Lesson 4: Common Health Problems of the Newborn
Contents
INTRODUCTION
Perinatal and neonatal problems are now the leading causes of death in children under five years. The baby may have been born at home or a health facility. For babies born at a health facility circumstances around delivery are handled by well trained health workers, while for the one born at home they may not. For all babies, the interval between onset of illness and death can be in a matter of minutes or hours. It is therefore very important for you to recognise and plan for the care of the newborn.
Let us first look at the objectives for this Unit.
|
By the end of this unit you should be able to:
|
Begin by doing the following activity. It should take you five minutes to complete.
| 1
Define the following: Perinatal period……………………………………………………………………… Neonatal period……………………………………………………………………… Normal birth weight………………………………………………………………… Low birth weight (LBW)…………………………………………………………… Very low birth weight (VLBW)……………………………………………………… Extremely LBW (ELBW)……………………………………………………………
|
Now read the following sections and compare what you wrote with the information given.
- Perinatal period is that period from late pregnancy through delivery up to the first 7 days postnatally. Generally the period of pregnancy is not clearly defined but the foetus must be viable.
- Neonatal/newborn period is the first 28 days/four weeks after birth – generally taken as the first month of life.
- Normal birth weight: this ranges from 2500g to 4000g at birth.
- Low birth weight is weight that is less than 2500g at birth.
- Very low birth weight: weight below 1500g at birth.
- Extremely low birth weight: weight below 1000g at birth.
4.1 ORGANIZING CARE FOR SICK &/OR SMALL BABY
| 2
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Compare your response with the following:
- All babies should not wait in the queue;
- Arrange for babies to be seen quickly;
- Assess baby for danger signs before general administrative procedures;
- Manage the danger signs.
4.2 DANGER SIGNS IN THE NEWBORN AND THEIR MANAGEMENT
| 3
List the danger signs you would look for in a newborn? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
I believe your answer included the following danger signs:
- Respiration
- Shock
- Unconscious/ convulsing/spasms
- Unable to breastfeed
- Very or extremely low birth weight.
Let us look at each in turn.
Before you assess a newborn for danger signs, you should place the baby in a warm environment, take a weight and establish an IV line. Then you should manage as follows:
- Respiration
- If the baby is not breathing (apnoea) or is gasping for air (respiratory rate <20/minute) you should start resuscitation immediately;
- If the child has respiratory distress, that is the breathing rate is greater than 60/minute, chest retraction, grunting, central cyanosis, you should give oxygen by nasal prong or nasal catheter
- Shock
Shock can be due to severe blood loss at birth, or dehydration through failure to feed, vomiting or diarrhoea. Dehydration is covered in unit 9 on diarrhoea. For the baby who has lost a lot of blood there will be signs of severe pallor in addition to signs of shock.
The signs of shock include cold hands and feet; capillary refill >3 seconds (this may be difficult to elicit in a baby with severe blood loss because of severe pallor); altered consciousness.
For both causes you should restore circulating blood volume by giving normal saline or Ringer’s lactate at 20mls/kg intravenously as rapidly as possible. Reassess if the child is still in shock repeat the dose. If shock is as a result of severe bleeding, then you should get blood as quickly as possible and transfuse.
- Unconscious/ convulsing /spasms
These could be due to serious bacterial infection, birth asphyxia, neonatal tetanus or bilirubin toxicity. You should establish the cause by taking thorough history and treat accordingly. Control convulsions using phenobarbital preferably IV 10- 20mg/kg give slowly while you watch the breathing.
- Unable to breastfeed
The causes of this include serious bacterial infection, birth asphyxia, or low birth weight (preterm baby). You should give dextrose 10mls/kg IV or nasogastric tube to prevent or treat hypoglycaemia immediately. This can be followed by giving breastmilk as soon as possible according to the condition of the baby.
- Very or extremely low birth weight
These children need to be referred or admitted urgently for specialized care. If you need to refer the child, show the mother the kangaroo in order to keep the baby warm during the journey. You should also pass a nasogastric tube and give expressed breastmilk to prevent hypoglycaemia.
All babies with danger signs will need admission to a unit that can treat them. If the health facility you are working in does not have the necessary staff or equipment to look after them, then you should refer them to the nearest facility that can. Transfer by the quickest means available preferably by ambulance so that you can administer oxygen if the baby has breathing problems.
4.3 COMMON PROBLEMS OF THE NEWBORN
| 4
List common neonatal problems _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now confirm your answers as you read the following discussion.
