Lesson 4: Protein Energy Malnutrition
Contents
Introduction
A well nourished woman is likely to be healthy and therefore able to look after her family well. The outcome of pregnancy and lactation are enhanced when the woman is healthy. The nutritional needs of a pregnant and a lactating woman are greater than at other times in her life. During pregnancy, the food the mother eats helps to meet the nutritional needs of the unborn baby. During lactation, the food the mother eats helps in production of breast milk.
In this unit you will learn about Protein-Energy-Malnutrition (PEM), the most serious nutritional problem among children. The knowledge acquired will enable you to identify children with PEM in your community at the earliest possible stage and be able to manage the situation.
|
1. Define the terms: • Nutrition • Nutrition security • Malnutrition • Protein-Energy-Malnutrition 2. Name different forms of Protein-Energy-Malnutrition. 3. Discuss the causes of Protein-Energy-Malnutrition. 4. For each form of PEM: • Give its description. • Describe its signs and symptoms. • Discuss its differential diagnosis. • Describe its management. • Describe its prevention 5. List categories of children who are at risk of malnutrition. 6. Discuss malnutrition in adults. 7. Outline the effects of PEM. 8. Outline strategies for promoting proper nutrition in the community. |
PERFORMANCE OBJECTIVES
1. Promote proper nutrition in the community. 2. Identify and manage children with PEM.
|
Nutrition: Science of food, the nutrients and other substances within food, their actions and interactions and balance in relation to health and disease. • Nutrition security Appropriate quantity and combination of inputs such as food, health services and caretakers time needed to ensure an active and healthy life at all times for all people. • Malnutrition Malnutrition includes a wide range of clinical disorders resulting from an unbalanced intake of energy, protein as well other nutrients. It can present as under or over nutrition. • Protein-Energy-Malnutrition (PEM) Protein-Energy-Malnutrition is a clinical syndrome present in infants and children as a result of deficient intake and/or utilization of food. |
Lesson
Types of Protein-Energy-Malnutrition (PEM)
What are the different types of Protein-Energy-Malnutrition?
Protein-Energy-Malnutrition takes different forms which include:
• Underweight • Kwashiorkor • Marasmus • Marasmic-Kwashiorkor • Stunting • Wasting
We shall discuss each of them in detail at a later stage.
Causes of Protein-Energy Malnutrition
Stop for a while and do Activity 4/1. You should spend about 5 minutes on it.
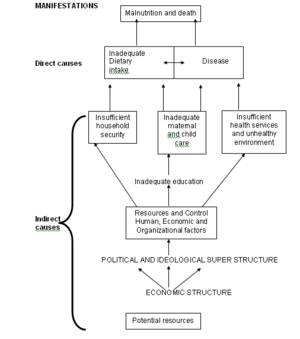
The causes of PEM can either be direct or indirect. Let us examine each of them in detail.
Direct causes
The direct factors, which are commonly referred to as immediate factors include:
(i) Inadequate food intake (ii) Diseases
(i) Inadequate food intake
Inadequate food intake is the result of limited access to food in terms of quality and quantity.
(ii) Diseases
Diseases notably malaria and measles lead to loss of appetite, increased rate of metabolism due to fevers thereby increasing the body’s nutrient demands. Diarrhoea reduces the absorption of food nutrients, whereas vomiting decreases food intake. Intestinal parasites compete for nutrients with the body e.g. hookworm competes for iron.
Indirect causes
Indirect causes of PEM include:
(i) Food insecurity and limited access to foodstuffs
• Families cannot acquire or produce enough food to cater for energy needs.
• Lack of or limited access to land or agriculture inputs, marketing and distribution of foods.
• Loss of food through destruction by pests, fungi, rodents, birds and wild animals.
• Soil erosion, often resulting from overstocking, deforestation and discriminate burning.
• Poor farming practices often due to lack of knowledge, money, time or equipment.
• Poor weather conditions like failure of rains, floods etc.
• Lack of time to gather food, prepare it properly and provide special dishes for young children. Among the time consuming and energy – expending activities of the rural African housewife are the fetching of water from long distances.
• Urbanization and rapid migration to the larger towns resulting in unemployment and low incomes.
(ii) Poor water / sanitation and inadequate health services.
• Health services may be of low quality, expensive, non-existent or unfriendly.
• Lack of pre-natal and child health care.
• Inadequate management of sick children.
• Inadequate water and sanitation facilities.
(iii) Inadequate maternal and childcare practice.
• Families do not give adequate time and resources for women and children’s health, dietary and emotional needs.
• Poor caring practices, including the inappropriate care of sick children.
• Not utilizing health care facilities for special needs of pregnant mothers or adolescent girls.
• Not supporting mothers to breastfeed adequately.
• Inadequate diets for women including food taboos during and after pregnancy.
4.4 Description and management of different forms of PEM
4.4.1 Underweight
Description
Being under weight for age is a common form of malnutrition in children, whereby the child weighs less than normal children of the same age and sex. This mildest form of PEM can be detected only by checking the weight of the child and plotting it on the Growth Chart.
Clinical signs of underweight
The remarkable sign is that the child may look thinner and smaller compared with other children of the same age and sex.
Reasons for special attention
Why do you think underweight children need special attention?
The underweight children need special attention because:
(i) Most of them are between the age of 1 to 3 years. (ii) They grow and develop more slowly than well-nourished children. (iii) They are “at risk” of illness, and theses illnesses are more serious than in well-nourished children.
Management of underweight child
How would you manage a child who is underweight?
In case you come across a child who is underweight at your health facility or in your community, this is how you should manage him or her: (i) Look for the primary cause of the child’s under nutrition. (ii) Advise the mother or caretaker proper feeding of the child. (iii) Immunize the child if he/she has not completed the immunization schedule. (iv) Follow up such children and observe the growth line. If there is no catch up, or if the weight stays the same or is lost, then refer the child for further examination and treatment. We shall discuss about growth lines later in Unit 6 when we are discussing Growth Monitoring Promotion.
