Lesson 7: Malaria in Pregnancy
Contents
Introduction
Welcome to Unit 7 on Malaria in Pregnancy. So far you have learnt how to diagnose and treat simple and severe malaria, how to avoid treatment failure and errors in the management of malaria and also how to refer malaria patients. In this unit we shall learn how to manage malaria in a very important and vulnerable group in our society, that is, pregnant women. You will find the knowledge you have acquired so far in this course very relevant to the lesson of this unit.
Malaria is the number one cause of miscarriages among pregnant women and poses great danger to the mother and her unborn baby. The same type of parasites that cause Malaria infection in the rest of the population cause Malaria in pregnancy. Malaria is not sexually transmitted or caused by the unborn baby.
In addition to causing severe disease to the mother, malaria attacks the placenta thereby causing nutrition and growth defects and other negative effects to the unborn baby. This is often fatal if not attended to in time.
Malaria is more dangerous to women when they are pregnant because the parasites cause a pregnant woman to become weak and anaemic. Anaemia is dangerous to women during pregnancy and at childbirth because they often lose more blood. Anaemia during pregnancy can lead to death during delivery if the mother suffers from complications that cause a lot of bleeding.
Severe Malaria in pregnancy is a medical emergency requiring referral to hospital where intensive care can be offered.
One of the reasons why we have dedicated a whole unit to the discussion of malaria in pregnancy is because it can easily be diagnosed, treated and prevented.
.
|
By the end of this unit you should be able to:
|
lesson
Effects of Malaria in Pregnancy
Malaria in pregnancy can cause a wide range of effects. These range from health effects to the pregnant mother during and after pregnancy as well as to the unborn and newborn baby. Socio-economically the family is also affected.
Before you read on do Activity 1, it should take you 5 minutes to complete.
| 1
You may have managed Malaria in pregnancy in your unit. What are some of the effects of malaria to the following: (i) The mother …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… (ii) The unborn baby …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………
|
Confirm your answer as you read the following discussion.
In pregnancy, Malaria parasites hide in the placenta and interfere with the transfer of oxygen and nutrients (food) from the mother to her unborn baby. Malaria parasites may cause illness during pregnancy in the mother especially in primigravidae and women from non-malarious areas.
The following are some of the effects of Malaria:
• To unborn baby
- Abortion (miscarriage);
- Still birth (baby born dead);
- Preterm delivery (delivery before 37 weeks);
- Interference with the normal growth of the baby resulting in low birth weight, which is a risk factor for mental disability and newborn mortality.
• To the mother severe malaria may present with:
- Anaemia of varying degrees sometimes severe;
- Coma;
- Convulsions;
- Renal failure;
- Pulmonary oedema.
All the above are a risk factor during delivery.
- Now that you have learnt the effects of malaria in pregnancy, let us now turn to the management of simple Malaria in pregnancy.}}
Management of Simple Malaria in Pregnancy
A pregnant mother can have Malaria parasites and NOT show any signs of the illness. However, simple Malaria in pregnancy present with fever which may be mild and may sometimes be accompanied by any of the following signs and symptoms:
- Backache;
- Weak labour like pains;
- Nausea;
- Vomiting;
- Diarrhoea;
- Headache;
- Body weakness.
Simple Malaria is said to occur when all the above signs and symptoms or some of them occur. Such a patient is fully conscious and in control of all her senses and mental faculties. She is able to walk, sit, and talk. The blood film shows Malaria parasites.
|
Simple or mild Malaria in pregnancy can quickly change to severe and complicated malaria. Severe and complicated malaria is life threatening to the mother and baby. |
Before you read on do Activity 2, it should take you 5 minutes to complete.
| 2
1. What drug(s) have you been prescribing for the treatment of simple Malaria in pregnancy? …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… 2.In what drug dosages and duration have you been prescribing these drugs? …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… 3. What information did you pass on to the pregnant mothers when you gave the drugs above? …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… …………………………………………………………………………………… ……………………………………………………………………………………
|
Confirm your answers as you read the following discussion.}}
The treatment guidelines for Malaria in pregnancy recommend that many patients who are diagnosed with simple Malaria during pregnancy should first be treated with a combination of Fansidar (SP) in the following dose: Oral Fansidar (SP) (3 Tablets)–single dose
- In addition, the patient should be:
- Given Paracetamol 1g (2 Tablets) as a pain killer from day I to III, given every 8 hours;
- Supervised when taking the SP dose.
- In Kenya where the first line treatment has changed, pregnant mothers with simple malaria are treated with oral quinine
You should then give the patient the following piece of advice/information.