Birth asphyxia
Birth asphyxia means the baby is not breathing at birth. It is one of the most common problem encountered at delivery. You should anticipate asphyxia when labour has unduly prolonged, if the baby is a breech presentation and if the baby is premature. An important sign of asphyxia during delivery is lack of oxygen in the baby or slowing of the heart rate or meconium (green) staining of the amniotic fluid.
All babies are assessed using the Apgar score. See Table 4.1 on how to assess newborns by Apgar Score. The most important in this score is the heart rate and breathing followed by colour.
Table 4.1: Assessing Newborns by Apgar Score.
| Sign | Score | ||
|---|---|---|---|
| 0 | 1 | 2 | |
| Appearance (colour) | Blue, pale grey | Pink body
Blue extremities |
Pink all over |
| Pulse (heart rate) | Absent | Less than 100 beats/minute | More than 100 beats/minute |
| Grimace (response to stimuli) | None | Grimace (slight) | Cry |
| Activity (muscle tone) | Limp | Some flexion of extremities | Active motion |
| Respiration | Absent | Slow, irregular gasping | Normal |
Classification according to total score: Apgar 7-10 = normal Apgar 4-6 = moderate asphyxia Apgar 0-3 = severe asphyxia
Anybody conducting a delivery must be able to resuscitate a neonate.
Neonatal Resuscitation
Although this is a practical subject that you can only learn by practice, nevertheless I will try to outline the procedure. .
If a baby is not breathing, you should proceed in the following order as quickly and as carefully as possible:
- Note the time;
- Dry and cover the baby;
- Supply heat from above the baby;
- Use a proper size suction catheter (3-4 mm in outer diameter) to clear the airway quickly and thoroughly, especially if the amniotic fluid is meconium-stained;
- Ventilate the baby by Ambu bag or other available bag and mask;
- Ensure the babies face is looking straight upwards to the ceiling;
- Prevent air leak around the baby’s face
- Start by giving 100% oxygen by connecting the oxygen cylinder to the face mask;
- Ventilate at a rate of 40 per minute, leaving as much time for breathing out as for breathing in;
- Allow the baby to breath out! Check to see if the chest and abdomen is moving with ventilation and whether you can hear proper breath sounds;
- Apply external cardiac massage if there is no heartbeat. If this is done simultaneously with the ventilation, then a cycle of respiration to cardiac massage of 1 to 3 or 1 to 4 should be maintained. Unfortunately, external cardiac massage is rarely of value in the newborn. So it is best to concentrate on clearing the airway and ventilating the baby.
If you apply these measures correctly, most babies will respond very well. However, if there is no response after 3-5 minutes, you should give the following:
- If the heart rate is very slow, 0.2 ml/kg of a 1 in 10,000 (0.01%) dilution of adrenaline can also be given intravenously. This dilution is prepared by adding 1ml of a 1 in 1,000 (0.1%) adrenaline solution to 9ml normal saline.
After resuscitation it is important to ask yourself the following questions:
- Did the baby improve as expected from perinatal asphyxia with simple and proper resuscitation or was infection or a congenital abnormality the real cause?
- Did the resuscitation including keeping the baby warm work out well?
- Is the equipment ready for the next baby whose life may depend on it?
If the baby improves, you should keep a close eye on him or her and watch out for convulsions, hypoglycaemia, feeding difficulties, hypothermia and recurrent apnoea.
