Lesson 5: Growth and Development
Contents
INTRODUCTION:
Welcome to Unit 5 of the Child Health Course. In the previous unit, you learnt about the common health problems of the new born. We hope you found it interesting and informative. In this unit, you will learn about child growth and development, factors that influence growth and development and what can be done to promote optimum growth and development.
5.1: GROWTH AND DEVELOPMENT
Before you proceed, do the following activity.
| 1
……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Confirm the answers as you read the following discussion.
Definition of growth and development
Growth is the progressive increase in the size of a child or parts of a child. Development is progressive acquisition of various skills (abilities) such as head support, speaking, learning, expressing the feelings and relating with other people. Growth and development go together but at different rates.
Importance of assessing growth and development
The assessment of growth and development is very helpful in finding out the state of health and nutrition of a child. Continuous normal growth and development indicate a good state of health and nutrition of a child. Abnormal growth or growth failure is a symptom of disease. Hence, measurement of growth is an essential component of the physical examination.
Factors affecting growth and development
Each child’s path or pattern of growth and development is determined by genetic and environmental factors. The genetic factors determine the potential and limitations of growth and development. If favourable, the environmental factors, such as adequate nutrition, facilitate the achievement of the genetic potential of growth and development. Unfavourable factors, acting singly or in combination, slow or stop growth and development. Some of the unfavourable factors are malnutrition, infections, congenital malformations, hormonal disturbances, disability, lack of emotional support, lack of play, and lack of language training. To promote optimum growth, these environmental factors can be removed or minimized. Once they are removed, there follows a period of catch up growth. During this period the growth rate is greater than normal. This growth rate continues until the previous growth pattern is reached. Then the growth rate is reduced to the normal rate determined by the individual’s genetic factors. A child genetically determined to be tall grows slightly more rapidly than a child genetically determined to be short. Similarly, a child genetically determined to be clever develops their intellect more rapidly than a child genetically determined to be less intelligent.
Let us now find out how we measure growth.
Measuring Growth
There are various measurements that are used to measure growth. These are:
- weight,
- height,
- head circumference,
- mid upper arm circumference (MUAC)
- the eruption of teeth.
To be useful, these measurements must be taken accurately using reliable equipment and correct measuring techniques.
Measuring weight For measuring the weight, a beam balance or spring balance is used. Before weighing a child, check the weighing scale to ensure it is working properly. You can do this by weighing a known weight and noting whether the scale has obtained the same weight. Then proceed as follows:
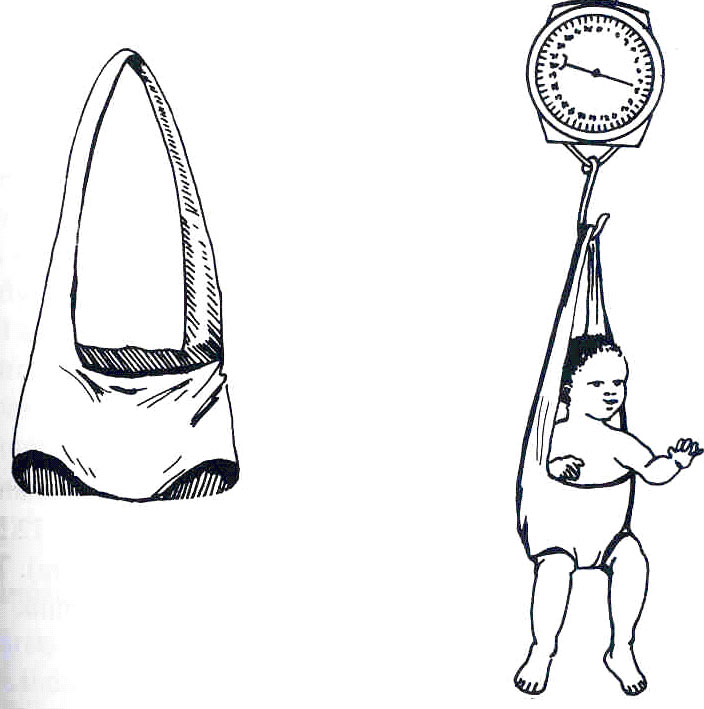
- Hung the scale securely with the dial of the scale at your eye level for correct reading. If you use the Salter scale, hang the weighing pants on the hook of the scale. See figure 5.1.
- Adjust the pointer of the scale to zero (“0”) by turning the knob on the top of the scale to account for the extra weight of the weighing pants;
- Ask the parent to remove any heavy clothes and shoes including the nappies and to dress the child in the weighing pants. .
- Once the child wears the weighing pants, ask her to lift the baby and fasten the loop of the pants to the hook of the weighing scale. Ask the mother to let go of the child but to continue standing nearby and talk to keep talking to the baby. The child’s feet should be off the ground as shown in figure 5.1.
- If the child is upset, ask the mother to calm him or her. When the child stops moving, note the weight quickly, reading to the nearest 10gm in infants and 100 gm in children.
Fig 5.1 Measuring weight using a spring balance
Measuring the Head Circumference The head circumference is measured by encircling the head with an unstretchable tape measure, or a piece of string in the absence of a tape measure. This is passed over the most prominent part of the occiput posteriorly and just above the supraorbital ridges anteriorly to obtain the greatest distance around the head. The piece of string used in the absence of a tape measure is then measured with a ruler to obtain the head circumference (see Fig 5.2).
Fig. 5.2 Measuring the head circumference.
Measuring the mid upper arm circumference (MUAC) The mid upper arm circumference is measured using a tape or string in the absence of a tape. The tape or string is placed around the upper arm, midway between the olecranon and acromion processes. Care is taken not to pull the tape or string too tightly. The measurement is read. The string used in the absence of a tape measures is then measured with a ruler to obtain the mid upper arm circumference. Figure 5.3 illustrates how to measure the mid-upper arm circumference.
Fig 5.3. Measuring the mid upper arm circumference.
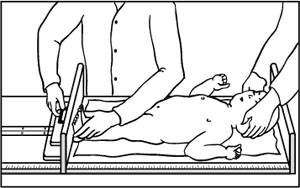
The length of a child is measured in the first 3 years and the height is measured after 3 years of age. The length is measured using a horizontal measuring board put on the ground or on a table. The child is laid on his back with the head against the fixed head board. A helper holds the child’s head so that the eye angle- external ear canal line is vertical and also keeps the body straight. With one hand of the health worker, the child’s knees are pressed down to straighten the child’s legs fully while, with the other hand, the sliding foot board is placed to touch the child’s heels firmly. With the foot board in place, the child’s length is read on the metre scale. Fig 5.4 illustrates how the length of a child is measured.
To measure the height, a bare foot child stands with the feet together. The heels, the buttocks and the occiput lightly touch the measuring device. The head is aligned so that that the external eye angle- external ear canal plane is horizontal. The child is told to stand tall and is gently stretched upward by pressure on the mastoid processes with the shoulders relaxed. The sliding head piece is lowered to rest firmly on the head. The height is read and recorded.
Fig 5.4 Measuring the length and the height.
Weight Growth Pattern
Table 5.1 below shows average growth measurements of a normal child. Learn them by heart so that you do not have to look in a book to find out how much a child of a certain age should weigh.