4.4.2 Kwashiorkor
Description
Do Activity 4/2 below. Spend not more than 5 minutes on it.
ACTIVITY 4/2
(i) What is kwashiorkor?
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
(ii) How does a child with kwashiorkor present?
… .…………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………….
…………………………………………………………………………………
………………………………………………………………………………….
…………………………………………………………………………………
“Kwashiorkor” is a word from Ghana that means illness of the displaced child”. Displaced in this context means that a younger brother or sister has displaced the child from his or her mother’s breast.
Kwashiorkor is a severe form of protein-energy malnutrition characterized by oedema, usually starting in the feet and legs, sometimes accompanied by a skin rash and or changes in hair colour.
The condition occurs most often in children aged from one to three years.
In kwashiorkor, the diet may be sufficient to assuage hunger, but is usually grossly deficient in protein and also in energy. The diet is therefore mainly carbohydrate, and too small in quantity to cater for the child’s needs. The condition is often associated with an infectious disease especially measles.
Causes of kwashiorkor
(i) Kwashiorkor occurs most frequently in children between 1 and 3 years of age, after they have been taken off the breast. While they are getting good quantities of breast milk, they are usually getting enough protein of good nutritional quality, containing all the amino acids essential for health and growth.
The immediate cause for stopping breast-feeding is frequently the realization by the mother that she is pregnant again. She may often believe that her milk will now poison the child, who is therefore taken away from the breast. There are of course other reasons why mothers stop breast-feeding their babies early, including the need for some mothers to work or live away from home. The young child may then be put on a diet of gruel or porridge of whatever is the staple food of the family. This may be maize, cassava, banana, millet, rice, sorghum, or sometimes potatoes. The child is sometimes sent away to live with a relative, frequently a grandmother, in order to make the process of complete weaning easier.
(ii) A young African child up to this time has usually had an extremely close relationship with his mother. He has ridden on his mother’s back when she went to draw water or to till the field, he has slept in the same bed with the mother. He has had access to the breast more or less on demand. The sudden removal from this intimacy is a severe psychological shock, which may cause the child to lose his appetite, and may therefore be a factor in causing kwashiorkor. In more than one tribal language, the term for kwashiorkor is the equivalent of “displaced person”. The baby in his mother’s womb has displaced the child.
(ii) Short intervals between births. If a mother becomes pregnant and when her previous baby is only 6 months old, she may neglect the first child. Her breast milk will get less and her time and attention will be concentrated more on the new baby.
(iv) Many children in a home is another cause of kwashiorkor. In large families there often less food for each person. The smaller children may be neglected because the mother has too much work.
(v) Other diseases may sometimes play an important role in precipitating the onset of true kwashiorkor in an already poorly nourished child. Among the most important of these are gastrointestinal infections, which cause diarrhoea and may hinder proper absorption of nutrients. They may also result in vomiting, and thus loss of food. Intestinal worms and other parasitic infections may be important, as well as measles, whooping cough and other infectious diseases. Nearly all infectious diseases lead to an increased loss of nitrogen from the body. This can only be replaced by protein in the diet.
(vi) Poverty: Poor socio-economic status is another cause of Kwashiokor due to limited access to resources
(vii) Lack education on child feeding practices
(viii) Prejudices and cultural beliefs that interfere with care and feeding of young children.
Clinical signs of Kwashiorkor
How does a child with kwashiorkor present?
A child with kwashiorkor presents with the following signs.
(i) Growth failure
Growth failure always occurs in a child with kwashiorkor. If the child’s precise age is known, he will be found to be shorter than normal. Except in cases of gross oedema, the child will be lighter in weight than normal. Usually between 60 and 80 percent of standard. These signs may be obscured by oedema or ignorance of the child’s age.
(iii) Wasting of muscles
Wasting of muscles is also typical but it may not be evident because of oedema.
(iv) Oedema
Oedema causes swelling owing to the fluid in the tissue, and is always present. It usually starts with a slight swelling of the feet and often spreads up the legs (see Fig.4.2). Later, the hands, the scrotum and the face may also swell. To diagnose the presence of oedema, press with your finger or thumb over the stun bone, for example above the ankle for about 30 seconds. If a dent (pit) remains after the thumb is removed, oedema is present. If oedema is present the pit formed takes a few seconds to return to the level of the surrounding skin.
Figure 4.2: A child with Kwashiorkor. This child shows oedema of the legs and face, dermatosis of the thigh, arm, and back. The oedema masks and muscle wasting.
(v) Irritable child
The child is usually miserable and apathetic. Irritable when being moved or disturbed. He prefers to remain in one position and is nearly always miserable. He has no appetite and is difficult to feed.
(vi) Hair changes
The hair of a normal African child is usually dark black, coarse in texture and has a healthy sheen that reflects light. In kwashiorkor, the texture often changes, with the hair becoming silker and losing its tight curl. At the same time it lacks luster, is dull and lifeless, and may change colour to brown or reddish brown or grey. It becomes sparse, and is easily pulled out. On examination under a miscroscope, plucked hair exhibits root changes and a narrower diameter than normal hair. The tensile strength of the hair is also reduced.
Figure 4.3: Oedema in Kwashiorkor. Unhappy and irritable child.
(vii) Skin changes
The skin, especially of the face, may be considerably lighter in colour than that of either parent. In some cases a dermatosis develops; this tends to occur first in areas of friction or of pressure, for example, the groin, behind the knees and at the elbow. Darkly pigmented patches appear, which may peel off or desquamate, rather like old sunbaked, blistered paint. This observation has given rise to the term “flaky paint dermatosis” particularly around the large joints like the elbows. (see Fig. 4.4): Underneath these flakes are atrophic depigmented areas that may resemble a healing burn. These areas may become secondarily infected. Skin cracks leading to ulcerations may also occur.
(viii) Diarrhoea
Stools are frequently loose and contain undigested particles of food. Sometimes they are offensive, watery, or blood-stained.
(ix) Anaemia
Few cases do have some degree of anaemia. This is due to lack of the protein required to synthesize blood cells. Anaemia may be complicated by iron deficiency, malaria, hookworm, etc.
