Lesson 4: Treatment of Malaria
Contents
- 1 Introduction
- 2 Lesson
- 2.1 The Principal Objectives of Malaria Treatment
- 2.2 The principle objectives of Malaria treatment are:
- 2.3 The Role of Health Workers in the Treatment of Malaria
- 2.4 Drug Used In the Treatment of Malaria
- 2.5 Treatment of Simple Malaria
- 2.6 First Line Treatment
- 2.7 Second Line Treatment
- 2.8 Treatment schedule
- 3 Management of Severe Complicated Malaria.
- 4 Self Assessment
- 5 Assignment
Introduction
Welcome to Unit 4 on treatment of Malaria. In the last unit you learnt about severe and complicated Malaria and how to diagnose it.
In this unit we shall look at the treatment of both simple and severe Malaria. Let us start by looking at our objectives for this lesson.
By the end of this unit you should be able to:
wn the principle objectives of malaria treatment;
- State the role of health workers in the treatment of Malaria;
- Describe the treatment of simple Malaria;
- Describe the management of severe and complicated Malaria;
- Treat and/or refer severe and complicated Malaria}}
Lesson
The Principal Objectives of Malaria Treatment
It is important to bear in mind that although malaria is among the top 5 causes of morbidity and mortality in Africa, it can be managed with proper diagnosis and prompt treatment. One of the reasons behind the renewed interest in this disease is the emergence of drug resistant strains of the parasites towards the easily available like Chloroquine and Fansidar. That is why it is very important to have guiding principles on malaria treatment
Before you read on do activity 1. It should take you 5 minutes to complete.
|
Write down three objectives of malaria treatment ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
Compare your answers with the information given in the following discussion.
The principle objectives of Malaria treatment are:
- To shorten the duration of the illness and cure it;
- To prevent the illness from becoming severe;
- To avoid death;
- To prevent further transmission;
- To serve as secondary prevention.
Having learnt about the principle objectives of malaria treatment, let us now turn to your role as health worker in treatment of Malaria.
The Role of Health Workers in the Treatment of Malaria
As a health worker you play a very important role in ensuring that the principle objectives of malaria treatment are achieved. How do you do this? Remind yourself by doing Activity 2. It should take you 3 minutes to complete.
| 1
What is your role in the treatment of malaria? ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
Correct your response as you read the following discussion.
The following are some of your key roles you play in the treatment of Malaria.
- Making proper diagnosis;
- Starting prompt and correct treatment with antimalarials;
- Supervising treatment, and ensuring the first dose of antimalarials is administered using “Direct observed therapy (DOT)”.
- Giving patients and their families information about diagnosis, importance of taking treatment as prescribed, need for their participation in the recovery process and prevention of further attack of Malaria;
- Keeping confidentiality;
- Being alert to the possibility that patients may have sought and received antimalarial treatment from other sources.
Having learnt what your role is in the treatment of Malaria, let us now turn to drug treatment of Malaria. We shall start by looking at the drugs used in the treatment of malaria.
Drug Used In the Treatment of Malaria
There are many antimalarial drugs available in Africa. You may have noticed this from the many advertisements of antimalarial drugs available from your health centre pharmacy or local drug shop.
| 2
List down at least 10 antimalarial drugs that you know ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
There are various antimalarial drugs available in Africa. Some act specifically on a stage of the malaria cycle while others are non-specific.
Some of these drugs include
- Amodiaquine (CAMOQUINE)
- Chloroquine
- Sulfadoxine/pyrimethamine (FANSIDAR)
- Quinine
- Primaquine
- Mefloquine
- Metakalfin
- Halofantrine (HALFAN)
- Artemether (ARTENAM)
- Arsumax
There are other drugs which have antimalarial activity but are not primarily used as antimalarials. These include: Azithromycin, Clindamycin, Doxycycline, Proguanil, Tetracycline and Septrine (Cotrimoxazole).
When deciding on the drug of choice for malaria treatment, it is important to take note of the following points:
- It is no longer advisable to use drugs that have shown high failure rates (e.g. Chloroquine, Amodiaquine, Sulphadoxine/Pyrimethamine and Sulfalene/Pyrimethamine) for the treatment of Malaria.