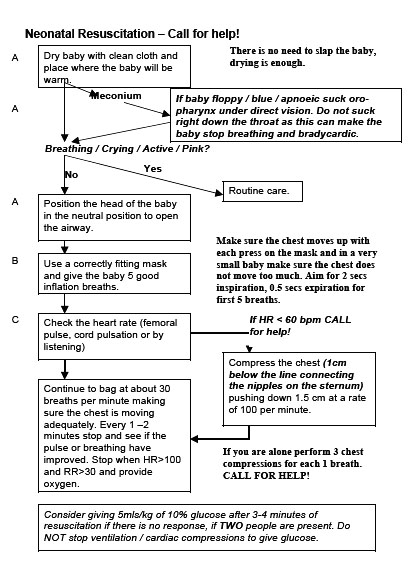
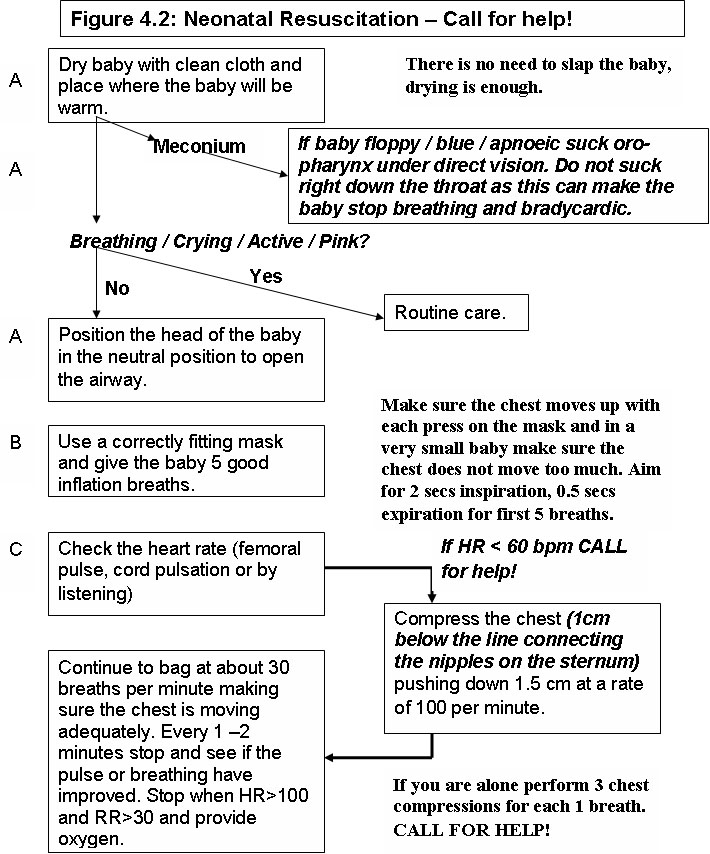
Table 4.2 gives guidelines on how to conduct neonatal resuscitation
Table 4.2: Guidelines on Neonatal Resuscitation (Source: Basic Paediatric Protocols, MOH Kenya)
| 5
List the equipment you would need to resuscitate a newborn _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now compare your list with the one given in the following discussion.
The equipment that one needs to resuscitate a baby includes the following:
- Dry linen (two – one to dry the baby another to cover the baby)
- A firm place (table)
- Source of heat
- Ambu bag
The most important thing in resuscitation is ventilating the baby. You can ventilate using room air. Remember apart from adrenaline you rarely need any other drugs during resuscitation at birth.
Additional information on common baby ailments can be found on the Why do babies cry page.
4.2 Common Infections in the Newborn
The common infections in the newborn are skin, eye and cord infections. You have already covered the diagnosis and management of common eye and skin infections earlier in this course. If the baby has none of the danger signs we discussed earlier in this unit, then you should treat him or her as an outpatients. Let us discuss how to diagnose and manage cord and serious bacterial infections.
Cord infections:
You should always check the cord for signs of infection. Can you remember what the signs are? Write them down before you look them up.
| 6
List down the main signs of a code infection. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now confirm your answers as you read the following discussion.
How do you manage cord infections? How can they be prevented
Severe skin or cord infections may be associated with serious bacterial infection. So always look for systemic signs in all babies.
Serious bacterial infection
This is also referred to as neonatal septicaemia or just sepsis. As already outlined above, the baby will present with one or more of the danger signs. In fact any baby who is not doing well is presumed infected until proven otherwise. Up to 30% of septic babies have associated meningitis without showing signs of meningitis. Thus any sick baby should be suspected of having meningitis and should have a spinal tap for cerebrospinal fluid infection.
| 7
Without looking back can you write down the danger signs? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Well done! Look back at the danger signs we listed earlier and check if you got them right.
In order to manage a baby with a serious bacterial infection you need to use appropriate antibiotic. The first choice is usually a penicillin and gentamicin given IV.
The duration of treatment will depend on the baby’s response. However 7-10 days are usually enough to clear the infection. Before you stop the treatment you should ensure that the baby has had an adequate response to the treatment. If you suspected of proved that the baby had meningitis treat for 21 days.
Pneumonia is often combined with septicaemia. This is usually due to infection of the baby by infected uterine contents. This is likely to happen during the following situations:
- When there is prolonged rupture of the membranes (24-48 hours), especially if a vaginal examination had been performed more than 8 h ours before delivery;
- When the mother has fever (of unexplained origin) during delivery and or foul smelling amniotic fluid.