Figure 4.4: Flaky-paint dermatosis of kwashiorkor
(x) Hepatomegaly
The liver may be palpably enlarged. This is due to fatty infiltration of the liver, which is always found post-mortem in cases of kwashiorkor.
(xi) Moonface
The cheeks appear to be swollen either with fatty tissue or oedema fluid, giving the characteristic appearance known as “moonface”.
(xii) Signs of other deficiencies
In kwashiorkor, some subcutaneous fat is usually palpable. The amount of this fat gives an indication of the degree of energy deficiency. Mouth and lip changes, characteristic of vitamin B deficiency, are quite commonly found. Xerosis or xerophthalmia due to vitamin A deficiency is occasionally seen.
(xiii) Findings in special laboratory tests
Serum proteins are reduced, the albumin content being more affected than the globulin. The serum amylase is reduced. Examination of duodenal juice reveals reduction in pancreatic enzymes.
Kwashiorkor is an extremely serious disease, and is a frequent cause of death in young children. Many mild cases occur that are not noticed by the parents, and therefore are never diagnosed. In these, recovery occurs if the child receives more protein and an adequate intake of energy. In severe cases with any of the above symptoms and signs, the outcome is likely to be fatal unless the child receives proper treatment. In all cases there is fatty infiltration of the liver but whether this results in any added risk of liver disease later is not known.
Differential diagnosis
In trying to make a diagnosis, the conclusion that the child has kwashiorkor does not rule out other diseases also being present.
(i) Nephrosis
If oedema is the main symptom of nephrosis, the diseases may be confused with kwashiorkor. In nephrosis, however, the urine contains much albumin, and also casts and cells. In kwashiorkor, there is usually only a trace of albumin. If flaky-paint dermatosis or other signs of kwashiorkor are present, the diagnosis is established. Ascites is frequently seen in nephrosis, but only rarely in kwashiorkor. In Africa kwashiorkor is a much commoner cause of oedema than is nephrosis.
(ii) Severe hookworm anaemia
Oedema may result from hookworm anemia alone. In young children kwashiorkor is often also present. In pure hookworm anaemia, there would be no skin changes other than pallor. In all cases, the stools should be examined.
(iii) Pellagra
This is rare in young children; the skin lesions are sometimes similar to those of kwashiorkor, but in pellagra they tend to be on areas exposed to sunlight (not the groin, etc). There may frequently be diarrhoea and weight loss, but no oedema, hair changes, etc.
How do we manage a child with kwashiorkor?
Management of a child with kwashiorkor
Do Activity 4/3. Spend 10 minutes on it.
ACTIVITY 4/3
Explain how you would manage a child with kwashiorkor at your health
facility.
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………….
…………………………………………………………………………………
This is how you would manage a child with kwashiorkor.
(i) Hospitalization
A child with severe kwashiorkor is an emergency.
All severe cases should, if possible, be admitted to hospital with the mother and careful examination is made to reveal any infection. This will include a thorough clinical examination. Stool, examination for worms and parasites, and blood examination for haemoglobin and malaria parasites should be performed. The child should be weighed and measured.
On admission therefore, you should do the following:
Take a history and examine the patient. Check for early signs of xerophthalmia. (v) Assess the degree of dehydration and treat. (vi) Examine for associated infections and infestations, (vii) Since malaria is endemic in most districts in Kenya, give a suppressive dose of Fansidar and Chloroquine on admission as a routine. (viii) Give one intramuscular injection of 100,000 IU Vitamin A or one oral dose of 200,000 IU Vitamin A. Give a second dose orally on the second day. Give half doses to children under one year. (ix) If the haemoglobin is below 3 g per 100 ml, do blood transfusion. (x) Start dietary treatment as soon as the child is no longer dehydrated. Some suitable milk feeds are given in the section of diet below.
(ii) Diet
Dried skim milk (DSM) powder often forms the basis of treatment. DSM may most simply be reconstituted in hospital by adding:
1 teaspoonful of DSM powder; to 25 ml of boiled water, and mixing thoroughly. The child should receive 150 ml of this mixture per kg body weight per day, given in six feeds at approximately 4-hour intervals. The milk mixture should be fed to the child with a feeding cup or a spoon. You can do this only if the child has sufficient appetite, is able to cooperate and is well enough. If not, the same mixture is best given through a nasogastric tube. This tube should be made of polythene. It should, be about 50 cm in length and have an interval diameter of 1 mm. It is passed through one nostril into the stomach. The protruding end should be secured to the cheek either with sticky tape or zinc oxide plaster. The tube can safely be left in position for 5 days. The milk mixture can best be given as a continuous drip, as for a transfusion.
Alternatively you can administer the milk mixture intermittently using a large syringe and a needle that fits the tube. You can then give the milk mixture in 4-hourly feeds. Before and after each feed, you should inject 5 ml of warm, previously boiled water through the lumen of the tube to prevent blockage.
There are better mixtures than the plain DSM which can all be administered, however, in exactly the same way. Most of these contain a vegetable oil e.g., simsim, and cottonseed oil, casein (pure milk protein, e.g., “Casilan-Glaxo”), DSM and sugar. The vegetable oil increases the energy content of the mixture, and appears to be better tolerated than the fat of full cream milk. Casein increases the cost of the mixture but, as it often serves to reduce the period in hospital, the money is well spent.
A good and easily remembered formula for sugar/Casein/Oil/Milk (SCOM) mixture is: 1 part sugar, 1 part casein.
1 part oil 1 part DSM and Water added to make 20 parts. A stock of the dry SCOM mixture can be stored for considerable periods of time in a sealed tin.
To make a feeding, the desired quantity of the mixture is placed in a measuring jug and water added to the correct level. Stirring or, better still, whisking will ensure an even mixture. The amount to be given is the same as the pure DSM mixture previously mentioned, i.e., 150 ml of liquid mixture per kilogram body weight per day. This provides about 28 Calories, 1 g protein, and 12 mg potassium per 30 ml of made-up liquid feed.