- The use of monotherapies such as Artesunate, Dihydroartemisinin, Artemether, Lumefantrine, Mefloquine, Chlorproguanil/Dapsone and Atovaquone/Proguanil are not recommended to avoid the rapid emergence of resistance to individual drugs;
- Where artemisinines are used as monotherapies, a 7 day course of treatment is recommended and adherence to treatment should be ensured.
The use of combination therapy/treatment is the recommended approach and especially atemisinin combined therapy (ACTs)
You have now learnt about the drugs used in the treatment of malaria. Next we shall discuss in turn, how to treat simple and severe/complicated Malaria. We shall start with treatment of simple malaria.
Treatment of Simple Malaria
As we mentioned in the last unit, Malaria may be described as simple or uncomplicated when the infection is not life threatening and is easily treatable.
There are four drugs that have previously been used for treatment of simple Malaria. These are *Chloroquine
- Sulphur Perimethamide (Fansidar]
- Amodiaquine
- Quinine.
However, due to the development of parasite resistance to some of these drugs, several changes have been introduced in the treatment of malaria. As a result, malaria is no longer treated with a single drug. A combination of drugs for treatment malaria is recommended. Although the choice of drug combination may vary from country to country, It is now recommended that malaria should be treated with a combination of two drugs one of which should be an artemisinin derivative. Combination drugs can either be co-formulated or co-packaged. Co- formulated drugs are two or more different drugs combined and taken as one tablet whereas co-packaged are two or more different drugs packaged together to be taken at once. The drugs can be given either as first line treatment or second line treatment. What does that mean? Let us see below.
First Line Treatment
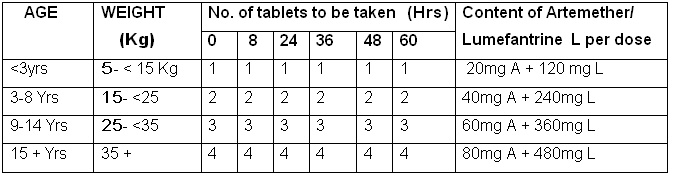
First line drug combination for treatment of Malaria refers to the drugs used initially for treatment of simple Malaria. The recommended first line treatment for Kenya is a fixed dose combination of ARTEMETHER/LUMEFANTRINE (20/120mg).
NB: For countries in which the antimalarial drug policy has not been changed refer to Annex A (or use the country specific recommendations).
Second Line Treatment
Second line drugs are used for the treatment of Malaria after the parasites have failed to respond to the 1st line treatment. They are also in case a patient develops an allergic reaction to 1st line drugs. In Kenya the drug used for second line treatment is oral Quinine.
You should always treat a patient with oral preparations unless there is a contraindication, such as, vomiting, severe nausea, or difficulty in swallowing. In case you begin with parenteral route, change to oral drugs as soon as the patient is stable enough to take the medicine orally.
If a child below two (2) months of age is brought to your facility with fever, this is usually a very serious condition and the cause may not necessarily be Malaria. In highly endemic areas, you should exclude other causes of fever such as meningitis, septicemia, urinary tract infections, respiratory tract infections, local sepsis/abscess, or ear infections.
Treatment schedule
The following are the treatment guidelines for both first line and second line treatment of simple malaria in Kenya.
1st line Treatment of simple malaria
Table 1: DOSAGE FOR ARTEMETHER/LUMEFANTRINE (20/120mg) (COARTEMR )
NB: In children weighing less than 5 Kg quinine is recommended.
Second line treatment of Malaria
The Second line treatment should be oral quinine. A full course of quinine tablets should be given when the 1st – line treatment (Coartem) has failed due to any of the reasons we mentioned earlier.
Table 2: DOSE: QUININE 10 mg/kg body weights given every 8 hours for 7 days.
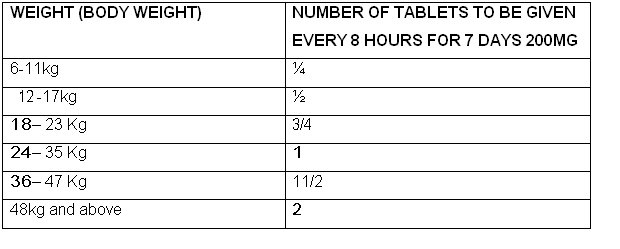
Refer to the Schedule in Annex B
Now you are ready to treat a patient with simple Malaria. Let’s practice from the following case studies.
|
Tonny is a 7 year old boy in Class 2. He was returned home by his school teacher because he was sick. Tonny’s mother has brought him to your health facility. She reports a history of fever and vomiting which lasted for one day. The rest of the history is unremarkable. You examine him and find he is 22 Kg and has a temperature of 38.5o C. The rest of the examination findings are normal except a tipped spleen. You do a blood slide and the report shows P. falciparum (+). |
Based on the above case study, do Activity 4 below. It should take you 3 minutes to complete.
| 4
a) What is your Diagnosis? ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… b)How would you further manage Tonny’s condition? ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
Confirm your answer as you read the following discussion.