Table 5.1 Average growth measurements of normal children.
| Age
Years |
Weight | Length | Mid Upper Arm Circumference (MUAC) |
|---|---|---|---|
| Birth | 23.5 Kg | 50 Cm | |
| 6 Months | 7.0 Kg | ||
| 1 Year | 10.0 Kg | 75 Cm | 16 Cm |
| 2 Years | 12.0 Kg | ||
| 3 Years | 14.0 Kg | ||
| 4 Years | 16.0 Kg | 100 Cm | 17 cm |
| 5 Years | 18.0 Kg |
An average term newborn weighs 3.5 kg (range 2.5 kg- 4.6 kg). The birth weight must be plotted in the first box of the growth chart and recorded in the appropriate space on the growth chart. The birth month should be written in the first box of the growth chart. Within the first 3-4 days, a term newborn loses 5-10 % of the birth weight. This weight loss is usually regained in 2 weeks by term babies and longer by premature babies. An average term baby doubles the birth weight in 4-6 months, triples it by one year and quadruples it by two years of age.
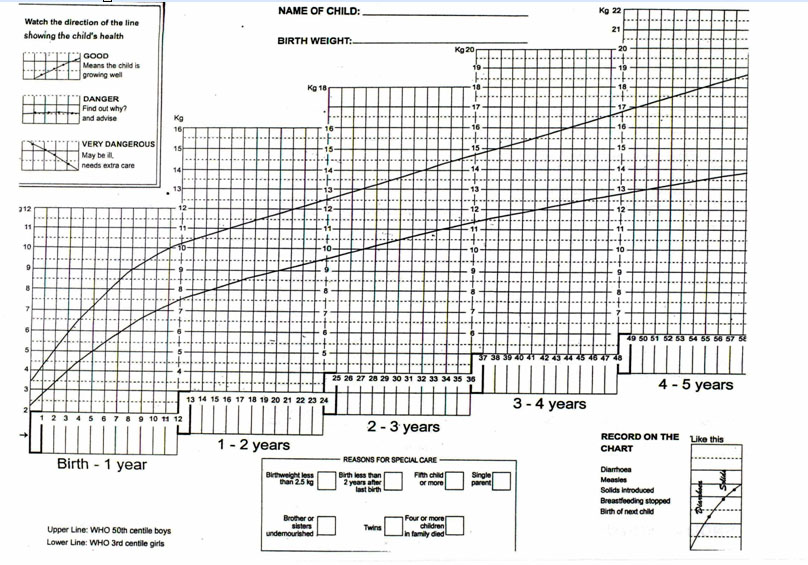
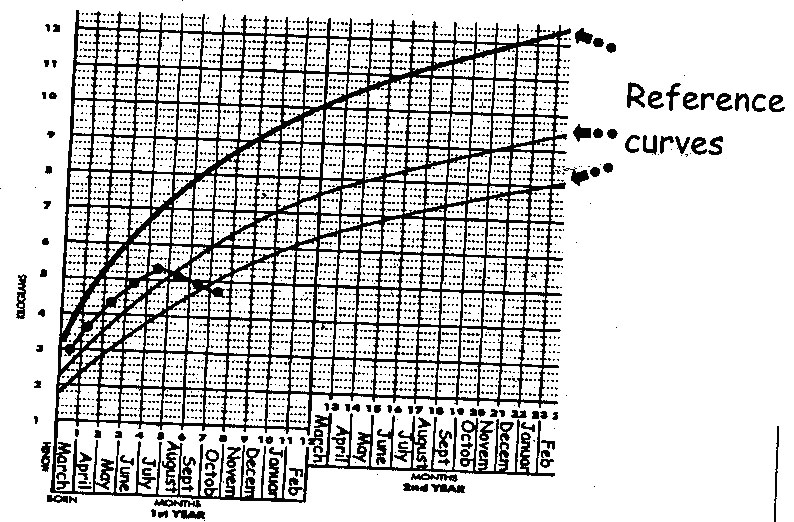
Growth Monitoring Growth monitoring is the process of maintaining regular close observation of a child’s growth. It starts with measurements of weight daily, weekly, monthly, bimonthly etc. The successive weights are plotted on the growth chart of the child health card. To monitor growth, you must use the growth chart on the back of the child health card. You need to study a blank growth chart to be thoroughly familiar with its contents (see figure 5.5 ). To start with, note: the top line represents the average growth line of healthy boys and the bottom line is the 3rd percentile for girls (the lower limit of normal weight-for-age of healthy girls).
To determine an individual child’s growth pattern, weight measurements from birth are plotted on the growth chart of the child health card. The plotting produces a line or graph. This line constitutes that individual child’s growth pattern or curve.
Fig. 5.5: Road to Health Chart
| 2
Ouma was weighed on three occasions. In first week of March 1989, he weighed 6 kg, in the second week of May 1989 weighed 7.5 kg and in the second week of July weighed 8 kg. Using this information, plot Ouma’s growth on a graph paper, squared paper or actual growth chart of child health card. Is Ouma’s growth adequate? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… Why do you say so? ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Compare your answers as you read the following discussion.
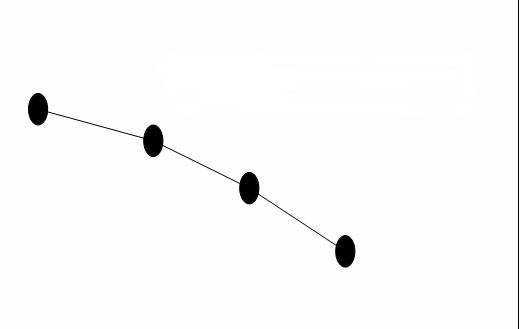
Ouma’s growth curve is constantly going upwards as shown in Figure 5.5 below. A constantly upward curve parallel to the printed lines shows GOOD growth. You should inform the mother or caretaker that the child is growing well and praise her for her good efforts.
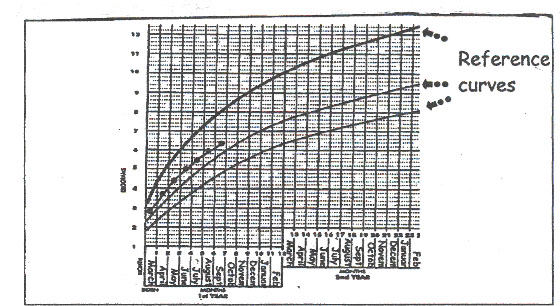
Figure 5.5: Upward growth curve indicating good growth.
By looking at the direction of the child’s growth curve, the healthworker and the mother can see at a glance whether the child is gaining weight appropriately or not. Let us briefly look at how to interprete a child’s growth curve or pattern..
Interpretation of the growth curve It is important to know how to interpret the individual child’s Growth Curve or pattern on the Child Health Card. Interpretation simply means determining whether the child is growing appropriately or not. The interpretation is done by watching the direction of the child’s growth pattern. The direction of the growth curve indicates how the child is growing.
The weight growth pattern of the larger term infants will be above the pattern of the average term infant. On the other hand, the weight growth pattern of the smaller term infants will be below the pattern of the average term infant. A small baby whose growth pattern is below the bottom line in the growth chart is healthy if that child’s growth pattern is parallel to the bottom percentile line. As long as the baby is gaining weight, however, at an acceptable rate, the mother should not worry
A horizontal (flat) growth curve like the one in Fig. 5.6 means DANGER! It means the child is not growing and is a sign of disease, especially malnutrition. A child who is malnourished cannot grow properly, cannot resist diseases, and is in danger of getting killer diseases. You should take a thorough history from the mother to establish the cause of growth failure and then advise the mother. You should also encourage the mother to give the child food containing enough calories, protein, vitamins and minerals.
