice rooming-in. This means allowing mothers and infants to remain together 24 hours a day.
- Encourage breastfeeding on demand. The mother should give the baby the breast every time the baby indicates a need to breastfeed.
- Give no artificial teats or pacifiers (also called “dummies” or “soothers”) to breastfeeding infants.
- Encourage the formation of breastfeeding support groups and refer mothers to them on discharge from the health facility.
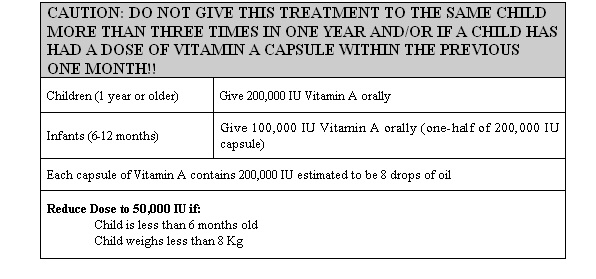
- Ensure that all infants delivered in the health facility receive BCG and Polio vaccines before discharge. Mothers are given Vitamin A capsules.
- Issue a properly filled in Child Health Card to every mother/infant pair at discharge.
Fig. 7.3: A health worker helping a mother put her baby onto the breast in the correct position.
When all twelve steps are fulfilled, your unit can be assessed and rewarded for being baby friendly. If you find that the above information on BFHI is inadequate, you can discuss the matter with your supervisor who will give you more information about BFHI.
Overcoming problems of breastfeeding: There are a few common problems that mothers can have with breastfeeding, especially in the first one or two weeks. The most frequent are a mother’s anxieties about her performance and the amount and quality of her milk. Others include flat nipples, sore nipples, and very swollen and tender breasts.
The health worker is a very important person who can support and encourage a new mother so that she breastfeeds successfully.
See Fig. 7.3. A husband can provide the best support if he is available (see Fig. 7.4). Preparation for breastfeeding during pregnancy can avoid a number of these problems. You should contact every mother during pregnancy and discuss breastfeeding. You can even include the father in these discussions if he and the mother are willing.
Problems when breastfeeding are many but we shall only discuss the most common ones:
1. Mother’s anxieties (Too little milk or that it is of poor quality): The mother should be taught to pull out the nipples and gently press out a few drops of fluid. This can build up her confidence in her ability to breastfeed successfully. As a health worker, you should give encouragement, support and comforting answers to the mother’s questions. Ask her to take enough food and fluids so that she has the energy she needs to produce enough milk.
If the mother says the baby cannot suckle, help the mother put the baby to the breast. If the baby still refuses to suck, check what is the problem. Is it the breast? Does the mother have an inverted nipple or engorged breast? If you find it is not a problem with the breasts, then assess the child for other problem such as fever, blocked nose, oral thrush, etc., and manage accordingly.
2. Flat nipples: Some women have short, flat nipples. Flat nipples are most common in women who are having their first baby. If a nipple is not protractile, the baby will have difficulty in feeding.
It is very important to examine the breasts of every pregnant woman. Teach her to squeeze her nipples and pull them gently. She should do this for several minutes every day. Her nipples will grow longer. After the baby is born, the nipples can still be stretched further. The mother should squeeze the areola before putting the nipple in baby's mouth.
3. Swollen (engorged) breasts:
Sometimes a mother’s breasts produce more milk than her baby needs. This is common in the first week after the baby is born. Sometimes the baby is too weak to suck all the milk, and sometimes it is just more than the baby needs to drink.
As you learned in Unit 3, if the breast is not emptied normally it becomes painful and swollen with milk. The skin is tight and the baby cannot put the whole areola into his/her mouth to suck. Sucking may be very painful to the mother. Tell the mother that she can prevent and treat engorged breasts by emptying them regularly.
Fig. 7.4: A husband can encourage his wife to breastfeed their baby.
Frequent breastfeeding relieves the pain. Teach a mother to express some milk when her breasts feel painfully full. Placing a cold cloth on the breast just after milk has been removed can help relieve oedema. If an engorged breast is not emptied, the amount of milk produced will decrease quickly.
An empty breast should be soft without any lumps. A blocked milk duct in the breast can sometimes cause a tender lump in the first week of breastfeeding. Apply a warm cloth to the areola area just before a feed to get milk started. Empty the breast and then gently press to empty the lump. This will prevent serious problems later.
4. Sore nipples: Nipples are very sensitive. If the skin is very soft and the baby sucks very hard, soreness develops. Sometimes the soreness develops into a crack that is very painful. Infection can get into the breast through a crack in the skin.
To prevent sore nipples, the mother can keep the skin soft by rubbing the areola and nipples with some oil. She should not let the baby suck for too long at first. Tell the mother to empty the breasts by expressing them if the baby does not suckle them empty. Let the nipples dry in the air after feeds.
If necessary, give an analgesic. Sometimes germs enter the breasts, perhaps through a crack in the nipple, and this causes infections. Antibiotics are then needed and the mother should be referred to the next larger unit. In the meantime, the breast should be kept empty by suckling the baby or expressing.
Cultural beliefs and practices affecting breastfeeding: Many cultural and local beliefs can affect breastfeeding. It is important to know how mothers in your community traditionally feed their children. In all communities, people have cultural beliefs, taboos and special practices concerning food production, preparation, serving and eating. You need to know which ones exist in your area, as you may need to give advice about them during your work.
| 10
Can you think of any of the cultural practice and beliefs which affect breastfeeding? …………………………………………………………………………………………………… …………………………………………………………………………………………………… …………………………………………………………………………………………………… …………………………………………………………………………………………………… How would you manage them? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………
|
Breastfeeding can be affected by the traditional feeding practices in society. As a health worker it would be very important for you to find out about feeding practices in your community. You can find out about traditional feeding practices by observing and asking questions.
Questioning can be done in a simple way. Here are some useful questions that may help you find out about infant feeding practices in the community.
- How soon after birth do mothers breastfeed their infants?
- What does the mother do with the colostrum? Does she make sure her baby sucks it?
- How are newborn babies fed for the first few days of life?
- Do all mothers in the community breastfeed their babies?
- For how many months does a mother breastfeed her baby?
- What foods is a mother not allowed to eat during lactation?
- What food or drink is given to the baby when the mother goes out to work?
- What would make a mother stop breast feeding abruptly?
We know very well that all people have their likes and dislikes and their beliefs about food. Feeding habits, however, can be changed as a result of both the influences of other people and sensible adaptation to local circumstances. A health worker can play a very important role in influencing desirable behaviour.
You should discourage harmful beliefs. One such belief is that it is best to take a child off the breast when she/he has diarrhoea for fear of making it worse. Other common local beliefs include taking the baby off the breast because the mother has stayed away overnight, or abruptly stopping breastfeeding because of an eminent pregnancy. There are many other common but erroneous beliefs.
While we examine bad cultural practices, we should also keep in mind the recent influences that are changing good breastfeeding practice. These influences include the urban way of life, women working away from home to earn additional income, the advertising of infant foods, and the idea that breast milk substitutes are modern and therefore better.
As a health worker you should act to reduce the effects of these negative influences on breastfeeding. Encourage the development of useful cultures such as breastfeeding a child exclusively for six months, and gradually introducing foods while continuing breastfeeding. Teach mothers that working outside the home need not keep them from breastfeeding, and that breast milk is far superior to breast milk substitutes.
WEANING:
Weaning is the process by which an infant gradually becomes accustomed to an adult diet. The child's diet changes from breast milk alone to a diet based on regular family meals.
Mothers should start weaning their babies at 4-6 months of age. This is because at this stage the breast milk is relatively deficient in iron and an infant’s store of iron is sufficient only until about 6 months of age. From 6 months onwards, the infant may need extra food to provide extra energy, protein, iron, and vitamins for his/her growth.