From the case study, we can see that Tonny’s condition is Uncomplicated P. falciparum Malaria because it is not life threatening, that is, it has no danger signs. His management therefore includes:
- Drug treatment using Artemether/Lumefantrine (CoartemR) using 2 tablets each at 0,8,24,36,48 and 60 hours.
- Tablets panadol 1 ½, stat.
- Advising the mother on the benefits of using insecticide treated mosquito nets;
- Advising the mother on how to prevent mosquito bites through appropriate clothing, repellents and elimination of mosquito breeding places;
- Advising her to monitor the Tonny at home, he should be reviewed in 2 days time and thereafter start school if his condition is good;
- Giving Tonny an anti-emetic if vomiting is severe, or use injectable forms if available;
- Treating coexisting conditions such as dehydration by advising the mother on adequate fluid intake.
| 2B
It is now 2 days since you treated Tonny. The mother rushes him back in poor general condition. She reports that he is vomiting everything and is not able to walk, sit or talk. He also passed “Coca cola” coloured urine twice that morning. She has observed that he is pale in his palms. However he has not convulsed nor developed a yellow colour in his eyes. |
Based on the above information do Activity 5, it should take you 3 minutes to complete.
| 5
i) What is your diagnosis now? ……………………………………………………… ii) How would you manage Tonny’s present condition? ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
|
We hope you were able to diagnose that Tonny’s condition is now severe complicated Malaria. This is because he has presented with the following signs and symptoms of severe Malaria:
- Prostration/lethargy (danger sign).
- Severe anaemia,
- Haemoglobinuria,
- Vomiting every thing (danger sign).
This case study now leads us to the second part of this section where we discuss the treatment of severe Malaria.
Management of Severe Complicated Malaria.
The ideal conditions for the management of severe complicated Malaria dictate the need for an Intensive Care Unit (ICU). Unfortunately, this is not always possible in many developing countries such as Kenya. Figure 4.1 shows a section of an Intensive Care Unit.
Figure 4.1: Part of the Intensive Care Unit in a Hospital
Since ICUs are not widely available, it is therefore very important to equip yourself with the necessary knowledge and skills so that they can give the desired management with basic equipment wherever you are stationed.
Treatment of severe and complicated Malaria calls for close supervision between the clinician and the nursing staff. You should ensure proper recording of observations and careful nursing of unconscious patients. You should also give medication strictly on schedule and at required doses.
The management of severe Malaria depends on the level of your health facility. Let us look at management at the following two levels:
- peripheral level, that is health centre, dispensary, or community post;
- Hospital level.
Management at Peripheral level:
At this level you should do the following:
- Recognize severe Malaria;
- ive pre-referral treatment: Quinine 10mg salt/Kg body weight, I.M. In adults loading dose quinine 20mg/kg then maintenance at 10mg/kg 12 hourly (8hrly in adults) till can take orally then change to Coartem or oral quinine to complete 7 days of treatment. Repeat 12 hourly while awaiting transport;
- In the absence of quinine, start with any available antimalarial I.M.;
- Control temperature by tepid sponging, Paracetamol or fanning;
- Control any convulsions with rectal diazepam 5 mg in children, 1/M or I/V diazepam 10mg in adults;
- Pass Nasogastric tube for feeding, if patient is not able to take orally;
- Give oral glucose to correct hypoglycaemia;
- Give oral fluids to correct fluid imbalance;
- Look for danger signs and start management, for example, take blood for grouping and cross-matching, institute anti-meningitis treatment, do L. P. if possible etc
If referral is not possible, keep the patient at the unit and continue with:
- Quinine 10 mg salt/Kg body weight IM 8 hourly until the condition is better, that is, the patient is conscious, or can eat orally, can sit up, can talk, or symptoms have subsided. Then change to oral quinine to complete 7 days of treatment. (Refer to Quinine Treatment Schedule for dosage on page 9)
- If there is no quinine then continue with I/M chloroquin 3.5mg base/Kg body weight 6 hourly until a full dose of 25mg/Kg body weight is completed (i.e., 8 injections)( in countries where chloroquin is still sensitive).