Fig 5.6: A static growth curve
A curve deviating downwards, as shown in Fig. 5.7 indicates a VERY DANGEROUS situation. The child is losing weight. The child needs extra care immediately. The baby may be suffering from malnutrition, tuberculosis, AIDS or other medical conditions. The mother is advised to take the baby to hospital for investigations and treatment.
Any infant who does not gain weight for one month or a child who does not gain weight for two months should receive urgent attention. Such an infant or child is becoming malnourished.
Fig. 5.7 A downward growth curve
Fig. 5.8 is an illustration of the growth curve of another child called Juma. Juma was growing well until about 4 months of age. From this point, the growth curve started being flat. The horizontal deviation indicates static growth. This is not good and action should have been taken by the health worker and the parents of the child earlier.
After 4 months of age, the child’s growth curve even began to go down. At this point the child was in a very dangerous position. Then the growth curve began to go upwards again, which meant that the child was gaining weight once more.
Fig 5. 8 Juma’s Growth curve.
As illustrated at the bottom right hand corner of the growth chart in Figure 5.5, you should record important events that affect the child’s growth above the curve in the Growth Chart. Such events include diseases, weaning, introduction of solids and stopping of breastfeeding.
Importance of Growth Monitoring:
Health workers and parents should monitor the growth of children for the following reasons
- For early detection of abnormal growth and development
- To facilitate the early treatment or correction of any conditions that may be causing abnormal growth and development.
- To provide an opportunity for giving health education and advice for the prevention of malnutrition.
Reasons for special care At the bottom of the Growth Chart there is a box that lists some of the factors that may make a child particularly vulnerable to malnutrition. A tick or mark should be made next to any of the reasons that apply. This will then remind you to be particularly alert to any signs of growth faltering and may suggest the reasons for poor growth. You can then plan how best to help this particular child. Note that regular weighing of infants (monthly) and young children (at least once every two months) will help you to detect growth failure and prevent malnutrition. Such growth monitoring should be continued up to the age of 5 years as a component of well child care. Encourage parents to have their children weighed and avoid keeping them waiting for too long. You must always report the findings to the mother or caretaker and inform her how the child is growing.
Do you have a child who is under five years of age? Do you weigh him regularly? You should encourage parents to monitor their children’s growth and development in the first 5 years. But first and foremost you should serve as a good example.
Head Circumference Growth Pattern.
The head circumference measurements are used for estimating the growth of the brain. At birth, the head circumference of a term baby averages 34 cm (see Table 5.2). The head circumference grows most rapidly in the first year: 2 cm monthly in the first 3 months, 3 cm during the next 3 months, and 3 cm in the last 6 months. This means that the average head circumference is 44 cm at 6 months and 47 cm at 12 months of age. Thus, the head circumference grows by 12 Cm during the first year.
Table 5.2 Average and range of head circumference and the average length/height of children
| Age | Head circumference | Length/height | ||
|---|---|---|---|---|
| Years | Months | Average | Normal range | Average |
| 0 | 34 cm | 32-37 cm | 50 cm | |
| 1 month | 36 cm | 34-40 cm | 55 cm | |
| 2 months | 38 cm | 36-41 cm | 58 cm | |
| ½ year | 3 months | 40 cm | 37-43 cm | 60 cm |
| 4 months | 41 cm | 38-44cm | 62 cm | |
| 5 months | 42 cm | 39-45 cm | 64 cm | |
| 6 months | 43 cm | 40-46 cm | 66 cm | |
| 7 months | 44 cm | 41-47 cm | 68 cm | |
| 8 months | 69 cm | |||
| 9 months | 45 cm | 42-48 cm | 71 cm | |
| 10 months | 72 cm | |||
| 11 months | 73 cm | |||
| 1 year | 12 months | 47 cm | 43-50 cm | 75 cm |
| 1 ½ years | 18 months | 47 cm | 44-51 cm | 81 cm |
| 2 years | 24 months | 48 cm | 45-52 cm | 87 cm |
| 2 ½ years | 30 month | 49 cm | 46-53 cm | 92 cm |
| 3 years | 36 months | 50 cm | 47-54 cm | 96 cm |
| 6 years | 51 cm | 48-55 cm | 116 cm | |
| 9 years | 52 cm | 49-56 cm | 133 cm | |
| 12 years | 53 cm | 50-57 cm | 148 cm |
Mid Upper Arm Circumference Growth Pattern:
The measurements of mid upper arm circumference (MUAC) are used for determining whether the child is well nourished or malnourished.
The mid upper arm circumference increases fairly rapidly to about 16 cm by the age of one year. In the period 1 to 5 years, the mid upper arm circumference increases by only 1 cm. So, irrespective of age, the mid upper arm circumference of well nourished children ranges 16 -17 cm in the period 1-5 years. Conversely, if the mid upper arm circumference of a child of 1 to 5 years of age is less than 16 cm, that child has malnutrition and corrective intervention should be carried out.
Length/ Height Growth Pattern
An average term baby is 50 cm long. The length increases by 50% in the first year. In the second year, the average height growth is about 12 cm. The birth length doubles by 4 years of age. After the second year of age, the annual height growth averages 5-6 cm until the beginning of the adolescent growth spurt. Height growth stops at about the age of 18 years in girls and at the age of about 20 years in boys.
After plotting the child’s height or length on a height chart, you should determine whether the growth pattern is normal. A normal growth pattern is parallel to the printed percentile lines.
There are also weight for height charts and tables. Weight for height below the fifth percentile is a good indicator of acute under nutrition. Another way you can measure growth is eruption of teeth but remember that this is not very reliable as it varies from child to child. All the same, let us briefly discuss too eruption as an indicator of measuring growth.
Tooth Eruption as an Element of Growth:
Start by doing the following activity. It should take less than 3 minutes to complete.
Compare your answer with mine.
Tooth eruption is an important part of growth. In general, teething in infants usually starts at about 6 months of age, but some start later than 6 months. A new tooth appears approximately every month so that by 2 - 2½ years of age the baby will have 20 primary teeth. This makes the number of teeth roughly equal to age in months minus 6.
A parent should only start to worry about tooth eruption if a child has not yet started teething by 13 months. This is because at this age the child should be eating solid foods. Breast milk alone is not enough after the age of 6 months.
Teething may cause excessive salivation, irritability, disturbed sleep and some pain. Sometimes it also causes diarrhoea.
At the age of about 6 years, the shedding of the primary teeth starts and continues through to the age of 12 years. Eruption of permanent teeth starts at about 6 years of age.
So far we have discussed growth and how to measure and monitor the growth of children. Next let us discuss development. Can you recall how we defined development?
DEVELOPMENT
At the beginning of this unit, we defined development as the progressive acquisition of various skills (abilities) such as head support, speaking, learning, expressing the feelings and relating with other people. We also said that each child follows a unique path in growth and development that is laid down from the beginning of life by what he has inherited from both parents. If a child is genetically determined to be clever, then development will be more rapid. Unfortunately, many things may change the genetically determined path of growth and development. These things include, for example, infections, lack of care, psychological trauma, bad education, and malnutrition, to mention just a few.