Neonatal Jaundice
The word jaundice comes from the French word jaune, which means yellow. Neonatal jauncine is a serious disease that needs to be treated appropriately and promptly. We worry about jaundice in the newborn because it can cause brain damage. Before you read on do the following activity. It should take you 5 minutes to complete.
| 8
Write down all the common causes of jaundice in a neonate and the age the jaundice will appear. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now confirm your answers as you read the following discussion.
The common causes include:
- Physiological jaundice
- Blood group incompatibility
- Infections.
Physiological jaundice:
Physiological jaundice appears 2-3 day after delivery and it usually disappears by the 7th to 10th day. More than 50% of term newborns and 80% of preterms will have some jaundice.
When an infant is born it has too many red blood cells. It is a natural process for the baby's body to break down these excess red blood cells, forming a large amount of bilirubin. Bilirubin is formed and released into the bloodstream when red blood cells are broken down. It is this bilirubin that causes the skin to take on a yellowish color.
A newborn's liver is immature and cannot process bilirubin as quickly as it would in an older baby. This slow processing of bilirubin has nothing to do with liver disease. It merely means that the baby's liver is not as fully developed as it should be and this situation usually corrects itself after seven days. The baby is better able to deal with the bilirubin when fully fed and given plenty of fluids, especially breast milk.
In full term babies apart from appearing yellow, the baby is fine. However, preterm babies may need treatment especially if they have intercurrent problems.
Blood group incompatibility
Commonly ABO less commonly rhesus incompatibility. Jaundice appears within the first 24 hours of birth.
Infections
The common infections that cause jaundice are both bacterial or viral. Jaundice can start any time from first 24 hours onwards depending on whether the baby acquires infection before or after birth.
The seriousness of jaundice is determined by the following:
- Age of onset - any jaundice appearing in the first 36 hrs is always serious.
- Depth of jaundice – sometimes the whole body appears yellow. Jaundice starts appearing on the face and spreads out and downwards. By the time the hands and feet appear yellow there is deep jaundice.
- Weight of the baby – the outcome is worse in small/ preterm babies.
- Presence of intercurrent problems such as infection;
- Presence of CNS signs
Treatment of Jaundiced Baby
The treatment of a jaundiced baby includes the following:
- Phototherapy or light treatment. This is the process of using light to eliminate bilirubin in the blood. The light is shone directly on an undressed baby (with diaper on) whose eyes are protected from the light by applying soft eye patches. Once the baby's skin and blood absorbs these light waves, it changes bilirubin into products which can pass through their system.
- Antibiotics if there is infection;
- Exchange transfusion if the bilirubin is high and cannot be reduced quickly using phototherapy;
- Adequate feeding. Babies in phototherapy lose more fluid than normal. Ask the mother to feed frequently and if not able to suck, he or she should be fed using a nasogastric tube or by giving IV fluids.
Low birth weight (LBW)
As I mentioned ealier, a low birth weight infant is a baby whose weight is less than than 2500g at birth. Problems of LBW depend on size at birth and gestation and they include the following:
- Inability to regulate body temperature;
- Breathing problems -respiratory distress or apnoea;
- Inability to feed;
- Prone to infection.
The care we give is dependent on weight as follows:
- Weight 2000-2499g can be cared for as normal weight babies. Some of them may have feeding difficulties. Observe for a day or two before discharging from maternity ward.
- Weight 1750- 1999g extra care is needed. Kangaroo mother care will provide enough warmth unless the baby has another problem. They can be able to breastfeed adequately but some may tire quickly and may need tube or cup feeding.
- Weight below 1750g: these babies have increased risk of respiratory distress, infection, apnoea, hypothermia, and usually not able to feed especially if very low birth weight. They need to be admitted to a specialised area that will cater for their needs. For these babies treat any intercurrent problem and when they stabilise, start kangaroo mother care.
4.3 SUPPORTIVE CARE FOR ALL SICK NEONATES
Some of this has already been mentioned in the preceding sections.
Begin by the following activity
| 9
List the supportive management and how you would monitor the baby _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Compare your response with the following information.
The following is the supportive care that we should give to all sick neonates:
- Temperature Regulation
- Fluid and feed management
- Oxygen therapy
- Prevention of infections
Temperature Regulation
The body temperature determines the survival as well as postnatal growth of a baby. Many LBW infants lose heat quickly and are not able to maintain normal body temperature unless the environment is warm enough.