What foods should be given? It is very important for you to find out which foods are grown locally in your area and which foods are available in shops and markets. Find out some information about the feeding of young children in your community. This information will guide you as to how to give advice on weaning foods.
Remember that feeding practices are part of the customs and traditions in any community. Religious beliefs also influence feeding practices. Feeding practices may also vary among different social groups.
Common foods in most communities are:
- Cereal grains: wheat, rice, millet, maize, sorghum etc.
- Leafy green or coloured vegetables or fruits: sukumawiki, carrots, tomatoes, pumpkin, pawpaw, mangoes, amaranth (Amaranthus), nakati, and Legumes or pulses: Peas, beans, lentils and cassava leaves
- Foods from animals: meat, eggs, fish and milk.
- Oils and sugar: Vegetable oils, animal fats, sugar etc.
- Tubers: cassava, yam and potatoes.
- Fruits: bananas, mangoes, pawpaws and oranges.
How should weaning foods be given? This depends on where you are and on the traditionally available staple foods. Let’s look at an example. If the staple is a cereal such as maize, millet or rice, it will provide a useful quantity of protein. If the staple is banana or a root such as cassava or yam, it will supply very little protein. In either case, but especially in the latter, it is vitally important to provide extra protein-rich foods.
Adding protein is not difficult. Milk can be added to a number of foods eaten by the child to increase the protein intake. A fresh egg beaten into the porridge while it is simmering in the pan is another simple way of providing excellent protein for a toddler. Meat or fish, if cut up finely, cooked well and mashed with the staple food also will provide protein of good quality.
Animal protein products may not be available or may be too expensive for a family budget. Legumes such as beans, peas, lentils, cowpeas and groundnuts are good sources of protein and should be added to the diet of the child. These can be ground or crushed before or after cooking. Beans give good soup as long as the bean skin is removed.
The above foods, as well as providing energy and protein, will also provide vitamins and minerals. Additional vitamins and minerals can be obtained from dark green leafy vegetables and coloured fruits.
What you have to note well is that young children need soft foods. They have no teeth with which to chew. Young children have small stomachs. They cannot eat a lot of food at once. At the beginning, food should be given only once or twice a day in small amounts. Gradually increase the number of supplemental feedings to 3 or 7. Increase the amount of food slightly later when the child is used to the food, given 4 to 5 times a day in small amounts.
A child is gradually fed on a more solid diet as she/he gets more teeth. By the age of 2 years, breastfeeding will usually have ceased and the child is completely weaned.
| 11
What is the most common weaning food in your community? …………………………………………………………………………………………………………… …………………………………………………………………………………………………………… …………………………………………………………………………………………………………… …………………………………………………………………………………………………………… How would you prepare it for an 8 month old infant? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Proper hygiene and food preparation: When a caretaker is beginning to give supplemental foods to a breastfeeding infant, certain practices should be put into place. These practices involve proper hygiene and food preparation. You as the health worker must teach parents the following:
- Wash hands before preparing weaning food and before feeding the baby.
- Prepare food in a clean place
- Wash uncooked food in clean water before feeding it to the baby.
- Cook or boil food well when preparing it.
- Cover foods that are being kept. Keep foods in a cool place.
- Mash and mix food with enough liquid such as milk or soup to make it semi-solid. Add some foods rich in oils such as simsim and groundnuts paste. Add sugar when necessary to make the food taste good.
- Feed the baby with clean spoon, cup or clean hands. Do not use a feeding bottle.
- If cooked food is prepared two hours in advance, boil it again before feeding it to the baby. Make sure the food is not too hot when giving it to the child.
- Continue with breastfeeding as baby is being weaned.
You have learned that weaning is a process by which an infant is gradually introduced to the adult diet. You have identified the local foods used for weaning and how weaning is done using these foods. We are now going to discuss the next topic, which is on growth promotion monitoring.
7.5: GROWTH PROMOTION MONITORING
Growth promotion monitoring (GPM) is usually carried out in young child clinics or in the community. This is done to see whether a child is growing well, is healthy and is adequately fed. Therefore, food is needed for growth, physical activities and maintenance of health. Terms used to assess the child’s health are growth and development.
Have you met these words in the text before? Please look again at Unit 3 on growth and development.
Growth means getting bigger. A child gets bigger because her/his bones, muscles and other body tissues increase in size. So a child needs body building nutrients and energy giving nutrients to grow.
Development is the increase in the number of skills performed by the body, including the brain in the performance of those skills. The growth and development of the brain requires adequate nutrition just like other parts of the body.
When a baby is born, it can do very little for itself. Gradually he/she develops and is able to move his/her body in the way he/she wants and can do simple things. Special skills like talking develop later. It is useful to know the ages when most children can do the same simple things. These are used as markers of development and are some times called “milestones of development”
In children, normal growth and development are signs of good health and nutrition. One of the best ways to measure a child's health is to measure growth. The easiest way to measure growth is to weigh a child regularly and to note how his body weight is increasing with age in comparison to the weights of healthy children of the same age.
Let’s begin by looking at the advantages of Growth Promotion Monitoring.
ADVANTAGES OF GROWTH PROMOTION MONITORING: Plotting children's weights on growth charts allows parents and health workers to see how they are growing.
- A family can compare the shape of their child’s weight line with the reference line. If the child is gaining weight at the same rate as the reference line, the parents know they are caring well for the child. If the child is gaining weight too slowly, they know the child needs more food or care.
- A family can see if their child stops gaining weight when she/he is sick. They can check that she/he is regaining lost weight quickly as she/he recovers.
- Families and health workers can identify children with growth failure early when it is easy to help them.
- Health workers know which families have under-nourished children and so need help most.
- Growth Promotion Motoring gives you a chance to meet mothers regularly and deal with problems quickly.
How do we measure growth and development?
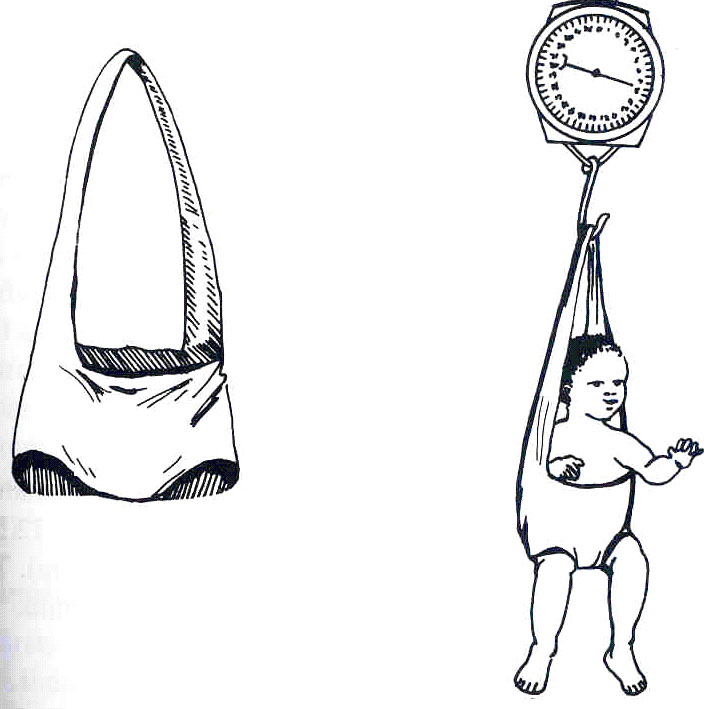
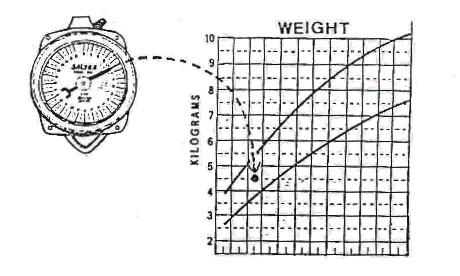
Growth is measured in different ways. Body weight is the simplest measurement, and in children, change in weight is the most reliable indicator of growth. In Kenya, many health units have been equipped with salter scales provided by UNICEF. Do you have one in your health unit? Which one do you have?