Examples of diet treatment:
(a) A 5-kg child on plain DSM mixture
We have said that a child who is on DSM should receive 150 ml of the mixture per kg body weight per day. For a child who weighs 5 kg, multiply the child’s weight by 150 ml. This gives you the amount of DSM to be given per day.
5 kg x 150 ml per day = 750 ml per day. 750 m is given in six feeds that is, one every 4 hours.
750 ml divide by 6 given you how much DSM to give per feed. 750 ml ÷ 6 = 125 ml per feed. ml per feed. The DSM liquid mixture is made by adding 5 teaspoonfuls of DSM powder to 125 ml of boiled cool water.
(b) A 5-kg child on SCOM mixture
To get the amount of SCOM mixture to give to a child you do exactly as I described for DSM.
5 kg x 150 ml per day = 750 ml per day 750 ml ÷ 6 = 125 ml per feed. The liquid SCOM mixture is made up by adding 5 teaspoonfuls of SCOM mixture to 125 ml of boiled cool water. Both liquid mixtures may be administered by spoon, feeding cup or by intragastric tube.
Days in Center Type of feed Daily dosage Divided into 1. Half-strength milk feeds 150 ml/Kg body weight 12 feeds 2 Half-strength milk feeds 150ml/Kg body weight 8 feeds 3 and 4 2/3 Strength milk feeds 150 ml/l/Kg body weight 8 feeds 5 and onward Full-strength milk feeds 150 ml/Kg body weight 6 feeds (iii) Medication
• Give Penicillin or some other antibiotics to all serious cases of kwashiorkor, e.g., Benethamine Penicillin at 500 000 units, intramuscular, daily for 5 days.
• In malarial areas, an antimalarial is desirable. Give half a tablet (125 mg) of Chloroquine daily for 3 days, then half a tablet weekly. In severe cases and when vomiting is present, give Chloroquine by injection.
• Potassium is desirable if dehydration exists, for it will serve to correct the electrolyte imbalance, Give 0.5 g Potassium Chloride (about 3 teaspoonfuls) in water, three times a day.
• If anaemia is very severe, you should treat it by blood transfusion and by intramuscular iron injection, using Iron dextran for example, Imferon, 1 ml daily for about 5 days. In other cases you should give Ferrous sulphate mixture or tablets. • If a stool examination reveals the presence of hookworm, roundworm (Ascaris) or other intestinal parasites, then you should give an appropriate anthelmintic drug after the general condition of the child has improved.
• If vomiting persists, give feeds in smaller and more frequent amounts.
It is important to stress that every child with this disease must be treated on his or her merits as an individual. On the above regime, a serious case of kwashiorkor would usually begin to lose oedema during the first 3 to 7 days, with consequent loss in weight.
During this period, the diarrhoea should ease or cease, the child becomes more cheerful and alert, and skin lesions begin to clear.
When the diarrhoea has stopped, the oedema disappeared, and the appetite returned, it is desirable to stop tube-feeding, if this method has been used. The same SCOM or plain DSM mixture can be continued with a cup and spoon, or feeding bowl. A bottle and teat should not be used. If anaemia is still present, the child should now start a course of receiving iron by mouth. Half a tablet (125 mg) of Chloroquine should be given weekly.
As recovery continues, usually during the second week in hospital, the patient gains weight. While continuing to supply milk, you should gradually introduce triple mix diet. This should aim at providing the necessary energy, protein, minerals, and vitamins for the child. We shall learn how to prepare porridge and triple mix diet in Unit 7.
To avoid disease recurrence, ensure that the mother participates in the feeding at this stage. You must tell her what the child is getting and why. Her cooperation is much more likely if the hospital diet of the child is based mainly on products that she uses at home.
This is not feasible in every case in a large hospital, but the diet should at least be based on locally available foods. Thus in a maize-eating area, for example, the child would now receive a maize gruel with DSM added. For an older child, crushed groundnuts can be added twice a day or, if custom prefers, the child can eat roasted groundnuts. A few teaspoonfuls of ripe papaya, mango, orange or other fruit can be given. At one or two meals per day, a small portion of the green vegetable and the beans, fish or meat that the mother eats can be fed to the child after having been well scapped. If eggs are available and custom allows their consumption, the mother can watch the process of boiling or scrambling an egg for the child. Alternatively, a raw egg can be broken into some simmering gruel porridge.
Protein-rich foods such as beans, peas, groundnuts, meat, sour milk or eggs are all important because they build and repair the body. Often protein-rich foods of animal origin are relatively expensive. However, good mixture of cereals, legumes and vegetables serves just as well. If suitable vitamin-containing foods are not available, then a vitamin mixture should be given, because the plain DSM and SCOM mixtures are not rich in vitamins.
The above are just examples. If the diet of the area is based on bananas, these can be used instead of maize, in which case protein-rich supplements are even more important.
The child, after discharge from hospital, should attend the Outpatient under-fives Clinic regularly, and should follow the regime for mild cases described below.
When mild or moderate cases of kwashiorkor are treated at home and not in the hospital, they should, if possible be followed in the Outpatient Department or clinic. It is much better if such cases can attend separately that is, on some special afternoon or at a child-welfare clinic, rather than in the tumult of most outpatient sessions. It is desirable to have a relaxed atmosphere, you should have time to explain matters to the mother and see that she understands what is expected of her. It is useless just to thrust a bag of milk powder or other supplement at her.
Treatment as an outpatient should be based on the provision of a suitable dietary supplement. In most cases, it is best that this supplement be given as part of the diet. The child should be weighed and the mother told how many teaspoonfuls of supplements to give per day, and shown a teaspoon. Many supplements are best provided by adding them to the usual food, such as porridge, rather than separate preparations. This is certainly so with powdered milk. The mother should be asked how many times a day she feeds the child. If he is fed only at family mealtimes, which is often only twice a day, then she should be told to feed him two extra times.
If facilities exist and it is feasible, the SCOM mixture can be used for outpatient treatment. This is best provided ready mixed in sealed polythene bags.