The normal well-fed infant who is protected from infections develops quickly, particularly during the first 3 months. This is shown in Table 5.3. It is very important to know the age ranges when most children acquire certain skills. The various skills the baby and a young child learn are called milestones. In monitoring development, we notice at what age the child achieves various milestones, such as smiling at the mother, sitting without support, grasping objects with his/her hands, standing, walking and talking. You should record at what age the child has achieved the various milestones.
Still, it is important to remember that every child develops at his/her own rate or pace. Some walk early, others late. The average age ranges at which children reach various milestones is given in Table 5.3. The individual child’s development rate often differs widely from the average but it is still be quite normal. The individual child’s development is normal if the rate of development is constant and the developmental pattern is within the normal range.
Table 5.3: Normal Development Milestones
| Age range | Motor Development | Language and social development |
|---|---|---|
| Birth | When prone turns head to one
side to avoid suffocation |
Cries |
| 3-6 Months | Good head control | Can follow an object with eyes,
plays with hands |
| 6-9Months | Can sit unsupported | Grasps actively, makes loud noises |
| 9-12Months | Able to stand | Understands a few words, tries to use them |
| 9-18Months | Able to walk | Grasps small objects with thumb and index finger |
| 15-30Months | Able to run around as much as he wants | Can say several words or even some sentences |
| 3 Years | Plays actively, is able to jump and climb | Starts talking a lot, is curious and
asks many questions |
FACTORS THAT PROMOTE DEVELOPMENT
Before you continue reading complete the following activity.
| 4
1. ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… 2. ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… 3. ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Now confirm your answer as you read the following discussion.
The factors that promote development include good nutrition, emotional support, play and language training. We shall discuss each of them in detail, starting with good nutrition.
Good nutrition: Good nutrition is essential for normal growth and development. Unlike most other organs in the body, the brain is not fully developed at birth. Good nutrition in the first 6 months of life is extremely important. Malnutrition in this period may inhibit the growth of the brain. As a result of impaired brain growth, the child may suffer for the rest of life if the child does not get enough good food. A malnourished child is often tired, apathetic and not interested in learning new things that will promote normal development. Nutrition is discussed in detail in Unit 7
Emotional Support: The first 5 years of life are critical for the foundation of the skills which are developed in the following periods of the child’s life. A newborn starts with no knowledge and learns a great deal during his/her first year of life. It is very important to realize that a child is a growing and developing human being right from birth. He ought to be treated very carefully, with love and respect, so that he can develop normally. He needs full emotional support. There are eight basic needs for a healthy emotional development of a child.
These are:
- Love;
- Security;
- Acceptance an an individual;
- Self-Respect (Self-Esteem);
- Achievement;
- Recognition;
- Independence;
- Authority.
Let us briefly look at each in detail.
Love A child needs to feel loved continuously. A child who does not feel loved will not develop properly, and will not learn as quickly as other children. Instead, he becomes sad and lonely and no longer interested in what goes on around him.
Security A child needs to feel safe. He can only feel safe if his parents show that they love him and take good care of him. He must know that his parents will look after him and help him, that they will feed him when he is hungry, play with him, and keep him happy and comfortable. The love and security a child gets from the mother and family helps him to develop a sense of trust in people, initially the family members and later people outside the family.
Acceptance as an individual: A child enjoys being accepted as an individual. A child needs to know that his mother and family love him for what he is. They should not compare him with other children and tell him that he is slow to do this or that, or that he is not as good as some other child. They should show him that they respect him as an individual with his own likes and dislikes, and that they realize he is unique, as all children are unique.
Self respect (self-esteem). Children need to feel that they are of great value, they are able to do things by themselves, they can achieve success, and that their success will be recognized. Anything suggesting that a child is inferior is very disturbing to the child.
Achievements The child feels the need to achieve. The parents should not do anything that the children can do for themselves.
Recognition A child enjoys recognition by his or her parents. A child needs to know that his parents are happy and pleased when he has learned to do something new. Parents should help a child to do things and encourage him to make achievements. They should also teach the child because they love him and show that they are proud of him. This helps the young child to feel secure and to learn more easily.
Independence A child needs to learn how to make decisions. As the child grows he needs to be allowed to decide more and more things for himself and learn how to be independent. The parents must not unnecessarily limit the child’s independence and exploration by overprotection and over anxiety.
Authority A child needs his parents’ authority mixed with affection. The parents train the child to learn to obey the rules of the home, the neighbourhood, the school and the society. The rules indicate what the child may do and what he may not do. What a child may do is approved and encouraged with rewards. What the child may not do is clearly and firmly disproved and discouraged. The discouragement is achieved by permitting consequences of undesired behaviour. The child thus learns to accept the restrictions that are there in life.
Play Play is an essential factor the development of a child. Play is an irreplaceable source of information, stimulation for the brain, stimulation for the muscles and a lot of fun. All these are necessary for physical, mental and social development. All normal children like to play. If a young child does not play, he may be ill. Encourage playing, even if it may be noisy sometimes.
Expensive toys are not necessary for play. Young children will improvise toys from common objects such as paper (but not plastic bags), sticks and stones. The parents should make sure the child does not injure him/ herself with any of the toys. For example, parents should ensure that a toy is not too small, as a child can easily choke on small objects. To help a child play and learn properly, he needs to have:
- Plenty of room so that he can move about and discover things for him/ herself.
- Independence. He should be encouraged to do things he wants or enjoys.
- Several different kinds of toys so he can practise different skills. Blocks of wood can be used for stacking, a ball for throwing, containers of water or sand for filling and pouring.
- Encouragement and interest from the adults. It is fun to play together.
There are different kinds of play, and each type helps a child to develop properly.
Physical play: This exercises the body's large muscles and keeps the child healthy and strong. Physical plays include: running, jumping, climbing, and swimming.
Manipulative play: This is a kind of play in which the child uses the hands and the eyes. It teaches such things as the size, consistency, texture, shape and colour of objects. Things for manipulative play include: sand, earth, clay and water. Children enjoy playing with all these things.
Creative play: Painting, paper cutting, sewing, using crayons, threading beads and shells, clay modelling, and building with bricks or blocks of wood are all activities that help children to use their hands and eyes together to make things which were not there before.
Imitative play helps the child to acquire the skills of being a person. Through imitating the sound, the child acquires speech. Imitating everything, the child acquires many skills: dressing, feeding, washing etc.
Imaginative play: The child can dress up and pretend to be an adult whom he knows, or pretend to be a driver driving a car. . Children can even pretend that they are animals. This sort of play is important because it allows young children can get rid of a lot of feelings of anger, anxiety and fear.
Language Training Another factor that promotes development is language training. Children should be offered opportunities to meet, use, and play with words in conversation and in reading books. Using an adult language, the adults should talk and sing with small children and infants, encourage them to talk about what they are thinking, not laugh when children are talking, read to the children, tell stories, and listen as attentively to the children as they listen to the other adults. Try to understand how they are thinking and be happy that they want to involve you in their world.
You now know what growth and development are and the factors that promote them. In the following section we shall discuss the importance of antenatal care, perinatal care and postnatal care and the effects of not having these services.
5.2 THE IMPORTANCE OF ANTENATAL CARE, PERINATAL CARE AND POSTNATAL CARE.
Start by doing the following activity.
I hope in your answer you mentioned that a pregnant woman needs good quality antenatal, perinatal and postnatal care, not only for her own well being, but also for that of her unborn child. We shall discuss the importance of antenatal care, perinatal care and post natal care separately, starting with antenatal care.