A Salter scale has one hook above to hang from a beam or a branch of a tree, and one hook below from which hangs a pair of pants in which the child is placed. There is a face or dial that looks like a clock (see Fig. 7.5). The weight is marked in kilograms around the dial. The weight measurement that is obtained from the salter scale is then plotted on the growth chart.
Fig. 7.5: A Salter scale. The top hook is fastened to a hook in the ceiling or a doorframe. A sling in the form of a pair of pants hangs from the bottom hook. The child is placed in these pants and weighed.
Some health units have been supplied with uni scales which come with instruction on how to use them. If you have this type of scale, then read instructions carefully. If you find them difficult to understand, please contact your supervisor.
| 12
We have just mentioned a growth chart where the weight of the child is plotted. What is a growth chart? Describe a growth chart below: ……………………………………………………………………………………… ……………………………………………………………………………………… ……………………………………………………………………………………… ……………………………………………………………………………………… ………………………………………………………………………………………
|
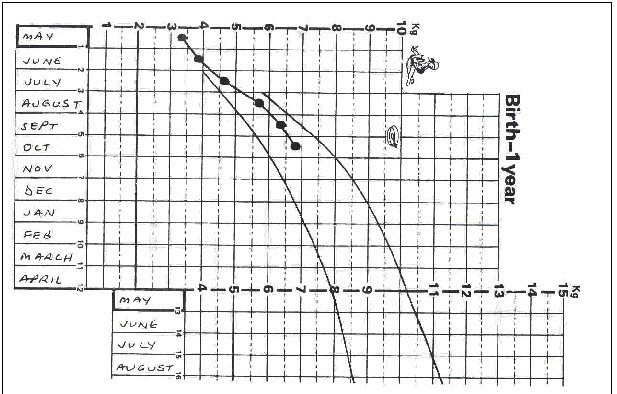
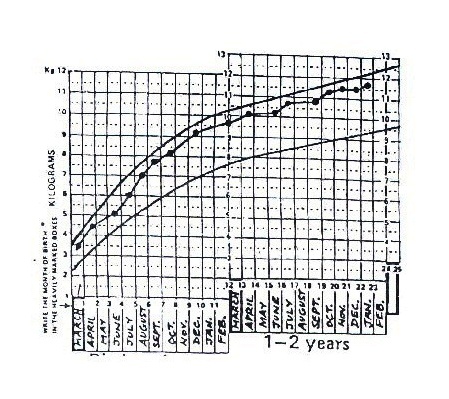
Was your answer similar to this? A growth chart is printed on the inside of the child health card. It is a graph on which a child's weight is shown at different ages (see Fig. 7.6). In order to use the growth chart, a child must be weighed and measured at regular intervals and have his/her weight marked on the chart at the place corresponding to his/her age.
(See Fig. 7.6)
The Child Health Card should be given to the caretaker who keeps it at home. You should remind the caretaker to bring the card every time they visit the health unit with the child. Most caretakers, for whatever reason, do not usually carry these health cards along.
| 13
Why do you think parent fail to bring the health cards along each time they bring their children for weighing? (Give three common reasons) …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………… How could you encourage the caretakers to carry the Child Health Cards along? ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………
|
DETERMINING AGE AND WEIGHT:
Always remember that there are two important factors in measuring growth: weight and age. It is very important, therefore, to know the age of a child. Often caretakers do not remember the dates of birth of their children.
Finding out the child's age. How would you help the caretaker to find out the age of the child if she/he has forgotten? In such cases you can estimate the age of a child by asking the caretaker certain questions and by using a local events calendar. A local events calendar shows all the dates on which important events took place. It may show the different seasons, months, phases of the moon, local festivals and events in the agricultural cycle. National and local occurrences of importance are also marked on it: these include storms, political elections, the opening of nearby roads, shops, etc. You should make your own events calendar now.
A local events calendar helps much more in estimating the ages of younger children before the age of four years. In the case of older children the year of birth becomes difficult to estimate correctly. However, with older children it is not so important to be absolutely accurate.
How to weigh a child accurately: A child's weight is the most reliable measure of health and nutrition. Weighing a child requires reliable equipment and a standard method to achieve accurate results.
The most common type of weighing scale in our health units is the salter scale, which we have already described. Accurate weighing is important. You can learn how to weigh a child quite easily by following the instructions given below:
- Hang up the scale securely, keeping the dial at eye-level so that the weight can be read easily.
- Adjust the pointer of the scale to 0 by turning the knob on the top of the scale. When you do this, the empty pair of pants should be hanging from the scale. This is done to account for the extra weight of the pair of pants.
- Ask the caretaker to remove any heavy clothes and shoes from the child. Light clothing can be left on. The caretaker can also put the blue plastic pants on the child in preparation for weighing.
- Put the loop of the trousers over the hook of the scale and ask the child to hold on to the straps that hold the pants (if the child is old enough to understand). The caretaker can stand nearby and talk to the child to reassure her/him. You should check, however, that the caretaker is not holding the child and that the child’s feet are off the ground.
- Read the weight on the scale. If the child is struggling try to calm him with the help of the caretaker and when she/he stops moving read the weight quickly.
Enter the weight on the Growth Chart exactly as it appears on the scale. The markings on the face of the scale correspond to those on the Growth Chart. If the pointer points halfway between the four and five on the scale, place a dot half way between four and five kilograms on the Growth Chart (see Fig. 7.7).
Fig. 7.7: A Salter scale and marking the weight on the Growth Chart.
6. Remember the dot should be placed in the middle of the column corresponding to the month of weighing.
The line of dots that a child's weight makes on the card is called his/her growth curve.
How do you interpret the growth curve?
There are two growth reference lines on the growth chart. The area between these lines gives the general direction of growth in healthy children.
Remember that this does not represent the target of growth for all children. If a child’s weight on the first weighing is much below the lower line there is some reason for concern, and you should look for the reason. However the direction of the child’s own growth line, based on weighing at regular intervals, is of much more significance than any single weight recorded below the lower reference line.
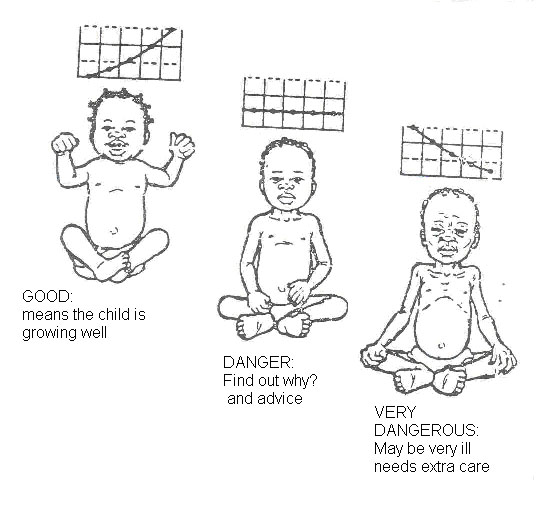
Look carefully at the growth line in Fig. 7.8. Note that the line is going upwards from left to right, from 5.5 kg in November 1996 to 6.5 kg in December, and then 7 kg in January 1997. Remember that when the line is going up, the child is growing. This is good. If the line is horizontal, the child is not growing well and this is not good.
Fig. 7.8: Growth Chart with plotted weights.