4.4.3 Marasmus
Description
Marasmus is another severe form of protein-energy malnutrition. Whereas in kwashiorkor the main deficiency is protein, in marasmus the main deficiency is energy/calories and other nutrients. It is a form of starvation. Marasmus normally occurs during the first two years of life.
Causes of marasmus
What are the causes of marasmus?
The possible underlying causes of marasmus include:
(i) Infectious and parasitic diseases of childhood.
These include measles, whooping cough, diarrhea, malaria and other parasitic diseases. Chronic infection such as tuberculosis also leads to marasmus.
(ii) Premature birth, mental deficiency and digestive upsets (malabsorption, vomiting, etc.).
(iii) Early cessation of breast-feeding.
This may be due to death of the mother, pregnancy, failure of lactation, separation of the mother from the infant because of family problems or because she is a working mother, etc.
(iv) Mother’s desire to feed her baby from the bottle rather than the breast.
She may be influenced by advertisements or alien cultures into believing that this is sophisticated or superior and also ease of using a bottle.
(v) The family having insufficient income
The family having insufficient income to buy enough milk to feed a baby properly. The tendency therefore is to over dilute a purchased mixture. Similarly, few households have running water or the other items in their homes that facilitate the sterile preparation of milk bottles for an infant. As a result of improperly cleaned feeding bottles, the child commonly develops gastrointestinal infections, which starts the vicious circle leading to marasmus.
(vi) Prolonged breastfeeding without introduction of other foods
Another cause of marasmus found in certain parts of Africa is prolonged breast-feeding without the introduction of other foods, or enough of other foods. It is unusual for a mother to be able to produce sufficient breast milk to supply all the energy and other nutrients necessary for an infant over 6 months of age.
(vii) Many children in large families like in kwashiorkor.
Like in Kwashiorkor there is often less food for each person. The smaller children may be neglected because the mother has too much work to do.
(viii) Delay in introducing additional food.
Breast milk is best and should be given up to 2 years of age. However, other foods should be added after 6 months and increased in amount as the child grows older. If this is not done growth will slow, and this may lead to malnutrition.
But how can one recognize a child with marasmus?
Clinical signs of marasmus
Do Activity 4/4 below. Spend not more than five minutes on it.
ACTIVITY 4/4
Outline five clinical signs of marasmus.
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………….
…………………………………………………………………………………
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………….
…………………………………………………………………………………
A child with marasmus presents with the following signs:
(i) The child fails to grow properly. The child has severely retarded growth. If the age is known, the weight will be found to be extremely low by normal standards (below 60 percent of the standard).
(ii) In severe cases the loss of flesh is obvious. The ribs are prominent, the belly, in contrast to the rest of the body, may be protuberant, the face looks like that of an old person, and the limbs are very emaciated. The child is “skin and bones”. An advanced case of the disease is unmistakable, and once seen is never forgotten (see Figure 4.5).
(iii) The muscles are always extremely wasted. There is little if any subcutaneous fat left. The skin is loose and seems to be too big for the body. It hangs in wrinkles, especially around the thighs and buttocks where the muscles should be thick. When taken between forefinger and thumb will reveal the absence of the usual layer of adipose tissue.
(iv) Children with marasmus are quite often not disinterested like those with kwashiorkor. Instead the deep sunken eyes have a rather wide-awake appearance (see Fig. 4.5 and 4.6). Similarly, the child may be less miserable and less irritable.
(v) The child usually has a good appetite In fact, like any starving being, he may be ravenous. He often violently sucks his hands or clothing or anything else available. Sometimes he is heard making sucking noises.
(vi) Loose stools Stools may be loose, but this is not a constant feature of the disease. Diarrhoea of an infective nature, as mentioned earlier, may commonly have been a precipitating factor.
(vii) Anaemia Anaemia due to iron, protein and other deficiencies is usually present.
(ix) In contrast to kwashiorkor, there is no oedema and no flaky-paint dermatosis in marasmus. There may be pressure sores, but these are usually over bony prominences, not in areas of friction. Hair changes similar to those in kwashiorkor can occur. There is more frequently a change of texture than of colour. Dehydration, although not feature of the disease itself, is a frequent accompaniment of the disease, and results from severe diarrhoea and sometimes vomiting.
Figure 4.5: Severe nutritional marasmus
Figure 4.6: Marasmus, showing loss of subcutaneous tissue
but bright, wide-awake eyes.
Differential diagnosis
Tuberculosis and AIDS
Tuberculosis and AIDS may also cause muscle wasting, failure to thrive and anaemia.
Management of a child with marasmus
Treatment for marasmus is similar to that of kwashiorkor. It is especially desirable, however, to see that adequate energy is supplied. It is very important that you find the underlying cause. If this is an infective diarrhoea, dehydration may require special treatment with intravenous fluids or with intragastric tube feeding, but using a much more dilute mixture than that recommended for kwashiorkor. If it is impossible to find a vein, then you can give fluids into the peritoneal cavity. Simultaneously you should give Sulphonamides or Tetracycline orally. Once the diarrhoea has been controlled, a nutritious high-energy diet is essential. The use of vegetable oil with DSM is even more important here than in kwashiorkor, as it will ensure a high energy intake.
Examination for tuberculosis is desirable. If there is any doubt, you should perform a tuberculin test and if this is positive a chest X-ray should be taken.
Prognosis
The cause and the severity of the disease will determine the prognosis. A child with severe marasmus and lungs grossly damaged by tuberculous infection obviously has poor prospects. However, for a child with no other infection and with mild marasmus, has better prospects. In any event response to treatment is likely to be slower than with kwashiorkor. It is often difficult to know what to do when the child is cured, especially if the child is under 1 year old. There may be no mother or she may be ill, and certainly she will have insufficient breast milk. Instructions and nutrition education of the person who will be responsible for the child are vital. If the child has been brought by the father, then some female relative should spend a few days in the hospital being taught how to look after the child before the child is discharged.