ANTENATAL CARE
Antenatal care is the health service given to a pregnant mother from the time she recognizes the pregnancy until the onset of labour to keep her and her baby healthy.
- Good antenatal care is the best health insurance for both the unborn baby and the mother. Antenatal care is important because it:
- Promotes and maintains good physical and mental health of the pregnant woman. It also helps to ensure that the mother delivers a mature, live and healthy baby.
- Helps in the avoidance of hazards (smoking, alcoholism).
- Prepares the mother for labour, lactation and subsequent care of her baby.
- Helps in early detection and treatment of high risk medical and obstetrical conditions that would endanger the life or impair the health of mother or baby. These high risk conditions include pre-eclampsia, malpresentation, intrauterine growth retardation, post-maturity, and diabetes.
In order to achieve the above aims of antenatal care, we need to provide all the pregnant mothers with the antenatal services.
| 6
A pregnant woman comes to your health facility for antenatal care. What services do you think you should offer her? List them down in the space provided. ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
Now compare your answer with what follows.
During antenatal care, the following services are given to pregnant mothers:
Registration: A record of the mother's name, age, address and next of kin is made. The name helps us to identify the mother. The age helps us to plan for her delivery. Mothers who are below 15 years of age and those above 35 years of age with a first pregnancy need special care, especially during delivery. Find out about their address. This helps us to identify the areas that have high maternal deaths, neonatal deaths and infant deaths and to follow-up the patient.
History taking: History taking means asking questions about when the mother had her last menstrual period, the past medical history and past obstetric history. You will recall that Unit 1 we covered history taking of children in detail. You can apply the same principles when taking the history of a pregnant mother. As you know the information you gather should help you make decision.
For example, asking for the date of the last menstrual period will help in calculating the Estimated Date of Delivery (EDD). The past medical history helps you to plan how to manage the mother during pregnancy and labour in case she has any other medical conditions.
Some illnesses are made worse by pregnancy, for example, heart disease. Some illnesses, for example, hypertension and diabetes cause complications during pregnancy and may damage the baby. Some maternal illnesses, for example, AIDS and tuberculosis, are transmitted to the baby and manifest after birth. Therefore it is important to find out if the pregnant woman is healthy and if she has ever had any serious illness. Any pregnant mother who has had a bad illness or an abdominal operation should be referred to hospital.
The past obstetric history gives you information about past pregnancies and deliveries and any difficulties a mother has experienced. If a woman has had normal pregnancies and labour in the past, and has delivered healthy babies, she is likely to do the same this time too. However, if she has had difficulties in her previous pregnancies, she will often have difficulty again and is at high risk. Also, a mother who has had very many deliveries, even if they have all been normal, is at high risk. She is more likely to have a malpresentation or postpartum haemorrhage (bleeding after delivery).
General examination: It is important to look carefully at the mother as she comes into your health facility. Does she look healthy or does she look ill? Does she walk normally, or does she walk with a limp? You can achieve this thorough observation. A general examination, however, includes the following:
• Height: Measure the mother’s height. A mother whose height is below 150 Cm is considered to be short. If a mother is short, her pelvis may be small. A small pelvis may be associated with a difficult delivery if the baby is large. Height is measured only on the first visit.
• Weight: Measure the mother’s weight at each antenatal visit. Every pregnant mother is expected to gain weight during each visit. If a pregnant mother has no weight gain or has very little weight gain it may be due to poor feeding during pregnancy or it may be due to some disease. Measuring a mother's weight at each visit can help detect problems like intra-uterine growth retardation.
• Blood pressure: Measure the mother’s blood pressure at every antenatal visit. By taking a mother's blood pressure you can detect a condition known as pre-eclampsia. When a mother has pre-eclampsia, her blood pressure can be as high as 140/90 and above (the diastolic pressure is the most important one). The mother will also sometimes have swelling of the legs and there will be protein in the urine. It is very important to find and treat this condition early in order to prevent eclampsia later on. This condition may cause premature delivery.
• Look for anaemia: You look for anaemia by looking for pallor at the conjunctiva of the eye, the tongue, the gums, the nail beds and the palms of the hand. These places are normally pink in colour. When a person has anaemia, these places become very pale.
Practice looking at the conjunctiva in as many people as possible. Then you will easily see the difference between the normal and the anaemic. Anaemia is a very serious problem in a pregnant mother and severe anaemia puts the mother at high risk.
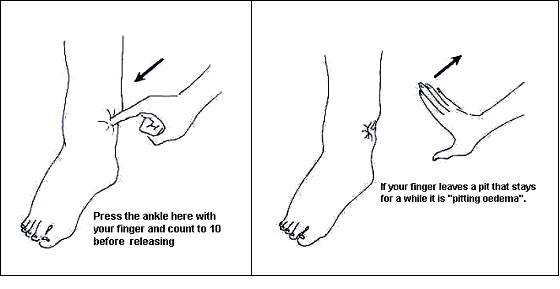
• Look for oedema: Examine the legs of every pregnant mother when she comes to the antenatal clinic and test for pitting oedema. Press your thumb over the lower part of the mother's leg and hold it there while counting to five. Oedema is present if the "pit" caused by the thumb remains after the thumb is removed. See Figure 5. 10.
Fig 5.10 An illusration of pitting oedema.
Oedema may be due to one of the following conditions:
- Hypertension
- Severe anaemia
- Heart failure
- Kidney disease
Severe oedema may be all over the body and not just in the legs. The mother's face and eyelids may look swollen and her hands and fingers may also be swollen.
- Examine the breasts: Examine the mother’s breasts and refer any woman with lumps to hospital. The breasts grow during pregnancy, getting bigger and firmer so that they are ready to produce milk when the baby is born. In primigravida, or a first pregnancy, the nipple and areola (the skin around the nipple) become darker.
Some primigravidae have flat or inverted nipples that do not stick out. These will improve when the baby sucks in the correct position – that is, if he takes the whole areola into his mouth. Women who have already successfully breastfed a baby are unlikely to have problems with breastfeeding.
- Examine the abdomen: The examination of the abdomen has many components.
First, look at the abdomen (inspection). Pay special attention to the following:
- Are there any scars?
- Has the woman had a caesarean section or some other abdominal operation? If yes, refer her to hospital for delivery.
- Does the abdomen look normal for the stage of pregnancy?
- Is the abdomen too large? (Too large an abdomen suggests possibility of twins or of too much amniotic fluid [polyhydramnios])
- Is the abdomen too small? ( Too small an abdomen suggests the possibility of poor growth of the baby or of too little amniotic fluid [oligohydramnios])
- Is the shape of the abdomen abnormal? (An abnormal shape of the abdomen suggests the possibility of a transverse lie.)
- Can you see the baby's movements?
Now feel the abdomen (palpation):
Feel the top of the uterus with the left hand to enable you determine the size of the uterus (fundal height) by measuring from the symphysis pubis to the top of the uterus.
Does the size agree with the gestation period worked out from the Last Menstrual Period (LMP)?
The uterus may be larger than expected because:
- There is too much amniotic fluid (polyhydramnios)
- There is more than one baby (twins or triplets)
- There is one very big baby
All these conditions could cause problems in labour, so the woman should be referred to the health centre or hospital. If the uterus grows too little it could be because the baby is growing poorly.
• Feel the lie of the foetus:
- Is it longitudinal? (The lie is longitudinal if the baby is lying with either the head or the breech (the bottom) directly above the pelvis.)