Fig. 7.9 offers some examples of the direction of the growth curve. This is to remind you that the direction of the curve tells us a great deal about the condition of the child.
Sometimes you will come across a weight line that is rising much faster than the reference line, as in the left-hand illustration in Fig. 7.9. This probably means that the child is catching up on weight lost during a previous illness or a period of growth failure. But this may also indicate a health problem that is causing obesity. A look at the child’s health record should indicate whether or not there needs to be further investigations.
A weight line that is flatter than the reference line means that the child is gaining weight too slowly. If the line is flat, as in the middle illustration in Fig. 7.9, you know that the child is not gaining weight at all. This is a warning that something is wrong. The child may be sick and/or not eating enough, therefore extra food and care are needed.
A weight line that is going down, as in the right-hand illustration in Fig. 7.9, means that the child is losing weight. This is very dangerous. The child is not eating enough, is almost certainly ill, and needs immediate help.
Fig. 7.9: Three examples of a child’ growth line. Watch the direction of the line, which shows the child’ health status.
When you interpret a child’s weight line, look at:
- The child's age. The younger the child, the more serious the effects of growth failure.
- The position of the line on the chart: The slope of the line is more important than its position on the chart. However, a small child who becomes ill or has a poor diet has less body stores of fat and other nutrients and so is more at risk of under-nutrition than a bigger child.
- Weight that does not increase for three consecutive months could be a bad indicator. Therefore urgent attention should be given. Such a child is becoming malnourished.
How would you help the caretaker understand the growth chart easily?
It is very important for you to take as much time as possible to explain about the Growth Chart to the caretaker. She/he is primarily responsible for the child and with the child most of the time. If it is really made clear to the caretaker that the child is not growing properly, she/he is the best person to do something about it. It is important to explain to the caretaker about the two curved lines that are printed on the Growth Chart.
The top line represents the average growth line of healthy children in a well-nourished community. Nearly all (97%) well-nourished children should fall above the lower curved line on the chart. If a child has a growth line below the lower line on the chart, it means that she/he is rather small for her/his age. If the child’s own growth line is going up in the same direction as the printed curved line, this means that she/he is growing well and that she/he is just a small person.
A note should be made on the Growth Chart of important events that affect the child’s growth and health.
Now pick up a Child Health Card and study the Growth Chart inside. Examples of events that can affect a child’s growth and health are listed at the bottom right hand corner of the inside of the Growth Chart. If a child has measles, for example, this should be written on the Growth Chart next to the dot representing the child’s weight at the time the child was seen.
Similarly, the day that the baby is first given food other than breast milk, the day when the child is weaned, and the birth of another child are important events. These should be noted on the Growth Chart. Most of these events make a child vulnerable and at risk for malnutrition. Therefore, there is a need to follow them up.
How can you identify a child at risk for follow up? There is a box at the top of the Growth Chart marked “Reasons for special care.” Some of the factors listed may make a child particularly vulnerable to malnutrition. A tick or mark should be made next to any of the reasons that apply. This will then remind you to be particularly alert to any signs of growth faltering and may suggest the reason for poor growth. You can then plan how best to help this child.
If a child, especially an undernourished or “at risk child” does not attend PGM (Growth Promotion Monitoring) regularly, find out how he/she is by visiting the home or consulting a community health worker, colleague or neighbour who knows the family.
If you refer a child to a senior health worker or social worker, try to find out if the family
Fig. 7.10: A caretaker taking his children for regular growth promotion monitoring.
has been helped. If a child goes to hospital, find out what happened to him/her and monitor him/her carefully when discharged. All the information recorded on the child health card will assist you in assessing the direction of progress.
How can information from the Growth Chart be used to help a community improve health and nutrition?
The success of managing the health of a child depends on adequate information. Fighting malnutrition is your duty and the job of all those who have health-related jobs. Nutrition work therefore should be planned and implemented by all the health workers and community members.
The information from Growth Charts can be used to show a health unit staff how nutrition in the community is changing from one time to another. Particular groups of people or people living in particular places might be found to be more malnourished than others. This information can be used by the health unit staff to try to understand more about causes of malnutrition in the community and how nutrition and health of young children can be improved.
Discuss this type of information with other community workers, especially those working in the fields of agriculture and community development.
Information from Growth Charts can also be of use at the District and National levels in order to understand which communities have the greatest nutrition problems and how effective various programmes aimed at improving nutrition have been
Remember: In order to detect growth failure and prevent malnutrition, encourage caretakers to have their children weighed regularly – at least once every two months, even if the child is not ill.
7.6: MALNUTRITION
Before beginning this section, complete the activity below.
What is malnutrition? Malnutrition means wrong or faulty nutrition. The fault may be too little food or the wrong or even too much food. The most common forms of malnutrition in our communities are due to shortages (deficiencies) of energy giving food. These shortages give rise to the group of diseases called “protein energy malnutrition” (PEM). Vitamin and mineral deficiency diseases occur if the food does not contain sufficient amounts of essential nutrients that are required in very small amounts to protect the body against certain diseases.
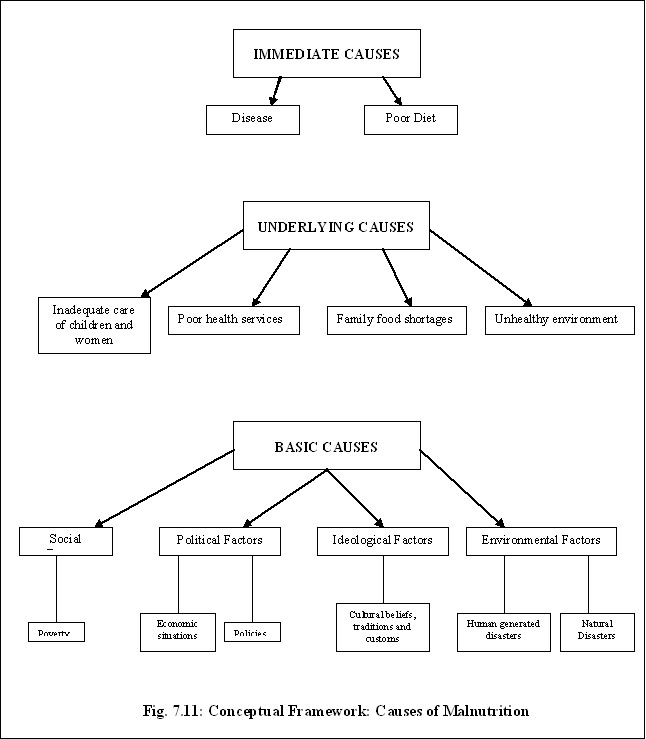
What are the causes of malnutrition? The problem of malnutrition is very complex because it is influenced by many factors acting at multiple levels. These often act in a vicious cycle and include dietary intake issues, diseases, food insecurity, inadequate maternal and child health care and sanitation services, illiteracy and poverty, among others. We can discuss the causes of malnutrition using a conceptual framework that serves as a guide to identify and clarify the various causes of malnutrition. Fig. 7.11 gives this conceptual framework of the causes of malnutrition.
We can now look at each of these causes in more detail.
A) Immediate Causes: The immediate causes of undernutrition and malnutrition are generally due to:
- Poor diet
- Disease
1. Poor diet: A poor diet may be due to:
- Not enough food, or a lack of variety of foods in meals.
- Low concentrations of energy and nutrients in meals.
- Infrequent meals.
- Insufficient breast milk and early weaning.
2. Disease: Diseases, especially infectious diseases, cause undernutrition because a sick child may not eat or absorb enough nutrients, or she/he may lose nutrients from the body due to vomiting or diarrhoea or have increased nutrient needs. The diseases most likely to cause undernutrition are:
- Measles
- Diarrhoea
- AIDS
- Respiratory infections
- Malaria
- Intestinal worms.