You should give instructions in feeding the child with a spoon or cup, and not from a bottle unless the infant is under 3 months of age. The best procedure is usually to provide a thin gruel made from the local staple plus 2 teaspoonfuls of DSM, or some other protein-rich supplement, and 2 teaspoonfuls of oil per kilogram body weight per day. You should give instructions regarding other items in the diet if the child is over 6 months old. The mother or guardian must attend the hospital or clinic at weekly intervals if she lives within, say, 10 kilometres, or at monthly intervals if far away. You should give at each visit supplies of a suitable supplement to last for slightly longer than this. The child can be put on other foods, as mentioned in the discussion of treatment for kwashiorkor.
It is essential that the diet provide adequate energy and protein. Usually 120 Calories and 3 g of protein per kilogram of body weight per day are sufficient for long-term treatment. Thus a 10-kg child should receive about 1200 Calories and 30 g of protein daily. It should be noted that a marasmic child, during the early part of recover, may be capable of consuming and utilizing 150-200 Calories and 4-5 g of protein per kilogram body weight.
Having discussed underweight, kwashiorkor and marasmus, let us discuss marasmic-kwashiorkor.
4.4.4 Marasmic - Kwashiorkor
Description
It is emphasized that kwashiorkor and nutritional marasmus are forms of protein-energy malnutrition. Kwashiorkor is the syndrome where the main deficiency is protein, while in marasmus the deficiency is mainly energy. In some cases the children are half way between kwashiorkor and marasmus. They might perhaps be very thin like a marasmic child and at the same time have oedema like a child with kwashiorkor. These children are said to have marasmic-kwashiorkor.
In some areas, most children will be like this and there will be a few with either “pure” kwashiorkor or “pure” marasmus.
Clinical signs of marasmic-kwashiorkor
(i) The child will be very thin like a child with marasmus. (ii) The child will have oedema like a child with kwashiorkor.
Causes of marasmic-kwashiorkor
Since a child with Marasmic-Kwashiorkor is half way between kwashiorkor and marasmus, the causes of marasmic-kwashiorkor therefore, are the same as those for kwashiorkor and marasmus. To remind you these causes, review the sections on the causes of kwashiorkor and marasmus.
Management of a child with marasmic-kwashiorkor
Since a child with marasmic-kwashiorkor has both marasmus and kwashiorkor, the treatment is the same as for marasmus and kwashiorkor. However, each patient should in any case be treated as an individual according to the clinical and other findings.
4.4.5 Mild or Moderate PEM (Wasting and Stunting)
The health worker finds it easy to diagnose both kwashiorkor and nutritional marasmus. These however are the extreme cases of protein-energy malnutrition, which may require hospital treatment and where the outlook for the child may be grave. Much commoner than these severe forms of PEM are what have been termed as mild or moderate PEM.
Clinical signs of a child with mild or moderate PEM
Stop for a while and do Activity 4/5 below. You should spent not more than five minutes on it.
ACTIVITY 4/5
Discuss with one or two of your colleagues what would make you
suspect or conclude that a child has mild or moderate PEM. Write
down all the points mentioned.
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………….
…………………………………………………………………………………
………………………………………………………………………………….
Children with mild or moderate PEM do not have the gross oedema of kwashiorkor nor the emaciated appearance of nutritional marasmus. But they do have evidence of malnutrition and they are at special risk of developing the more severe forms of PEM, or of succumbing to an infectious disease. In most communities in Africa fewer than 5% of children at any one time have kwashiorkor or nutritional marasmus. In these same communities usually at least 30% and sometimes as high as 75% of children have mild or moderate PEM. These present as wasting and stunting. A child is said to be wasted when their weight is less than children of the same height and sex. A child is stunted if their height is shorter than children of the same age and sex.
The main feature of mild or moderate PEM is a failure to grow and develop optimally. Anthropometric measurements are used in determining these conditions. Anthropometric measurements will be discussed later in another unit when discussing Growth Promotion Monitoring.
Management of mild or moderate PEM
A child with mild or moderate PEM can be managed at home using locally available foods. A child should be given food adequate in amount for protein, energy and all the other nutrients.
You should therefore, teach and show the mother appropriate food for a child and how to prepare it.
Children at risk of malnutrition Let us now discuss the categories of children who are likely to become malnourished.
4.5 Categories of children who are likely to become malnourished
Do Activity 4/6 below. It should take you about 5 minutes to accomplish it.
ACTIVITY 4/6
List the categories of children who are most likely to become
malnourished.
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………….
The categories of children who are most likely to become malnourished include:
(i) Children between 6 months and 5 years of age. This is because they are growing fast. They may get malnourished easily if they do not get enough of the right foods for their needs.
(ii) Children from a large family. This is because in a family there is less food for each person. Because the mother has so much work to do she may not pay enough attention in the feeding of young children.
Figure 4.7: Many children in a family
(iii) If a mother has pregnancies too close together, the health of both babies, and the mother, will suffer. She will have less breast milk to feed the baby and the older child will get less time and care and may become malnourished.
(iv) Babies who are born small (less than 2 kilograms) are likely to become malnourished.
(v) Babies who do not get enough breast milk may become malnourished.
(vi) Breast milk is the only food babies need for the first four months of life, but from 6 months they need other foods, such as fruits, fruit juices and porridge. If they do not get enough of these other foods at the right time, they will not grow properly and they may become malnourished.
(vii) If a child catches an infection such as diarrhoea, malaria, whooping cough or measles, he is likely to become malnourished, because of low appetite, high fever and vomiting.
(viii) By the time a baby is 3 months old he should be about 1.5 kilograms heavier than he was when he was born. If he gains less, he may become malnourished. Ceasing breastfeeding too early can cause the baby to stop growing.
(ix) Children from a family or community that lacks knowledge on proper child feeding. Children often do not get enough of the right kinds of food, and are likely to become malnourished.
Figure 4.8: Poor family
4.6 Protein-Energy malnutrition in adults
Protein-Energy-Malnutrition does not occur in children only, adults too can get it. Let us now discuss PEM in adults.
Although the term “adult kwashiorkor” has been used in some publications, it is probably better to reserve the word kwashiorkor for the disease in children, and use adult malnutrition.