- Take adequate rest;
- Continue taking iron tablets;
- Stop folic acid for 1 week then resume thereafter;
- Complete the course of drugs as prescribed even after you feel better;
- Come back in 2 days time for review and reassessment;
- Take adequate oral fluids.
Here are some factors you should consider when giving oral drugs in pregnancy.
(i) Vomiting:
- If vomiting occurs within 30 minutes of taking the tablets, the patient should repeat the dose of Fansidar (SP) because she may have vomited the drug before it was absorbed.
(ii) SP (Fansidar) in pregnancy:
- Avoid giving SP (Fansidar) before 16 weeks and after 36 weeks of pregnancy because of possible damage to the baby;
- Patients allergic to Sulpha drugs should avoid SP (Fansidar);
- Do not give SP (Fansidar) if patient has had it within the last 4 weeks.
(iii)Temperature control:
- This is important. Use tepid sponging, fanning or paracetamol to achieve temperature control.
(iv) Drug interaction:
- Do not prescribe other sulpha drugs and folate with Fansidar (SP) together.
(vi) Follow up:
- If follow up at health centre is difficult, inform community health worker to visit the patient at home to check on her and give additional advice.
(vii)Diagnose treatment failure:
- If the patient does not improve within 24 - 48 hours of beginning treatment, or if the symptoms and signs return within a few days, you should refer the patient appropriately.
You have now learnt about the treatment of simple Malaria in pregnancy. Let us turn to management of severe and complicated Malaria in pregnancy.
Management of Severe and Complicated Malaria in Pregnancy
We hope you have noted that Malaria in pregnancy is a high priority medical problem. However, not every pregnant woman with Malaria should be referred to hospital. You should refer a pregnant mother to hospital only if she meets any of the following conditions:
- Has severe and complicated Malaria or signs and symptoms suggestive of severe Malaria. Can you remember the signs and symptoms of severe and complicated malaria? If you have forgotten review them again in Unit 4.
- Has taken Fansider (SP) within the last 4 weeks but still comes with Malaria or symptoms and signs of Malaria disease;
- Has Malaria and is less than 16 weeks or more than 36 weeks of pregnancy;
At the referral facility, the woman will receive treatment with the second line drugs. The 2nd line drug of choice is Quinine, which is given orally, intramuscularly, or intravenously.
The dose is 10mg/kg body weight every 8 hours for 7 days or for 3 days then a single dose of SP (Fansidar) given on the 4th day.
If the patient is in the 1st trimester or is beyond 36 weeks of pregnancy, avoid SP (Fansidar) and continue with Quinine.
Please note once again that severe complicated Malaria is a medical emergency. It should only be managed by experienced health care workers in a well-equipped clinic or hospital.
If you work in a health centre or dispensary, your role in the management of severe and complicated malaria should be to:
- Promptly recognize the condition i.e. severe complicated Malaria;
- Arrange for immediate transfer to the nearest hospital.
Give pre-referral treatment as follows:
- Give quinine as first line before referring her to the hospital;
- Give the patient full prescription and referral information;
- If you have an experienced health worker in your health unit, who has the knowledge and skills of managing severe Malaria using Quinine tablets or injection, let him or her know about the patient.
Once the patient gets to the referral hospital, in addition to antimalarial drug therapy, health care workers there will detect and manage other complications of severe malaria, such as:
- Anaemia, hypoglycaemia, fluid and electrolyte imbalance;
- Controlling convulsions;
- Detecting and managing kidney failure; etc.
Figure 2: Pregnant mothers admitted with severe Malaria.
You now know how to manage severe and complicated Malaria in pregnancy. Let us now discuss intermittent presumptive treatment of Malaria in pregnancy.
Intermittent Presumptive Treatment (IPT) of Malaria In Pregnancy
This is a new and effective treatment policy that has been introduced in the health care of pregnant mothers using Fansidar (SP) to treat Malaria.
Before you read on do Activity 3, it should take you 3 minutes to complete.
| 3
Have you heard of Intermittent Presumptive Treatment (IPT) of Malaria? Briefly state what it means. ………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………
|
Intermittent presumptive treatment (IPT) of Malaria during pregnancy is based on the assumption that every pregnant woman living in an area with high Malaria transmission has Malaria parasites. The parasites live in her blood or placenta, whether or not she has symptoms and signs of Malaria.
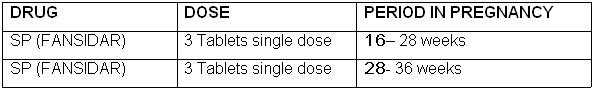
Therefore, the Ministry of Health recommends that ALL pregnant mothers should be treated with at least two doses of Fansidar (SP) during the second trimester (16-28 weeks) and third trimester (28-36 weeks) of pregnancy.