- Is it transverse? (The lie is transverse if the baby is lying across the abdomen with the back or an arm towards the pelvis.)
- Is it oblique? (The lie is oblique if the baby is lying diagonally, with the head or the breech in the iliac fossa.)
• Feel the presentation of the foetus.
Presentation is the part of the baby which is at the lower end of the uterus and will be born first. Check if:
- Is it cephalic (the head) or is it breech (the bottom) presentation? The foetus normally lies longitudinally with a cephalic presentation. The head is easy to feel as it is hard and round.
- Engagement is the going down of the head into the pelvis. In primigravida, this happens during the last four weeks of pregnancy. However, in multipara and in most primigravidae, the head remains high and above the pelvis until labour pains start. When the head is engaged, only a small part of it can be felt on abdominal palpation.
• Listen to the fetal heart (auscultation): It is usually possible to hear the fetal heartbeat with a fetal stethoscope from 28 weeks (7 months) onwards. It is easiest to hear the heart by placing the fetal stethoscope over the baby's anterior shoulder, or in the middle of the uterus over the woman's umbilicus.
To count the fetal heart, you need a clock or watch with a second hand ticker. Count the number of beats during a full minute. If there is no clock or watch, feel the mother's pulse at the same time as you listen. The fetal heart should be much faster than the mother's pulse and is normally between 120 and 160 beats per minute.
If the mother complains that she cannot feel her baby moving, you cannot hear the fetal heart, and the pregnancy is more than 28 weeks, then refer the woman to the health centre as the foetus may have died (intrauterine death).
Laboratory tests: Screening reveals incipient evidence of conditions that put the pregnant mother or her baby at high risk before signs of the actual disease are manifest. Confirmatory laboratory tests are then made to establish the findings.
- Test urine for protein and sugar at every antenatal visit. The presence of protein in urine may indicate pre-eclampsia, while the presence of sugar in urine may indicate diabetes. Both of these conditions put the mother and the baby at high risk.
- Also, test the mother's blood for haemoglobin estimation and for malaria parasites if the mother is anaemic. If she is found to have malaria, she should be treated. (See Unit 9 for more details). In larger health facilities like hospitals, where a test for syphilis can be carried out, it should be done to rule out syphilis. If a mother is found to have syphilis, she should be treated. This will prevent the baby from getting syphilis from the mother. Elisa test for Human Immunodeficicency Virus (HIV) infection should also be done. If the test is positive, appropriate treatment measure is instituted. (See Unit 14)
Immunizations: Immunization of pregnant women with at least two doses of tetanus toxoid prevents neonatal tetanus. (See Unit 9) Tetanus toxoid stimulates production of antibodies. These antibodies cross the placenta to enter the blood of the baby and protect the baby against neonatal tetanus.
Identify High Risk Mothers Mothers who deviate from normal are termed "high-risk." These include:
- Mothers with a history of stillbirth, premature deliveries, neonatal deaths and previous difficult labour;
- Mothers with previous caesarean section;
- Short mothers. Height less than 150 Cm;
- Young (below 15 years) or elderly (above 35 years)
- mothers pregnant for first time;
- Mothers with medical conditions like hypertension, diabetes and tuberculosis;
- Mothers with vaginal bleeding;
- Mothers with twin pregnancies;
Always identify early all high-risk mothers and refer them to hospital so that an appropriate plan of management can be formulated well in advance. High-risk mothers need to be seen more frequently than mothers with normal pregnancies. Advise mothers with normal pregnancies to continue attending the Antenatal Clinic at the health centre or dispensary. When you are at a health centre or dispensary you can refer them when the need arises.
You should encourage Traditional Birth Attendants (TBAs) to send their clients to Antenatal Clinics for antenatal care. Help them to understand and recognise that there are certain problems that they cannot deal with alone.
Confirm your answers as you read the following discussion.
PERINATAL CARE:
Perinatal care is the health service given to a mother and her baby during labour. Labour is defined as the period from the time painful uterine contractions start until the baby, the placenta and the membranes are completely expelled from the uterus and bleeding is controlled.
The average duration of labour is 18 hours. If a mother has not delivered by this time, she should be carefully assessed. If she appears unlikely to deliver in the next 2 - 3 hours, then refer her to hospital.
The health worker has three duties when looking after a mother in labour:
- To make sure the mother is well.
- To make sure the baby is well.
- To make sure the labour is progressing normally.
When a midwife is called to see a mother in labour she should do following:
- Take a history of labour: When taking the history, she should ask how long the mother has been having painful uterine contractions and whether the membranes have ruptured. If the membranes have ruptured, she should find out the colour of the amniotic fluids.
- Check the mother's Antenatal record: A midwife should check the mother's Antenatal card and make sure there have been no abnormalities and the mother is low risk.
- Examine the mother: A midwife should carry out a general examination of the mother to find out whether there is anaemia or high blood pressure. She also carries out an abdominal examination of the mother to determine the lie of the baby and the presenting part. If the lie of the baby is transverse or if the baby is presenting with buttocks instead of the head, the mother should be referred to hospital for better management.
- If the midwife is satisfied that everything is normal and the mother is low risk, she should then prepare the room and a tray for delivery. If there are abnormal findings the midwife should refer the mother to hospital.
- During labour, after the baby's head is born, wipe the nose and mouth clean to clear the airway. If the airway is blocked, the baby will die.
- When delivering the baby, a midwife should handle the baby gently to prevent injury to the baby and tearing of the mothers perineum.
- A midwife must make sure that bleeding from the placental site is as little as possible, and she must prevent postpartum haemorrhage. If the mother bleeds a lot before the placenta has come out, the midwife should give an injection of Ergometrine intramuscularly immediately and use controlled cord traction to deliver the placenta.
- The midwife should look carefully at the placenta to make sure it is complete. If it is not complete, the mother may continue to bleed from the vagina and should be referred to hospital.
Do the following activity before continuing with the next section:
Compare your answer with the following discussion.
Assessment of the new born baby is part of perinatal care and is done using the Apgar Score. This is done routinely at 1 and 5 minutes after delivery. You can use Table 2.4 to help you to assess a newborn baby.
Assess the condition of the baby by looking at:
- Colour of the skin (the normal colour is pink).
- Heart beat. Listen to it with a stethoscope.
- Respiration. Watch the chest and abdomen.
- Grimace (response to stimuli). Does the baby cry when pinched?
- Activity (muscle tone). Does the baby move?
Table 5.4: Assessing Newborns by Apgar Score
| SIGN | SCORE | ||
|---|---|---|---|
| 0 | 1 | 2 | |
| Colour | Blue or pale grey | Pink body, blue extremities | Pink all over |
| Heartbeat | Absent | Less than 100 beats/minute | More than 100 beats/minute |
| Respiration | Absent | Slow, irregular, gasping | Normal |
| Grimace (response to stimuli) | None | Grimace (slight) | Cry |
| Activity (muscle tone) | Limp | Some flexion of extremities | Active motion |
Classification according to total score:
- Apgar score 7 - 10 = Normal
- Apgar score 4 - 6 = Moderate asphyxia
- Apgar score 0 - 3 = Severe asphyxia
Asphyxia is lack of oxygen in a baby and manifests with slow heartbeat. Asphyxia is the commonest cause of deaths and long-term disabilities in babies.
You or the midwife should also give the baby the following vaccines:
- BCG 0.5 ml;
- Oral Polio Vaccine Zero 2 drops.