Signs and symptoms of an adult with PEM
Do Activity 4/7 before you proceed. Spend 5 minutes on it.
ACTIVITY 4/7
I am sure you must at one time come across an adult with PEM.
Discuss with two to three of your colleagues at your place of work the
signs and symptoms of an adult with PEM. Write down the answers
each member gives.
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………….
…………………………………………………………………………………
PEM in adults is very common in the war affected areas especially at the Displaced peoples’ camps because these people have no access to food as they were before. It also occurs in chronic alcoholics.
An adult with kwashiorkor may present with the following signs and symptoms:
(i) The patient is markedly under weight for his height (unless grossly oedematous), the muscles are wasted and there is reduced subcutaneous fat.
(ii) Mental changes are common, with the patient usually disinterested and appearing to be in a dream world. It is difficult to attract his attention and equally hard to keep it.
(iii) Reduced appetite and the patient is very weak.
(iv) Oedema which may mask the weight loss, wasting and lack of subcutaneous fat. Oedema is commonest in the legs and in the scrotum in male patients, but any part of the body may be affected. The face is often puffy. This has been termed as “famine oedema” because it occurs where there is starvation due to famine, war or insurgency.
(v) Frequent, loose, offensive stools may be passed.
(vi) Slightly distended abdomen, and when palpated, the organs can be very easily felt through the thin abdominal wall.
(vii) Hair changes. There are more often changes of texture than of colour, though reddish brown hair is sometimes seen. The hair is much softer and silkier than normal, less curly and loses its reflective power and sheen. It may be a dull black rather than a shiny black, similar to black shoes when the polish is put on, but before they have been shined.
(viii) Dry and scaly skin.
(ix) Swelling of both parotids.
(x) Anaemia.
(xi) Low blood pressure.
(xii) A trace of albumen in the urine.
Although the above signs and symptoms are usually present, it is very difficult to separate them from many other signs and symptoms observed in other disease conditions. Other signs and symptoms present resulting from other disease processes and deficiencies include:
(i) Angular stomatitis, soreness and redness of the tongue due probably to riboflavin deficiency.
(ii) Blood stained stools or severe diarrhoea due to bacillary (or sometimes amoebic) dysentery or tropical ulcers, in areas where these are common.
(iii) Heavy loads of hookworms and other intestinal parasites.
(iv) Malaria infection and splenomegally due to some of the above causes.
Management of adults with PEM
How would you manage an adult with PEM?
The management for adult protein-energy malnutrition is on exactly the same lines as that in children. A mixed diet high in protein and energy, as prescribed for children recovering from kwashiorkor or marasmus, can be introduced earlier. Care must be taken with the introduction of beans, which although they are desirable because of their high protein content and availability, may be indigestible and increase flatulence.
Particular care must be taken to treat allied infections. In severe anaemia, blood transfusion may cause rapid all-around improvement and shorten the stay in hospital.
It is important that you advice the patient to have bed rest.
Differential diagnosis
Anaemia Severe anaemia may also cause oedema. In protein-energy malnutrition in adults, there is less dyspnoea and usually no cardiomegaly. Other features such as hair changes and parotid swelling are common in adult PEM but not in anaemia.
However, as lack of dietary protein appears to be a cause of anaemia, the two conditions are closely related.
Effects of PEM on adults Adults with severe PEM: • get mental disorders. • get low blood pressure. • are very weak and non-productive in the community
Now let us discuss the effect of Protein-Energy-Malnutrition on the population.
4.7 Effects of Protein-Energy Malnutrition on the population
Do Activity 4/8 below before you continue reading. Spend about 5 minutes on it.
ACTIVITY 4/8
What are the effects of poor nutrition on the population?
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
………………………………………………………………………………..
…………………………………………………………………………………
As malnutrition has wider causation, its effects are also multidimensional in nature. These include:
• Ill health and disease. • Poor productivity of the malnourished individuals. • High health budgets at household, district and national levels. • Poverty perpetuation (a vicious circle). • Poor growth and development of children. • Poor academic performance and attendance of children at school. • Poor obstetrical performance in females due to stunting, hence obstructed labour.
But what are the effects of PEM on children?
Effects of PEM in children
The effects of under nutrition on children are potentially serious, depending on how severe it is, how long it lasts, and the age the child.
Children with severe kwashiorkor and marasmus:
• Often die. Kwashiorkor is particularly difficult to treat.
• Have poor growth and development.
• Are often anaemic and suffer from xerophthalmia, an eye condition that can eventually end in blindness.
• Have poor academic performance and attendances of children at school.
What strategies can we use to promote proper nutrition in a community?
4.8 Strategies for promoting proper nutrition in a community
Good nutrition is apparent when a child is getting enough food in quality and quantity. The following strategies can be employed to counteract malnutrition.
Proper education
• Basic education is a pre-requisite to child nutrition and care. Therefore advocacy should be done for equal chances of education for both boys and girls to make better parents/caretakers.
• Spreading knowledge on nutrition and child health in schools, families, communities etc should be done, to improve on attitudes and practices, with emphasis on proper nutrition in the most vulnerable groups that is, the mothers and children.
• Sensitization of communities on the importance of adequate intake of nutritional supplements.
Healthy environment
• Availability and easy access to safe and adequate water for drinking, cooking, cleaning etc.
• Safe disposal of wastes like using latrines and proper disposal of refuse.
• Vector and vermin control is important for nutrition and general health.
Maternal and childcare
• Prevention of low birth weight (< 2.5kg) and prematurity through adequate antenatal care for safe motherhood. For example, proper nutrition and supplementation, preparation for successful breast feeding, de-worming and non-drug/alcohol abuse.
• Prevention of intrauterine infections such as malaria and HIV infection through community sensitization.
• Proper ante-natal care for example, conducting safe delivery and care for the new-born.
• Promotion of exclusive breast-feeding in the first 6 months of age, and complementary feeding after 6 months at the same time continuing to breast-feed at least up to 2 years. Breastfeeding of children born of HIV positive mothers should be done according to HIV infant feeding guidelines.