Table 3: Dilution of Quinine for intramuscular injections.
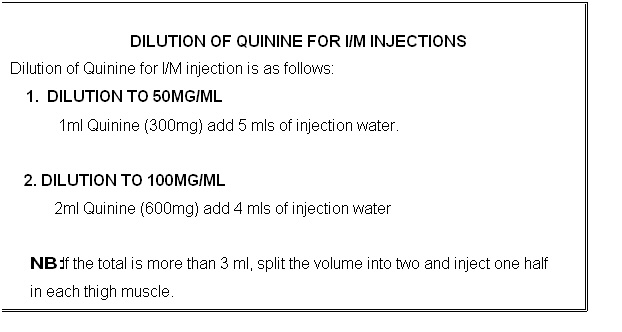
NB: If the total is more than 3 ml, split the volume into two and inject one half in each thigh muscle.
- You MUST always refer the following conditions to hospital because they require intensive care:
- Persistent convulsions;
- Renal failure;
- Pregnant mother with severe Malaria;
- Pulmonary oedema;
- Severe anaemia See Figure 4.2;
- Coma, See Figure 4.3.
Figure 4.2 Transfusing a child with severe anaemia due to Malaria.
Figure 4.3 A malaria victim in coma.
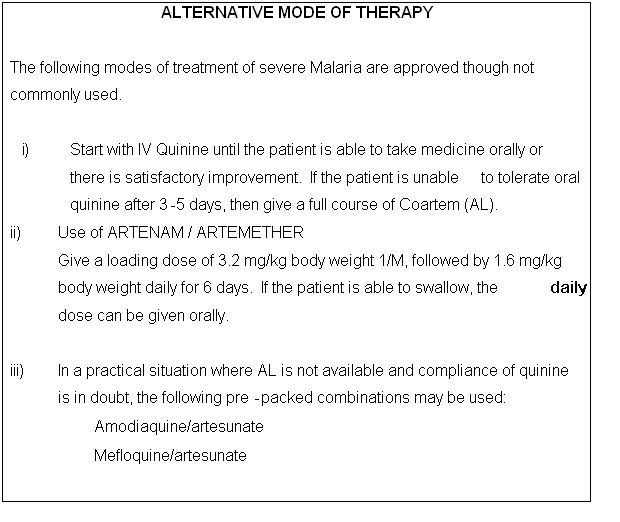
Management of severe malaria at Hospital level.
At this level, you should do the following:
- A. Institute URGENT Antimalarial Treatment:
- Use IM/IV Quinine as the drug of choice for treatment of severe Malaria;
- Administer quinine dose as 10mg salt/kg body weight, 8 hourly to complete 7 days of treatment, both adults and children;
- Give 10mg of quinine salt/kg body weight (not to exceed 600mg as single dose) in 5% dextrose infusion, given over 4 hours period. Repeat this dose after every 8 hours until the patient can take oral medication;
- In an adult, put the required quinine dose in 500 mls of 5% dextrose then run it over 4 hours;
- In children you should give quinine 10mg/kg body weight in appropriate volume of 5% dextrose as 5-10mls/kg of body weight depending on the patient’s Onset fluid balance;
- Because of the danger of cardio-toxicity, never exceed a single dose of quinine of 600 mg salt, even when body weight exceeds 60 kgs;
- Give a bolus of 50% dextrose slowly IV over 1-2 minutes to correct hypoglycaemia.
IV 50% DEXTROSE DOSE
- Give a bolus of 1 ml/kg body weight of 50% dextrose in children.
- Give a bolus of 20 mg in an adult.
Please note the following regarding the duration of treatment with quinine in severe malaria case:
- Give IV quinine until the patient is able to take orally. Ensure that the patient continues with oral quinine to complete a 7-day’s course or artemether/lumefantrine full course;
- It is unusual to continue IV infusions of quinine for more than 4-5 days. This is because patients usually improve by 3rd day of intensive treatment.
B. Institute Supportive Treatment.
Supportive treatment is important in the management of severe Malaria and you should always provide it for the following conditions:
• Hypo-glycaemia. : To correct hypoglycaemia, you should:
- give a bolus of 50% dextrose in both adults and children.