B) Underlying Causes: The underlying causes differ from community and family to family but it is useful to group them into:
- Family food shortages.
- Inadequate care of children and women
- Unhealthy environment and poor health services.
- Too many children in a family to feed.
For each underlying cause you identify, there is probably another, “deeper” cause. For example, a child may have a poor diet because the family has little food. But why is the family short of food? Perhaps they have too little land or a low income. But why have they too little land? Keep probing and asking “But why?” Eventually you will determine the basic causes.
Let us now examine the underlying causes further under the three groups given above.
1. Family food shortages: Many families do not have enough food to feed everyone properly throughout the year. But why are these families short of food? Some of the reasons are:
- The area of farming or grazing land has decreased because of increased population.
- Yields from crops or livestock are poor due to low or erratic rainfall or to pests and diseases.
- Over-cultivation, overgrazing or soil erosion has made land less productive.
- Mould and pests destroy much stored food and many families lack the information or resources to improve storage facilities.
- Fresh foods, such as vegetables and fruits, are often not available all year because families do not know how to preserve them properly.
- Families that stay in urban areas cannot buy enough food when incomes are low compared to food prices.
- Poor budgeting. Some people spend so much on “non-essential” things such as beer, etc., so there is not enough money left for the family’s food needs.
- Poor distribution of food among the family members
2. Inadequate care of children and women. Nutrition and health care are partly determined by the amount of care given to women and children, and this is strongly influenced by a woman’s workload, access to resources and education.
- A woman’s workload affects the amount of time she spends breastfeeding, cooking and encouraging the children to eat, cleaning the home, and children, playing with the child, attending clinics and learning new information or skills.
- Some women must work far from home and this may mean the child is bottle fed or left with an inexperienced or disinterested maid who may not feed the child properly.
- Many women head families because men have to work away from home, or are unmarried, divorced, widowed or abandoned. Women who have no support from fathers/husbands or other relatives have very heavy workloads.
- Many women are uneducated and have little knowledge about feeding, childcare and hygiene. Thus they lack awareness of the correct thing to do these same women often cannot or do not attend clinics or women’s groups where they could learn skills to improve their lives and that of their families.
3. Unhealthy environment and poor health services: Disease is more likely to occur, especially among young children, when there are poor living conditions; overcrowding and poor health services.
• Unhealthy environment:
- Poor or expensive water supplies make it difficult for people to keep their homes, food and themselves clean.
- Poor disposal of human and animal faeces leads to diarrhoea and other diseases. A dirty environment allows rats, flies and other carriers of disease to breed.
- Respiratory and other diseases spread quickly when people are in crowded, poorly constructed houses.
- Food may not be thoroughly cooked and drinking water may not be boiled.
• Poor health services. Poor health services lead in poor health care of the sick children community because:
- Infections are not treated promptly and there may be shortages of drugs, skills, staff, etc.
- Few children are immunised.
- Less advice is given on how to prevent or control diseases.
- There is less control of environmental hygiene in markets and other public places.
C) Basic causes:
The availability and control of resources (human, economic and organisational) at the various levels of society is a result of four major factors:
- Political factors, such as policies and economic situations that affect household, district or national levels of society.
- Ideological factors, such as cultural beliefs, traditions and customs that influence the nutritional state of vulnerable groups.
- Environmental factors, such as war or natural disasters (draught, flood).
- Social factors, such as poverty.
1. Political factors: Certain political factors, such as policy decisions and economic situations caused by inflation or war can cause undernutrition.
2. Ideological factors: The effects of cultural beliefs, traditions and customs on nutrition are enormous in our communities, but they vary from region to region. Cultural beliefs, traditions and customs mostly affect the nutrition of women and children. Generally, men take advantage of the opportunity to eat better than their wives or children. Here are some examples of cultural beliefs, traditions and customs affecting nutrition of the children.
- Abrupt weaning due to pregnancy.
- Food should not be given to a child who is suffering from measles or diarrhoea.
- Serving food late waiting for the husband to return home.
- Sharing food in the same bowl. This practice often results in the child getting less than his/her body requirements.
- The pattern of authority in the home regarding food purchasing and preparation.
- Food prejudices:-Certain foods are considered inferior foods while others are considered superior foods.
3. Environmental factors:
- Natural disasters can cause malnutrition because of the effect these disasters have on growing crops or harvest. Examples include drought, floods and earthquake.
- Human generated disaster, such as wars, can cause undernutrition or malnutrition because often people are displaced and unable to grow food at all. If they are displaced they must leave their livelihoods behind, and cannot buy food. The most affected in such situations are children and women.
4. Social factors: Poverty is the reason that some families cannot produce or buy more food. Men leave home to search for work, leaving women to bring up children alone. Poverty can lead to family quarrels and child abuse. Often women have less access to money, land and other resources and less control over family decisions than men.
We have now come to the end of our discussion of the causes of undernutrition using the conceptual framework. If you are not very clear about the explanation, please go back and read it again. If you have internalised this material, then let’s talk about the common nutritional problems in our community.
First, take time to complete the activity below:
PROTEIN ENERGY MALNUTRITION (PEM):
The condition we are going to talk about first is the one brought about by shortages (deficiencies) of proteins energy giving foods. This leads to “protein energy malnutrition,” or PEM. This include arrange of conditions which are:
- Underweight
- Marasmus
- Kwashiorkor
- Marasmic kwashiorkor.
1) Underweight: This mildest form of PEM can be detected only by checking the weight of the child and plotting it on the weight for age (or growth) chart. In “under weight” the child has an expected weight for age of 60-80%. There are no other remarkable signs, but the child may look thinner and smaller than other normal children. These children need special attention because:
- There are very many underweight children in the community. Most are between 1 - 3 years of age.
- Underweight children grow and develop more slowly than well-nourished children.
- They are considered "at risk" for illness. Underweight children are always in danger of picking up infections very easily. These infections are more serious and more prolonged than in well-nourished children and are more likely to cause death.
Management of the underweight child:
- Look for the primary causes of the child’s undernutrition.
- Advise on good mixed diets.
- Follow up those children under the age of five years and observe the growth line. If there is no catch up in weight, or if the weight stays the same or is lost, then refer the child for further examination and treatment.
- Carry out comprehensive immunisation.
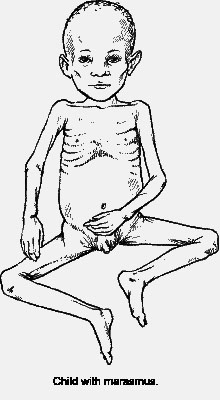
2) Marasmus: Marasmus literally means “starvation.” Marasmus can occur at any age but is more commonly found in infants who do not get enough breast milk, or during the weaning period are not given adequate food. Infections are often contributing factors.
Clinical features.
- The weight is below 60% of the standard weight for age.
- Lack of subcutaneous fat. Legs and arms are thin.
- The skin is thin, wrinkled and seems to be large for the body it covers.
- Child looks anxious and has a face like that of an old person.
- The child is usually hungry, suckling at his/her fingers
- There may be constipation or diarrhoea, which is often the reason why the mother brings the child for medical care.
Fig. 7.12: Marasmus
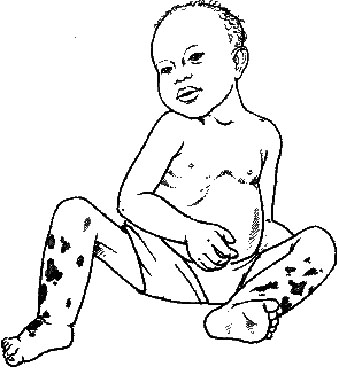
3) Kwashiorkor: Kwashiorkor is a word from a Ghana language that means “illness of the displaced child.” Displaced in this context means that a younger brother or sister has displaced the child from her/his mother’s breast. Many local languages describe the presence of oedema in this disease, and for that reason it is sometimes called “wet malnutrition.”