• Promotion of special nutritional care for sick children.
Healthy social and family life
• Family size: All children are more likely to receive enough attention and food if the family is small. Therefore, modern family planning methods should be encouraged as to have quality families or children.
• Younger children need to be accorded more care. If both parents are away efforts should be made to give children enough food and attention by the caretaker. • Distribution of money, work and food within the family should be equitable. For example, pregnant mothers and growing children need more high quality energy and protein foods for their increased body demands. However, children need this food in small portions frequently, because they can’t digest large quantities of food at once. Secondly, pregnant mothers should have light exercises and enough rest.
• Care for children from broken, incomplete or underprivileged families should be done through social integration and communal care.
Proper agriculture
• Allocation of money and other resources for agricultural improvement, education and health.
• Create conditions for accessing land for cultivation and growing of enough food.
• Clearing of land at the right time.
• Planting of the right and different seeds (diversification) and weeding should be ensured if one is to get optimal and value harvest.
• Irrigation and use of fertilizers should be employed where needed and advice sought from agricultural extension workers.
• Harvesting at the right time and proper handling of harvests through storage, processing and preparation so that nutrients are preserved and there is enough food in times of hunger.
• Communal production and fair distribution/marketing of food for equity purposes through women groups and co-operative societies.
• Creation of jobs for those who do not have access to land so that they can have income to purchase food.
• Food distribution at house hold levels should be equitable, giving children and pregnant mothers priority.
Public health measures
• Prevention and treatment of perinatal infections of mothers and babies especially Chlamydia, HIV and sexually transmitted diseases.
• Immunization against vaccine preventable diseases like measles, tuberculosis, and whooping cough which contribute to malnutrition in children.
• Emphasis on growth promotion and monitoring activities using the “Child growth curve” and initiate remedial measures for faulty growth.
• Early detection and effective treatment of acute diseases like diarrhoea and acute respiratory tract infections can be used to prevent or control malnutrition.
Child with severe PEM should be identified and referred to appropriate referral units/nutrition rehabilitation centres for expert management.
Make appointment with your tutor/mentor to come and assess you while you carry out Activity 4/9 and 4/10. These Activities will help you to promote proper nutrition in your service area.
Make all the necessary preparations before your tutor arrives. Collect all the materials you will need before hand. For example teaching aids like posters, and real food.
The Activity 4/9 should take you 30 minutes. This is a critical activity.
ACTIVITY 4/9
Give health education talk to a group of parents at your health facility
on Protein Energy Malnutrition (PEM) under the following headings:
• Common types of PEM. • Causes of each type of PEM and how to prevent it.
This Activity 4/10 should take you 40 minutes to complete. Make all the preparations before your tutor arrives. The activity is to be carried out in the community. So make sure the community is well mobilized and keep the appointment and time.
ACTIVITY 4/10
Give a talk to the community on:
(i) The causes of PEM
(ii) Strategies for promoting proper nutrition in the community.
Before we come to the end of our Unit on Protein-Energy Malnutrition, let us have a summary of what we discussed.
Summary
In this unit, we defined nutrition as the Science of food, the nutrients and other substances within food, their actions and interactions and balance in relation to health and disease.
Nutrition security appropriate quantity and combination of inputs such as food, health services and caretakers time needed to ensure an active and healthy life at all times for all people.
Malnutrition includes a wide range of clinical disorders resulting from an unbalanced intake of energy, protein as well other nutrients. It can present as under or over nutrition.
Protein-Energy Malnutrition is a condition caused by a deficient intake of energy and usually protein.
We named the types of Protein-Energy Malnutrition as under weight, kwashiorkor, marasmus, marasmic –kwashiorkor, wasting and stunting.
Under weight is the mildest form of PEM and can be detected only by checking the weight of the child and plotting it on the Growth Chart.
Kwashiorkor is a severe form of PEM characterized by oedema, usually starting in the feet and legs, sometimes accompanied by skin rash. The child is usually irritable when being moved of disturbed. Skin cracks leading to ulcerations may also occur. The diet is usually deficient in protein and also in carbohydrate.
In marasmus, the main deficiency is food in general. The child is skin and bones. The face is like that of an old person. There is little subcutaneous fat left. The skin hangs in wrinkles, especially around the buttocks. The child’s appetite is good and he/she is always alert.
A child with marasmic-kwashiorkor is half way between marasmus and kwashiorkor.
We discussed the causes of PEM as:
• Inadequate food intake. • Diseases like measles. • Food insecurity and limited access to foodstuffs. • Poor sanitation and inadequate health services. • Inadequate maternal and child care practices, among others. Finally, we said that the strategies for promoting proper nutrition include:
• Advocating for equal chances of education for both boys and girls. • Having healthy environment, which include, proper excreta and refuse disposal and availability of safe water. • Proper antenatal and postnatal care and safe delivery. • Encouraging the use of Family Planning methods. • Prevention and treatment of perinatal infections of mothers and babies and immunization of children and pregnant women.
Take a rest and when you are ready, complete the Tutor-
Good luck!
REFERENCES
1. M.C. Latham, O.B.E Second Edition 1979. Reprinted 1981: Human Nutrition in Tropical Africa.
2. King, H.M. et al, 1988: Nutrition for Developing Countries, Oxyford University press, Nairobi.
3. Wener, D. and Bower B. 1991: Helping Health workers learn, The Hesoeruob Foundation, Polo Alto U.S.A.
4. AMREF Second Edition 1999: Child Health. A manual for medical and health workers in health centres and rural hospitals.
5. Maurice H. King, Felicity M. King et al 1984: Nutrition for Developing Countries.
6. Burgess, Ann 1994: Community Nutrition for Eastern Africa.
7. C.H. Wood, J.P. Vaughan et al 1981: Community Health.
8. WHO. Geneva 1986: Guidelines for training Community Health Workers in nutrition. Second Edition.
9. Margaret Cameron and Yngve Hafvander 1983: Manual on Feeding Infants and young children.