• Dehydration. Ensure continuous adequate feeding. Assess the degree of dehydration and fluid requirement based on body weight and set up appropriate volume of fluids to run in the first four hours;
• Convulsions. To control convulsions, first correct any detectable cause of convulsions, for example, hypoglycemia, and hyperpyrexia. Give anti-convulsion drug, such as:
- I.V Rectal diazepam 5 mg in children(0.3mg/kg iv or 0.5mg/kg rectal),
- 10mg diazepam IV in adults.
• Temperature: Reduce body temperature if greater than 38.5o C, you can do this best by giving Paracetamol by mouth if possible. AL has no anti-pyretic activity. Other ways you can use to reduce body temperature are tepid sponging or fanning;
• Severe anaemia: To correct severe anaemia, you should give a transfusion with packed cells;
• Renal failure: To correct this you should correct dehydration. Pass a urinary catheter, this is necessary to guide fluid balance. If the patient is still oliguric, give furosemide 1-5 mg/kg body weight slowly I.V, if there is no response, consider dialysis.
Maintain proper fluid balance for those patients on IV fluids.
C. Carry out Vital investigations
- Ensure that the following vital investigations are done:
- Blood For malaria parasites;
- Blood Sugar;
- Full Blood Count (Hb, Wbcs);
- Laboratory monitoring of malaria parasites daily;
- Lumber puncture and csf analysis to exclude meningitis;
- Blood electrolytes: Na+, K+, urea;
- Blood culture to exclude any bacterial infection (septicemia).
D. Monitor the vital signs and laboratory indicators
- You should monitor the following vital signs:
- Level of consciousness (use Glasgow Coma Scale (GCS) for adults and Blantyre coma scale for children given in Annex B);
- Parasitaemia by (blood smears);
- Temperature at least twice daily;
- General condition of patient.
- Blood pressure
Your aims of monitoring include:
- Controlling delivery of drugs and infusion fluids;
- Detecting complications of Malaria;
- Detecting toxic effects of drugs given;
- Documenting the patient’s recovery and charting findings and treatment.
CONCLUSION
You have now come to the end of this unit. In this unit we looked at the principles of management of simple and severe or complicated malaria. We saw that the management of severe malaria should consist of:
- Establishing an I/V line as soon as possible;
- orrecting hypoglycaemia;
- Administering appropriate volume of fluids;
- Administering correct drug in correct dosages for treatment of Malaria;
- Controlling body temperature;
- Maintaining body fluid balance.
Avoid the following in the treatment of Malaria:
|
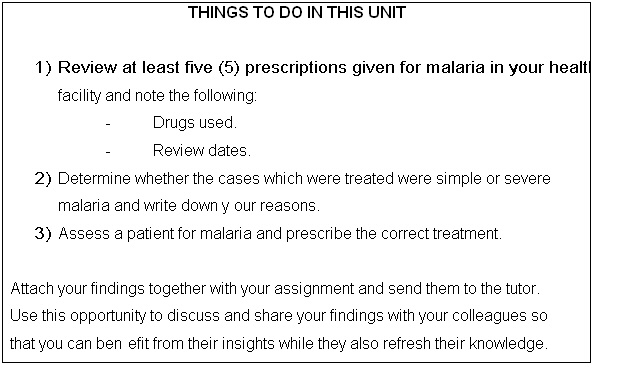
You should now review the learning objectives at the beginning of this unit to see if you have achieved all of them. If there is any you are not sure about go over the relevant section in the unit again. If you are satisfied that you have achieved all the objectives, complete the attached Tutor Marked Assignment before you proceed to the next unit. Make sure you also do the practical exercise below to reinforce your knowledge and skills in the management of malaria.