These protect the baby from tuberculosis and poliomyelitis and should be recorded in the child health card of the baby.
Let us now discuss low birth weight, which is one of the most common problems in this country.
LOW BIRTH WEIGHT
After assessing the condition of the baby by Apgar score, you should weigh the baby and record the weight in the baby’s record and in the child health card. Birth weight is the first weight of the newborn obtained at birth, preferably within the first hour of life.
At the beginning of this unit, we said that the average birth weight is 3.5 Kg, but some babies are born with a weight more or less than 3.5Kg. Our main concern is babies with low birth weight.
Low birth weight is a birth weight less than 2500g (2½kg) regardless of the estimated period of gestation. This condition reflects intra-uterine malnutrition and growth retardation of the foetus.
Do the activity below before continuing with your reading.
I hope your answers included the following:
Low birth weight can be due to:
- Prematurity;
- Small size of the mother. If a mother is short (height < 150cm ) and weighs less than expected, she is likely to have a baby with low birth weight;
- Poor nutritional status of the mother leading to Protein-Energy Malnutrition
- Anaemia;
- Unregulated fertility (too many and too closely spaced births);
- Twins;
- Congenital malformations;
- Chromosomal abnormalities;
- Maternal Infections (malaria, tuberculosis, urinary tract infection);
- Congenital infections (cytomegalic inclusion virus, rubella, syphilis);
- Other illness in pregnancy, such as pre-eclampsia, hypertension and antepartum haemorrhage;
- Placental abnormalities;
- Maternal cigarette smoking and alcoholism;
- Pregnant mothers doing manual labour in the fields until very late in pregnancy.
Now that we know the causes of low birth weight, let us also discuss the risks associated with low birth weight:
A baby with low birth weight is likely to be at risk of the following:
- Weak suckling, swallowing and cough reflexes which lead to difficulties in feeding and danger of aspiration of milk into lungs;
- High susceptibility to infections;
- Limited iron stores which can lead to the development of iron deficiency anaemia later in infancy.
Risk of hypoglycaemia.
Finally, let us discuss the management of a baby with low birth weight.
The following routine methods applied to a baby with normal birth weight should be followed:
- The umbilical cord should be tied with a double ligature.
- All low birth weight babies should be given 1 mg Vitamin K1, by intramuscular injection, in order to prevent haemorrhage.
- Low birth weight infants should be allowed to rest in their cots as much as possible.
- Feeding should be started as soon as the infant has recovered from birth. Breastfeeding is essential for the survival of the infant and should start within an hour of delivery. If suckling at the mother's breast is not possible, the mother should be shown how to express breast milk before feeding the infant. Ensure that the colostrum from the mother is given to the infant and is not wasted.
Complete the next activity before continuing with the reading:
| 10
Besides postpartum haemorrhage and retained placenta, what other problems may arise during labour to either the mother or the baby? List 4 problems below. ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ……………………………………………………………………………………………………………… ………………………………………………………………………………………………………………
|
I hope your list included the following common ones, starting with fetal distress.
Fetal distress: Fetal distress is a condition in which the fetus is not getting enough oxygen. Foetal distress will kill the baby unless the baby is delivered quickly. Fetal distress is caused by:
- Prolonged labour
- separation of part of the placenta
- prolapsed cord
- illness in the mother, such as high blood pressure.
- malpresentation
How can you recognize fetal distress? Foetal distress is firstly recognized by listening to the fetal heart beat rate. If it is less than 120 beats per minute, faster than 160 beats per minute, or very irregular instead of the normal 120 – 160 heart beats per minute then you should diagnose fetal distress.. Secondly, foetal distress is recognize if you find brown or green staining of the amniotic fluid due to the passage of meconium.
In these cases, a midwife should deliver the baby as soon as possible. If the hospital is less than a two-hour journey away, she should transfer the mother to hospital if she thinks there is time to do so before the mother delivers. If the hospital is more than two hours away, the midwife should continue looking after and delivering the mother.
Cephalo-pelvic disproportion: Cephalo-pelvic disproportion is a condition in which the baby's head is too big to go through the mother's pelvis. Both mother and baby may die if they do not get help. One of the most important duties at an antenatal clinic is to find out which mothers are likely to develop cephalo-pelvic disproportion and make sure that they deliver their babies in the hospital.
Obstructed labour: Obstructed labour is the condition that results from cephalo-pelvic disproportion, abnormal lie and malpresentations if they are not treated. Obstructed labour can be avoided if all women are looked after by trained health workers during pregnancy and labour. The causes of obstructed labour will then be detected during pregnancy or in early labour and the mother can be referred to hospital in time for proper treatment.
If obstructed labour is not treated, the mother will get infection. The baby usually dies, and sometimes the mother will die too. If the mother has had many children, her uterus may rupture.
Transverse lie: It is normal for a baby to lie transversely before 32 weeks of pregnancy. After the 36th week, a transverse lie must always be referred to hospital because the baby cannot be born normally.
Having discussed perinatal care, let us now discuss the importance of postnatal care and the effects of not having postnatal care.
POSTNATAL CARE
Before you read on do the following activity. It should take you less than 5 minutes.
Postnatal care is the service given to the mother and the baby in the first six weeks after delivery. These six weeks constitute the postnatal period. During the postnatal period, the organs related with child bearing return to their pre-pregnancy state.
Why do we provide Postnatal care?
We provide postnatal care for the following reasons:
- To find out whether the mother’s reproductive organs have returned to their pre-pregnancy state;
- To check the mother's condition;
- To check the baby's condition.
Compare your answer with what follows.
The services you should offer during postnatal care are as follows:
- Examination of the mother to make sure that:
- She has enough blood
- The uterus and birth canal have returned to the pre-pregnancy state.
- Breasts have no problems and are producing milk adequately for the baby.
- The tears and cuts in the birth canal have healed.
- No delayed genito-urinary complication has occurred, such as leaking of urine or faeces through the vagina;
- Starting the mother on Family Planning methods if she chooses to do so.
- Information and advice to the mother on the following:
- Simple exercises to help abdominal muscles become firm again.
- Breast-feeding.
- Proper nutrition for a breast-feeding mother.
- Care for herself, baby and the family.
- Giving care to the baby as follows:
- Gently drying the baby with a warm towel and cover him well and placing him in a warm environment.
- Weighing the baby.
- Measurement of the head circumference and the length
- General examination.
The baby is immunized against polio, diphtheria, whooping cough, tetanus, Hepatitis B, Haemophilus b influenza, and tuberculosis (if BCG was not given at birth). The baby is exclusively breastfed within the first hour of delivery.
Now let us discuss the common problems that can arise for a newly delivered mother.
Sometimes the newly delivered mother develops some problems, especially in the breasts during lactation. These problems are more common in young mothers having their first babies. You should be able to identify these problems during the postnatal care and manage or refer them to the health centre or hospital for better management.
Now do the following activity. It should take you less than 5 minutes to complete.
Now check if your list compares with the one below.
The most common problems that arise include:
- Breast engorgement
- Sore and Cracked nipples
- Breast abscess
- Mastitis
- Post partum mental illness
Let us discuss each of these problems in detail starting with breast engorgement.
Breast engorgement: Between the third and fifth day after delivery, the breasts fill with milk that replaces the colostrum. It is common for the mother to have a slight fever at this time, but it will last only one or two days. If the fever lasts for more than two days, look for infection and treat it. Sometimes the breasts swell enormously. This is called breast engorgement.