Kwashiorkor can come on rather quickly over a few weeks. It often follows infections like measles or diarrhoea, and may suddenly develop in a child who is underweight, failing to thrive or marasmic.
Clinical features:
- Weight for age is between 80-60% of that expected for the age.
- There is weight loss, with muscle wasting
- Pitting oedema, of the legs and hands.
- The face is puffy (moon faced).
- The child is miserable. He/she is not interested in his/her surroundings and refuses to feed.
- The skin is light coloured, thin and weak and may peel off (Flaky; also called flaky paint dermatosis). Skin sores and fissures occur frequently.
- The hair becomes brownish, straight, thin and easy to pull out. (Note that occasionally some normal children may show this brown - hair sign).
- Subcutaneous fat is retained.
- Diarrhoea, anaemia and enlarged liver are common features.
Fig. 7.13: Kwashiorkor
4) Marasmic Kwashiorkor: Most children with Kwashiorkor show some wasting of muscles and loss of subcutaneous fat. If this is severe enough to reduce the child’s weight to below 60% of normal weight for age, despite the oedema, the child has marasmic kwashiorkor. In this most severe form of PEM, a child has developed acute oedematous malnutrition, usually following an infection like measles. An adequate energy and protein intake is needed urgently, and as oedema is lost, the true extent of the child's marasmic state will be revealed.
Management of moderate and severe PEM: All health workers should be able to recognise severely under nourished children. Severe marasmus or kwashiorkor children must be referred to hospital for in patient care and eventual nutrition rehabilitation.
- Malnourished children die easily from hypoglycaemia, hypothermia find overload and undetected infections
The steps of management that severely malnourished children undergo on admission are:
- Treatment/prevention of hypoglycaemia.
- Treatment/prevention of hypothermia by providing warmth
- Treatment/prevention of dehydration.
- Correction of imbalance of electrolytes.
- Treatment and prevention of infections.
- Correction of micro nutrient deficiencies.
- Cautious feeding (therapeutic feeds).
- Intensified feeding to rebuild wasted tissues and provide catch up growth (supplementary feeding on locally available food).
- Provide sensory stimulation and play and emotional support
- Nutrition education of parents and preparation for discharge and follow up to ensure adequate recovery is achieved in this rehabilitation phase of treatment.
Although the ten management steps for severe malnutrition are carried out in a hospital, you should know in a summary form what actually is done at hospital let us see the main aims of management. The ten steps aim at achieving:
- Reduction in the high mortality which usually occurs in severaly malnourished children.
- Regaining the lost growth and development
- Reduction in recurrences of malnutrition once the child has improved and discharged home.
What is done in the management steps include:
- The child is admitted with his mother to hospital in a warmed/heated room to correct and maintain body temperature which is usually low.
- The child is fed on special formulas and given supplement to provide proteins, energy, Vitamin A, Minerals such as Zinc, Potassium, Magnesium and copper. Iron is not included among the minerals to be given.
- The child receives broad spectrum antibiotic for example co-trimoxazole (septrin) to treat infections which normally do not manifest with fever.
- The child receives stimulation making him/her cheerful playful and accepting and accepting feeds.
- The child’s temperature, weight, hydration status and oedema are monitored regularly to ascertain progress and recovery
- The mother is assisted to participate in the management and taught what to do after discharge particularly on feeding on locally available food. Rich in proteins and energy
- Special associated conditions and complications are looked for and managed.
These include: Dehydration, Heart failure, tuberculosis, intestinal worms, missed immunisation and associated other deficiencies such as Vitamin deficiency and anaemia.
Consequences of PEM: The effects of undernutrition are potentially serious, depending on how severe it is, how long it lasts, and the child’s age. Children with marasmus and kwashiorkor:
- Often die.
- Often remain weak and stunted throughout life. Some are permanently mentally damaged.
- Are often anaemic and suffer from xerophthalmia, an eye condition that can eventually end in blindness, caused by Vitamin A deficiency i.e. children with marasmus and kwashiorkor may have other nutritional disorders.
- Suffer and give their parents a lot of anxiety. Getting treatment can be expensive and difficult.
MICRO-NUTRIENT DISORDERS:
Having discussed protein energy malnutrition, we will now discuss common micro-nutrient disorders. Micro-nutrient disorders are many, but we shall only include those that are most common and therefore of great importance in our communities. These are:
- Vitamin A disorders
- Iron deficiency anaemia
- Iodine deficiency disorders
Vitamin deficiency disorders occur commonly in association with PEM. Isolated vitamin deficiency disorders not associated with PEM are rarely seen with exception of folate (Folic acid) deficiency.
1) Vitamin A Deficiency (VAD): Vitamin A deficiency is most common among young children below the age of 5 years. Children with marasmus, kwashiorkor, measles and prolonged diarrhoea are mostly affected.
Vitamin A deficiency occurs when a child has used up the stores of vitamin A in the liver and is not getting enough from food. The vitamin is present in milk, and meats like liver, but for most people the main source of Vitamin A in the diet is the carotene pigments in plants. The body then transforms the carotene into Vitamin A. Any red, yellow or dark green vegetables will contain carotene, including dark green leaves like spinach, tomatoes, carrots, pawpaw, and red palm oil.
Some diseases increase the risk of vitamin A deficiency because they:
- Reduce the appetite so a child gets less Vitamin A.
- Reduce absorption of Vitamin A (such as diarrhoea or worms).
- Increase Vitamin A needs (such as diarrhoea and measles).
Clinical features:
There is no easy-to-see early sign of VAD. It is often not recognised until the deficiency is so severe that it causes a disorder of the eye called Xerophthalmia. The signs of xerophthalmia, which usually appear in the following order are:
• Night blindness: The child cannot see in dim light. In the evening, the child trips over things. Night blindness may be a sign of early xerophthalmia.
• Conjuctival Xerosis (dryness of the conjuctiva - the white surface of the eye). The conjuctiva looks dry and slightly rough instead of smooth and shiny. Sometimes there are Bitot’s spots (white foamy patches) on it.
• Corneal Xerosis (dryness of the cornea - the part over the black and brown centre of the eye). The cornea looks dry and cloudy, although this is difficult to see. At this stage, the disease can get worse very quickly (within a few hours) and the child’s eyesight may be permanently damaged.
• Corneal ulcers. These look like little holes on the edge of the cornea. If not treated the child becomes partially or totally blind. Giving Vitamin A can cure the ulcers but sometimes scars remain which affect sight.
• Keratomalacia (soft cornea) This is quite rare.
The cornea becomes cloudy and soft like jelly, and the child is partially or totally blind. Occasionally the cornea breaks and the inside of the eye comes out.
Management of Vitamin A deficiency: Sometimes it is necessary to give Vitamin A supplements. See Fig. 7.14: Vitamin A Supplementation Schedule. Modified Universal Supplementation
| Target Group | Vitamin A (IU) Dose for Age | Number of Doses | Estimated Oil Drops |
|---|---|---|---|
| Mother within first month of delivery | 200,000 | 1 | 8 |
| Child at nine months | 100,000 | 1 | 4 |
Disease Targeted Supplementation:
| Disease Condition | Indication | Number of Doses | Given at: |
|---|---|---|---|
| Xeropthalmia | At any stage | 3 | First dose: At diagnosis |
| Measles | At any stage | 3 | Second dose: The next day
|
| Protein Energy Malnutrition | Kwashiokor
Marasmus |
3 | Third dose: 2-4 weeks later |
| Prolonged Diarrhoea | Diarrhoea lasting for 14 days or more | 3 | |
| Respiratory Tract Infections | Tuberculosis (TB)
Pneumonia |
1
1 |
At diagnosis |
Fig. 7.14: Vitamin A Supplementation Schedule
What are the consequences of VAD?