Enjoy the rest of the course! ANNEXE A
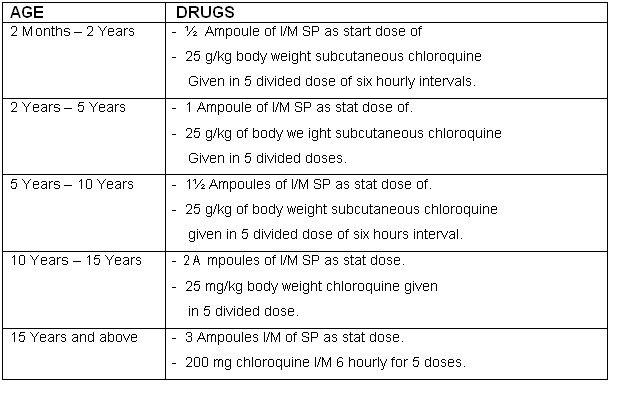
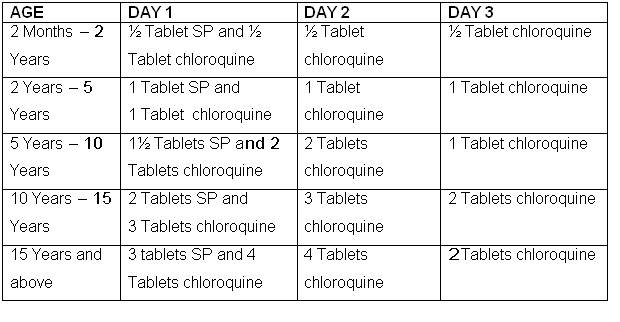
The First Line Antimalarial Treatment Schedule Using Chloroquine And Fansidar (Sp) Drugs.
Oral Drugs
• PARENTERAL DRUGS:
- ANNEXE B
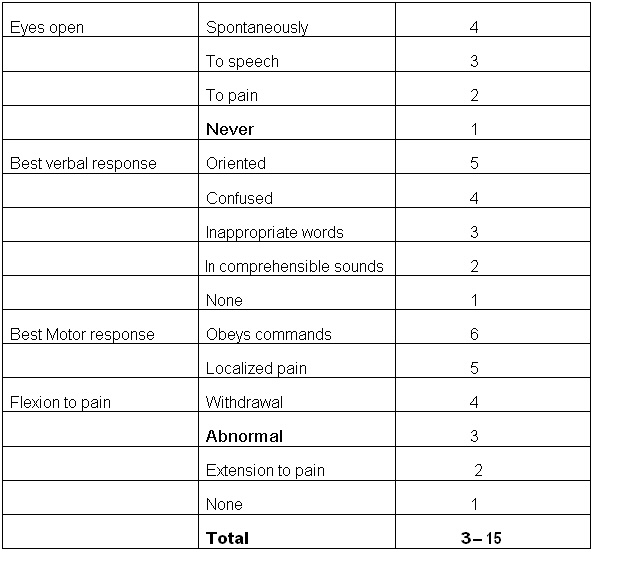
The Glasgow Coma Score (for Adults and Children over 12yrs)
- To obtain the Glasgow coma score obtain the score for each section add the three figures to obtain a total.
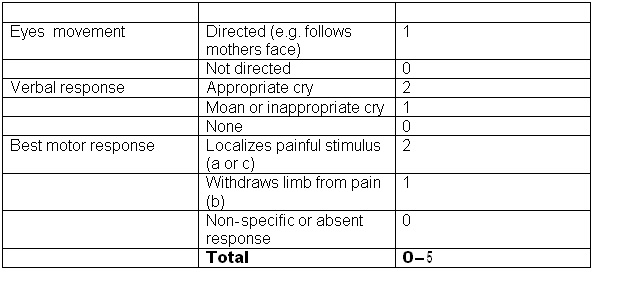
The modified Glasgow Coma scale (The Blantyre Coma Scale) for children < 12 years
- Press knuckles firmly on the patients sternum
- Press firmly on the thumbnail bed with side of a horizontal pencil
- Press firmly on the supra-orbital groove with the thumb
The scales can be used repeatedly to assess improvement or deterioration.
|
DIRECTORATE OF LEARNING SYSTEMS
Student Number:_________________________________ Student Postal Address: __________________________ __________________________
DISTANCE LEARNING COURSE ON MALARIA
1.a.What combination of drugs are used for First line treatment of simple Malaria. ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ………………………………………………………………………………………………
c.What is the drug of choice for treatment of severe complicated Malaria. ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… 2.What roles should health workers play in the management of Malaria? ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… 3a. When would you refer a patient with Malaria to hospital? ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… b.Give a reason why you would refer such a patient. ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… 4.Which medications should you not use for the management of severe complicated Malaria? ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… ……………………………………………………………………………………………… Congratulations! You have come to the end of this assignment. Please ensure that you have written your correct address and student number. Then post it to or bring it in person to AMREF. |