When the breasts are engorged:
- They feel painful and are tender to touch.
- The skin over the breasts is smooth and shiny.
- Veins appear under the skin.
- Lumps may be felt in the breasts.
Breast engorgement is less likely to occur if:
- The baby sucks the colostrum for the first two days;
- The baby is kept with the mother and allowed to suck on demand night and day;
- The baby sucks in the correct position;
- The baby empties the breast at each feed;
- The breast is emptied by manual expression of the milk.
Sometimes the breast is not fully emptied because the newborn baby may not be strong enough to suck in the first few days or the mother may produce more milk than the baby needs. Then engorgement may develop.
You should treat a mother with breast engorgement as follows:
- Encourage the mother to continue breastfeeding if the breasts are not painful;
- In case the baby is unable to suck, like in premature babies and babies following difficult delivery, or in case the breasts are too painful, the mother should express the milk by hand. This is what we refer to as manual expression of breast milk;
After some milk has been expressed, the breasts become soft and less painful. Then the baby is able to suck.
If the baby cannot suck, encourage the mother to give him the expressed milk by cup and spoon. She should avoid using the bottle.
Advise the mother to continue expressing milk by hand as often as necessary to keep the breasts empty and soft until the baby can suck.
How to express milk by hand: Expressing milk by hand is not difficult and requires only perseverance and practice. See Figure 5.11 below.
Figure 5.11: Expressing milk to treat engorgement
To express milk effectively a mother should:
- Press repeatedly and rhythmically behind and around the nipple area.
- Press with finger and thumb above and below and then from the sides.
- Collect the milk in a clean bowl or mug.
Advise the mother to express from the breast for 3-5 minutes and then repeat with the other breast. When manual expression is only needed for one breast (because of a cracked nipple or mastitis), then the baby should continue to suck normally from the other breast.
Sore and Cracked Nipples: Sore and cracked nipples is a condition in which the nipples have cracks and sores form thus making the breast painful.
Sore nipples result from the baby sucking the nipple instead of sucking the areola, the darker part of the breast. If a mother continues breastfeeding through a sore nipple, it causes a crack in the nipple. Nipple sucking is painful, but sucking the areola is painless.
The crack makes breastfeeding painful and the mother may stop giving that breast to the baby. When this happens, the breast fills with milk and may become infected. It is very important to prevent sore and cracked nipples because this will help prevent mastitis and breast abscess. Sore and cracked nipples can be prevented by proper positioning of the baby’s mouth on the areola of the breast. The mother needs to be taught the proper attachment of the baby to the breast. . You should advise a mother to continue breastfeeding on the breast that does not have a problem.
Improving the baby's sucking position on the breast with the cracked nipple is sometimes enough to stop the pain and allow the baby to continue sucking. If there is still too much pain, advise the mother to express the milk by hand and feed it to the baby by cup and spoon. When the crack heals after a few days the baby can suck again from both breasts.
Mastitis: Mastitis means an infection of the breast. Mastitis may happen when the breast is not emptied completely. Then germs may enter through a cracked nipple and infect part of the breast.
Symptoms and Signs: A patient with mastitis presents with the following signs and symptoms:
- The infected area is very red and tender to touch.
- It is usually shaped like a triangle.
- Lumps may be felt in the arm pit. These are enlarged lymph nodes.
- The mother feels very unwell and usually has both fever and headache.
Advise the mother to rest as much as possible. She should continue breastfeeding from the normal breast. She should manually express milk from the infected breast and give the expressed milk to the baby. Alternatively, give the mother two tablets of Acetylsalicylic Acid and wait for half an hour. Then, if it is not too painful, allow the baby to suck from the infected breast. Reassure her that this will not make the baby ill. It is very important for the mother to empty the breasts or the infection will not be cured.
Treatment: Give her a full course of Penicillin, 2 mega-units to start, followed by 1 mega-unit daily for 5 days. Place warm cloths or towels, soaked in warm water, on the breast to relieve the pain and support the breast.
Remember to refer the mother to the health centre if there is no improvement after two days.
Mastitis must be treated early and thoroughly to prevent the development of a breast abscess.
Breast Abscess: A breast abscess develops when there is a collection of pus in the breast. It is a complication of mastitis when it is not treated early and thoroughly.
Symptoms and Signs: The signs of a breast abscess are distinguished from mastitis by the following:
- The mother becomes very ill with a high temperature;.
- The infected mastitis area becomes larger;
- The skin over the area becomes thick;.
- Instead of being hard, the area can now be depressed. There is a bag of pus under the skin;
- Fluctuation.
A breast abscess is treated in the same way as mastitis with urgent referral to a health centre or hospital for further treatment.
The abscess needs to be opened and the pus drained away. After opening, the wound needs to be dressed daily. The mother should continue breast feeding on the normal breast. One breast will make enough milk if it is emptied regularly.
Prevention of mastitis and breast abscess is by correct attachment of the baby to the breast and proper hygiene. Proper breast hygiene is daily washing of the nipples with clean water. It is not advisable to put ointment or medicine on the nipples. Cleaning them is enough.
5.3: SUMMARY
In this unit we have described the normal growth and development of children. We said that growth is the progressive increase in size and development is progressive acquisition of skills or abilities. Each child follows a particular path in growth and development that is determined by his genetic make up. A child genetically determined to be tall grows slightly more rapidly than a child genetically determined to be short. Similarly, a child genetically destined to be clever develops more rapidly than one destined to be less intelligent.
We also said that adequate nutrition is one of the environmental factors that influence growth and development. There are several ways of measuring growth, but the best way and the one most commonly used in our health facilities is weighing.
Lastly, we discussed antenatal care, perinatal care and postnatal care and their importance. Remember the health of a child starts from the mother’s womb. So we should take good care of pregnant mothers. Do not forget to pay special attention to newborns with low birth weight as it is a major cause of mortality and morbidity of the newborns.
Congratulations! You have now come to the end of this Unit. Have a rest before you do the attached assignment.
|
DIRECTORATE OF LEARNING SYSTEMS DISTANCE EDUCATION PROGRAMME
Name: __________________________________________ Address_________________________________________ ________________________________________________
CHILD HEALTH COURSE UNIT 5: ASSIGNMENT GROWTH AND DEVELOPMENT
1. List 3 measures you can use at your health facility to determine whether a child is growing. ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 2. At what age should a baby begin walking? ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 3. Outline 4 factors that promote development of a child. ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 5. Explain why it is important to take a pregnant mother’s past obstetric history and medical history during antenatal care. Past obstetric history: ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 7. Explain why immunizing pregnant mothers against tetanus is important: ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 8. What is perinatal care? ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 9. Outline five (5) things a midwife should do for a mother and baby during perinatal care: ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 11. List three causes of obstructed labour: ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 14. What is low birth weight? ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
17. Outline three risks to a low birth weight baby: ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 18. What is postnatal care? ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 19. Outline three reasons why it is important for a mother to attend postnatal clinic: ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ 20. A breastfeeding mother comes to your health facility complaining of painful breasts. On examination you find that the breasts are full with milk and the mother has a temperature of 39°C. Explain how you would manage this mother: ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
Once you complete this assignment, post or bring it in person to AMREF Training Centre. We will mark it and return it to you with comments. |
Our address is as follows:
Directorate of Learning Systems
AMREF Headquarters
P O Box 27691-00506
Nairobi, Kenya
Email: amreftraining@amrefhq.org