As we already mentioned, ALL pregnant women should get IPT. However priority should be given to those with the following:
- Low parity (1st and 2nd pregnancies);
- HIV positive;
- Between 10 – 24 years of age;
- Sickle Cell Anaemia
- Unexplained anaemia during pregnancy;
- Those living in areas where Malaria is less common;
- Those who migrated from low Malaria transmission areas.
How is IPT administered?
IPT is administered according to the following schedule.
During antenatal care clinic (ANC), you should supervise mothers swallowing the SP (Fansidar) through the Directly Observed Treatment (DOT) method.
If this is the first time you have learnt about IPT, we hope that you have understood the concept well and that you can apply it effectively. Next, let us look at how you can use information, education and communication massages to provide health education to pregnant mothers.
Information, Education and Communication (IEC) Messages to Pregnant Mothers
All pregnant mothers should be educated and counselled about Malaria during their routine visits to the antenatal clinic or when they come to your health facility suffering from Malaria.
Before you read on, do Activity 4, it should take you 5 minutes to complete.
| 4
What messages would you pass on to a pregnant mother who comes to attend ANC at your health facility? …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… …………………………………………………………………………………………… ……………………………………………………………………………………………
|
I hope in your answer you indicated that you would give them the following messages:
- Malaria is caused by a parasite transmitted by Anopheles mosquito.
- If a pregnant woman has Malaria, the parasites invade the blood, liver as well as the placenta;
- The unborn baby is affected by malaria because the Malaria parasites interfere with the normal functioning of the placenta. This can result in abortions, missed abortion, low birth weight babies;
- Malaria is even more dangerous for women when they are pregnant because it can develop complications such as anaemia, which put the life of the mother and baby at risk;
- Pregnant mothers should come to the health facility immediately they develop fever for treatment;
- They should share correct information on Malaria with other pregnant women in the community and inform them to seek early medical attention.
Well, we hope you are now knowledgeable about the IEC messages to give to pregnant womenz. Before we wind up this unit, let us see how malaria can be prevented and controlled during pregnancy.
Prevention and Control of Malaria during Pregnancy
There are many reasons why a pregnant woman would want to protect herself and her baby from malaria. By so doing she is able to live a healthy life, to carry her pregnancy to term and to give birth to a healthy baby. It is therefore very important that we explain to her how she can prevent and control this disease..
Before you read on, do Activity 5, it should take you 5 minutes to complete.
| 5
|
In this country and indeed most African countries, the control and prevention of Malaria is based on the following four (4) elements. These are:
- Intermittent Presumptive Treatment (IPT), with SP (Fansidar)
- Use of Insecticide treated mosquito nets (ITNs)
- Proper and timely management of women with symptoms and signs of Malaria infection.
- Health education and counselling of all pregnant mothers about Malaria during pregnancy.
Conclusion
You have now come to the end of this unit. In this unit we discussed Malaria in pregnancy. We saw that malaria can cause miscarriages (abortions) in Africa and it affects the mother and her unborn baby. It is actually more dangerous in pregnant women than in non-pregnant females or adult males. We also looked at the treatment of simple and severe malaria in pregnancy, the concept of IPT, and how malaria can be prevented. Prevention of malaria in pregnancy involves preventing mosquito bites through the use of ITN, as well as use of Fansidar (SP) for chemoprophylaxis as part of Intermittent Presumptive Treatment. Remember to give all pregnant mothers IEC messages on malaria so that they can be well informed.
Well, its now time again for you to review the learning objectives we outlined at the beginning of this unit. Go through them and see if you have achieved them. If there is any objective you are not sure about, read the relevant section in this unit again. If you feel confident that you have achieved all of them, complete the attached assignment and send it to us. Do not forget to do the practical exercises given below.}
| Things to do in this unit
1. Assess a pregnant mother with fever and in particular do the following:
Record all your findings, advice given and the treatment you prescribe on paper and send it to the tutor. 2. Give pregnant mothers attending antenatal care (ANC) key messages on Malaria disease.}}
|
|
Student Names:__________________________________ Student Identification Number:_______________________ Student Postal Address:__________________________ __________________________
1.List down signs and symptoms of severe Malaria in pregnancy. ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… …………………………………………………………………………………
………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… …………………………………………………………………………………
………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… 4.What drugs are used for: - (i) First line treatment of simple Malaria ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… (ii) Treatment of severe complicated Malaria in pregnancy. ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… ………………………………………………………………………………… …………………………………………………………………………………
Time spent doing the assignment: Hours …………………. Minutes ………….. |
Enjoy the rest of the course!