- Children who lack Vitamin A are more likely to die from infections such as measles or diarrhoea than are healthy children. These infections may cause a child to become more deficient in Vitamin A and develop xeropthalmia.
- Children with xerophthalmia may become partially or totally blind. Many of these children die. The ones who survive have difficult lives and may be a burden to their parents and community.
- Children with VAD do not grow at a healthy rate.
2) Iron deficiency Anaemia (IDA): When the diet is deficient in iron, anaemia is the result. Iron deficiency anaemia is common in many areas, and is particularly common towards the end of the first year of life when the infant grow rapidly and his/her stores of iron get exhausted while breast milk does not provide sufficient iron. (For more reading and information on IDA please refer to UNIT 10, Section 5: Anaemia).
3) Iodine Deficiency Disorders (IDD): Iodine is used by the thyroid gland to make a hormone called Thyroxine. Thyroxine controls normal physical growth and mental development. Iodine deficiency leads into low or no production of thyroxine and accompanying poor growth but most importantly, a reduced mental and physical development with the occurrence of more or less severe degree of brain damage. This condition, when it occurs, is called cretinism. Iodine deficiency causes other disorders including goitre (see fig 7.14), reduced fertility, miscarriages and stillbirth.
Fig. 7.15: Goitre. If a person with a goitre trembles a lot, is very nervous, and has eyes that bulge out, this may be a sign of toxic goitre. Medical advice is needed.
What are the causes of IDD? Unlike other chemical elements such as iron or vitamins, iodine does not occur naturally in specific foods. Iodine is present in the soil and plants obtain it from the soil. Iodine deficiency in the soil is caused by the environmental depletion of iodine and hence foods grown in these soils also lack iodine in them.
Iodine deficient soils are found in hilly/mountainous areas that are exposed to heavy rainfall and periodic floods whereby iodine is washed away from the soil or is leached from the soil. Hilly districts or those often affected by floods have this problem of lack of iodine.
Some foods contain chemicals called goitrogens that interfere with the absorption and use of iodine in the body. Cassava, particularly bitter cassava, contains a goitrogen and occurs in some parts of Kenya. Other foods such as millet, cabbage and kale contain small amounts of goitrogens that will make IDDs worse if people are already iodine deficient. This is why you often see people with goitre coming from same area.
Do you know why iodine deficiency is such an important problem? IDD is an important problem because, due to the reduced mental and physical development, it results in millions of children being unable to make the best use of their education.
Management of IDD: Iodine deficiency can be completely prevented by increasing iodine intake through adding iodine to salt in this country iodized salt is produced and used. In individual cases of goitre or hypothyroidism, both iodine supplementation and treatment with thyroid hormones are needed and are administered for at least 12 months. Prevention Public health measures to control iodine deficiency include:
- Administration of iodine tablets to school going children and pregnant women
- Iodization of local drinking water supplier.
- Inclusion of fish from the sea in the diet such fishes are rich in iodine.
THE ROLE OF THE HEALTH WORKER AND COMMUNITY:
You have now learned about the common nutritional disorders and their management. But you will find that you cannot manage alone to solve the nutritional problems in your community. What is your role, then, and that of the community, in prevention and control of malnutrition?
In all communities there will be people who are ready to help. Their influence should be put to good use. So, getting to know the people is the first step towards working together with them. Attend community meetings with them. This will give you an opportunity to present your problems and seek solutions. Arrange for periodic exchange of information with them. Such meetings also provide an occasion for discussing your progress. The people who can help in solving the nutritional problems are “formal” leaders: the local religious heads, school teachers, landlords, heads of small industries, women’s groups, farmers, civil servants and political leaders. You should tell these people the importance of nutritional problems. They must understand how they can help, and their co-operation must be won.
You should also seek the help of any government or private organisations working in your community. These will mostly include community development programmes and national nutrition supplementation programmes. You should also have close contact with the schools in your community.
Below are the critical areas in the prevention and control of malnutrition both in PEM and micro-nutrient deficiencies.
- Production and consumption of adequate amounts of food.
- Nutrition education
- Growth Promotion Monitoring
- Breastfeeding promotion
- Immunisation
- Safe water and sanitation
- Prevention of diarrhoea
- Family planning
- Female education
- Inter-sectoral collaboration
If all the things mentioned above are carried out in your community, then you will have gone a long way in the prevention and control of malnutrition in your area. But remember: most importantly you need the strong support of all other people in different fields of activity.
OBESITY:
Before we come to the end of this section, let's discuss yet another important nutritional disorder known as obesity.
What is obesity? Obesity means being too fat. This condition is now common in our society especially among the urban population. It results from eating more calories than the body needs, and the excess is stored as fat. Obesity is mentioned here because children who are overfed tend to become fat adults.
Associated factors: There are many factors that can affect the regulating mechanism of appetite and produce obesity. These factors include age, sex, pregnancy, economics, eating habits, physical activity, psychological factors, genetics, endocrine factors and overfeeding in children.
Some consequences of obesity (these are common later in life):
- Finds it difficult to dress well and look attractive.
- Flat feet and osteoarthrosis of the knees and hips are common
- Uterine prolapse
- Abdominal hernia
- Varicose veins
- Recurrent chest infections
- Diabetes mellitus
- Gout
- Atherosclerosis
- Peripheral neuropathy
- Hypertension
- Cerebral vascular accidents
- Cardiac failure
- Poor anaesthetic and surgical risk.
Management of obesity: An obese person must be motivated to lose weight. This motivation may be based on very individual factors, but every effort must be made to reinforce it and to support the client with advice and encouragement during the times when the goal appears more remote.
It is important that the members of the client’s intimate circle do not sabotage these efforts, either psychologically or physically, by encouraging the eating of prohibited foods.
- Diet should be altered to meet the physiological needs. Carbohydrate intake is reduced.
- Make a graph on which the client’s progress can be charted.
- Reduce salt intake.
- An increase in daily exercise is desirable. Walking a minimum of about 3 miles a day is encouraged.
7.7: NUTRITION SURVEY
Some food and nutrition problems tend to go unnoticed, even by those who live in the village or neighbourhood where they exist. A good way to find out about these problems is to take a simple nutrition survey.
Often the information collected through surveys serve the needs of the health authorities, but means little to the people themselves. Many people dislike surveys. This is especially true for the poorest of the poor who are repeatedly studied but seldom see any real benefits.
In this section, we are going to discuss steps in conducting a nutrition survey for children under age 5. But let’s begin by finding out why you would conduct a nutrition survey at all. A simple community survey to check for nutritional problems can perform at least four functions:
- It can help determine how many persons in their area are poorly nourished.
- It can show which children and which families have the greatest nutritional needs and deserve special care and concern.
- The health worker can use the survey to help inform, and involve various groups in the community, like mothers, fathers, school children and community leaders.
- The survey can provide a basis for comparison at a later date. People will be able to see if the action they have taken to improve nutrition in their village has been successful.
Different groups from the community can be involved in different aspects of a survey. However, if surveys are to be conducted by untrained people, they should be simple, quick and interesting.
| 19
Remember that it is usually easy to recognise the severely protein energy malnourished children in the community without taking measurements. How, then, would you recognise those whose malnutrition is not always obvious and yet they are the majority? ……………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………… ……………………………………………………………………………………………………………………… ……………………………………………………………………………………………
|
It is important to find those children who are malnourished but not easily recognisable and make sure they get the special care and food they need before they become seriously ill. Because it is not always obvious which children are growing well and which are not, some form of measurement is often helpful. Nutritional problems are complex in their causes. The types of information that can be useful in the assessment of nutritional status are numerous and diverse. They include:
- Clinical examination
- Anthropometric data
- Laboratory tests of nutritional status
- Dietary surveys
- Vital statistics
For the purpose of our exercise we shall only discuss anthropometric data. Because this data are commonly used, a dot for it has been placed on the chart. Clinical examination data is inclusive. This also seems to be the simplest, most reproducible, most reliable and least costly method for evaluating protein energy nutritional status.
We shall not discuss all the methods used in anthropometry. We shall only discuss the following:
- Weight for age
- Weight for height
- Mid Upper Arm Circumference (MAUC)
The precise measurement method you choose will depend on local resources, needs, and who does the measuring. You should also make sure that measurement and recording is done correctly and that the instruments used function properly.
1) Weight for age (using the Road to Health Chart): The weight of a child is the single most important anthropometric measurement that can be taken. In children its interpretation is dependent on knowing the age of the child. Weight should be taken with the subject nude or wearing a minimum of clothing.
The weights of many children can be put on a chart. See Fig. 7.16. Chart A is from the Ushago area where top civil servants live. Two clinical officers weighed 97 children in Ushago under the age of 3. A dot has been put on the chart for the weight of each child. You will see that Chart A has dots for the weights of 97 children under the age of three and that only 3 of the 97 children under age three fall below the Road to Health. This, therefore, indicates that malnutrition in young children is not a big problem in this village.
Chart B is from a village called Nyarugunga where people are living close together in mud-brick houses without enough water or proper drains or roads, and usually also without clinics or schools. Most of people who live in Nyarugunga are poor and many have no jobs. The weights of 76 children in Nyarugunga are shown on Chart B. you will see that 32, or nearly one/third (30%), are below the road to health. This village has a serious problem with the nutrition of young children.
By using a Road to Health chart in this way and putting the weights of many children on it, we are doing a community nutritional survey. But before we leave Road to Health charts, there is one more very important thing to say about them.
The information on the graphs is used to determine if children in a given area are well nourished and are growing. If the children are underweight and not growing, our job is to show their caretakers how to feed them. What matters most is the advice given, not charting the weight! However, weighing a child regularly and charting her/his weight will tell you if your teaching is succeeding. Caretakers should also be told to bring their child’s weight charts whenever they take the children to a health unit.
2) Weight for Height: For survey purposes, comparing a child’s height to his/her weight is perhaps the most accurate way to check whether or not he/she is too thin. A new thinness chart has been developed. It is colourful, simple to use, and easy to understand.
This is the way it is used:
- Weigh the child.
- Note the weight.
- Find the weight on the chart with your finger.
- Have the caretaker help the child to stand directly under your finger.
- Check to see that the child’s shoulders and feet are against the chart.
- Make sure that the child’s feet are against her weight as shown at the bottom of the chart.
- Now put your hand flat on the child's head. Which colour does your finger touch? Is the child in the upper red, lower red, yellow or green?
- If the child is in the upper red, he is dangerously thin and needs more food urgently.
- If the child is in the lower red, he is very thin and needs more food at once.
- If the child is in the yellow, he is thin and may need more food. Check him regularly.
- If the child is in the green, he is well nourished.
This chart is especially useful when children are measured only once, as in a survey.
Do you have this chart? If you don’t, ask your District Public Health Nurse if she could get you on.
3) Mid Upper-Arm Circumference: The thickness of a child’s upper arm is usually a good indicator of how well nourished he/she is.
The measurement of the circumference of the left upper arm mid way between the acromion process of the shoulder and the olecranon process of the elbow is being increasingly used as an index of nutritional status. This method is simple to use and easy to understand. It may be especially useful for village persons with little or no formal education.
This method does not provide us with information concerning nutritional status that is as reliable as the weight versus height measurement. However, it has the advantage of being inexpensive and usable where no weighing scale is available. Furthermore, between about 8 months and 5 years of age, the standard arm circumference increases very little.
An arm circumference of above 13.5 cm (green) can be considered normal for children from 1 to 5 years of age A measurement of between 12.5 cm (yellow) and 13.5 indicates moderate malnutrition and a measurement below 12.5 cm indicates more serious malnutrition. Measurement is performed on the left arm, which should be hanging freely. The measurement tape should be held gently but firmly so as not to press on the soft tissues (Fig. 7.17).
Where will you find a measuring instrument? If you have a tape measure, that is good. If you do not have one, a measuring instrument is easy to make. The directions are in Fig. 7.16.
Fig. 7.16: MAKING A MEASURING STRIP:
Now that you have learned about the three most common anthropometric measurements, we should also remember that however accurate and reliable they may be, measurements are of no use if they are not interpreted. This must be done at individual and community levels in view of making decisions, project implementation, and evaluation of actions.
Please consider these points if you do a simple survey:
a. Ask the permission of the village leadership first. b. Give each house an equal chance to be visited. c. Collect a little data well (use a questionnaire). d. Do not collect more data than you can analyse. e. Survey enough children. Usually 100 children is the smallest useful sample. f. Publish the findings of the survey. g. Give the community feedback (results of the survey). h. Plan for action with the community.
FIG. 7.17: Measuring upper arm circumference. You learned in Unit 2: Growth Promotion and Monitoring, that if you do not have a tape measure, you can use a string to measure the circumference. Then measure the string with a ruler.
Well done! You are now through the work of unit 7. Look back at the objectives at the beginning of the unit. If you feel you have understood them, do the attached perforated assignment but you can take a break first. By the way, are you planning to do the nutritional survey?
Keep up the good work!!
|
TUTOR MARKED ASSIGNMENT Personal File Number: Name: Address:
Answer all the questions. When you have finished, mail it to the correct address.
Case study Tuba, a boy, was born on 15th March 1996 in a health unit near his home. The birth weight was 2.8kg and he was the 6th child born in the family. In September Tuba was brought to the clinic with a fever which was treated. When the caretaker asked why she did not attend the young child clinic earlier, she said she was not aware that she should have gone. Tuba now weighed 7½kg and had not started a weaning diet yet. The caretaker was requested to start weaning immediately and continue bringing the child for regular growth promotion monitoring. The following month he weighed 7.8kg. In November he weighed 8.3kg, he was given measles vaccine and 100,000 i/u of Vitamin A. After completing the immunisation, the caretaker saw no good reason to return to the clinic. When the child got diarrhoea in April 1997, he was brought to the clinic and he weighed 7kg. The health worker advised the mother. In May the child was not brought because he had measles and they could not travel with the sick baby. They reported in June and the weight was unchanged: 7kg. Tuba was sent to the Nutrition Rehabilitation Unit. Advice was given. The child improved in the next 3 months: the weight was 7.3kg in July, 7.8 in August and 8.6kg in September. Tuba’s sister was born in October of that year. Plot Tuba’s weight on growth chart as described in the case study. 1.a) Which month would Tuba have started on weaning diet? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… b) Why was the child not brought early for immunisation? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… c) Was there any reason for special care? What? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… d) Why did the weight drop in October? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… 2. How would you manage a child, 2 years old, who is brought to your health unit with a weight of 7.5 kg? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… 3. Which other nutrition disorders do children have? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… 4. What are the consequences of severe marasmus or Kwashiokor in a child? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… 5. How much Vitamin A would you give to 5 year old child brought to the clinic with night blindness? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… 6. How much vitamin A would you give to an 8-month-old child with pneumonia who has, in the within a month, had a course of Vitamin A capsules for prolonged diarrhoea? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… …………………………………………………………………………………………………………
|
Congratulations! You have now come to the end of this unit.
When you have finished this assignment, post or bring it in person.. We will mark it and get it back to you with comments through the means indicated on your enrolment form.
Remember to indicate your Personal File Number, names and address accordingly.