There are a number of way of ensuring that an infant is warm enough. These include:
- Keeping the baby dry and well wrapped and nurse away from open windows
- Avoiding unnecessary exposure
- Keeping the room warm (at least 25oC)
- Initiating Kangaroo mother care (KMC)
- Using Incubators
Kangaroo mother care is a method of care of preterm infants which involves infants being carried, usually by the mother, with skin-to-skin contact (see Figure 4.1) As you well know incubators are extremely expensive and are not available at all levels of our health care system. A mothers skin temperature is usually at 32oC. Thus if a baby is clothed and close between the mothers breasts, even the smallest LBW baby will remain warm enough. That is why KMC was developed. KMC is more than an alternative to incubator care. Research and experience according to WHO show that:
- KMC is at least equivalent to conventional care (incubators), in terms of safety and thermal protection, if measured by mortality;
- KMC, by facilitating breastfeeding, offers noticeable advantages in cases of severe morbidity;
- KMC contributes to the humanization of neonatal care and to better bonding between mother and baby in both low and high-income countries;
- KMC is, in this respect, a modern method of care in any setting, even where expensive technology and adequate care are available.
Figure 4.1: Kangaroo Mother Care Method
Once a mother is confident in the care of her baby using this method, she can continue it at home under your guidance. You should closely follow-up the mother to ensure the baby is growing and developing properly.
| 10
How do you manage fever in a newborn? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Well I hope you realised that the management of raised temperature will depend on the cause.
Let us look at some of the causes and how to manage them.
- Over heated: (hands and feet warm
(a) In the incubator
- Reduce incubator setting
- Open the portholes
- Measure baby’s temperature preferably 1hrly (3hrly at the most) until it is normal
- Continue adjusting incubator temperature until baby no longer over heated.
(b) Baby clothed/covered:
- Remove covering for 10 minutes then cover lightly
- Sick baby
Look for Sepsis if the hands and feet are cold despite the high temperature. Investigate and treat for sepsis. CNS lesions: birth asphyxia, congenital defects (rare)
General Guidelines
For all babies with high temperature:
Ensure that the baby receives adequate feed and/or IV fluids;
- Measure temperature every three hours;
- Treat the underlying condition;
- DO NOT GIVE ANTIPYRETICS TO NEONATES;
- Do not tepid sponge unless temperature is above 39o C. In this case use water that is 2 degrees below body temperature.
Fluid and Feed Management
If a baby is over 1,500g assist the mother to try breast or cup feeding every 2 to 3 hours. If the infant can breastfeed check the position and attachment of the baby to the breast. Other measures include the following:
- If unable to breastfeed pass a nasogastric tube and give expressed breastmilk every 2 or 3 hours depending on the weight of baby. Show the mother how to express milk;
- Ensure adequate intake by calculating the requirement per day;
- If not able to tolerate enteral feed give fluids IV.
Record all intake (oral and IV) and check every 6 hrs to see if the desired intake is achieved.
The other supportive care that infants with LBW may need is oxygen therapy.
Oxygen Therapy
Respiratory distress is fairly common in very immature babies, especially infants with very low birth weight (VLBW) and those with a gestation of less than 32 weeks. It is mainly due to lung immaturity but may also be caused by infection or aspiration. These infants therefore need oxygen therapy as follows:
- Give oxygen via nasal prongs or catheter is preferred;
- Give oxygen when there is severe respiratory distress, or recurrent apnoea;
- Discontinue as soon as normal breathing is restored;
- Remember that VLBW and to a less extent other LBW babies can get eye and lung damage from too much oxygen.
Prevent Infection
Infants have very low resistance to infection, particularly those who have low birth weight. Infection is a major of death among infants but it is preventable. Infections largely arise from hospital with bacteria that would not normally harm a normal full-term baby. The prevention of infections in these small babies depends upon the quality and amount of care given by first the mother, then the health care worker. We can prevent infection by observing the following measures:
- Hand washing between handling babies;
- Using clean/sterile equipment;
- Giving breast milk as it provides the baby with the kind of antibodies he or she needs to fight infection;
- Allowing the mother to take care of the baby herself as much as possible to reduce spread of infection from one baby to another;
- Supervising, advising and supporting mothers to take care to isolate LBW infants from other babies, especially those who with an infection;
- Keeping the environment clean;
- Avoiding overcrowding;
- Detecting, diagnosing and treating early infection.
Information and Counselling of The Mother - Points To Remember:
It is very important to keep the mother informed of what is going on with the baby at all times. This is because you will depend on her for a history of neonatal events later on in childhood. Ask the mother about her condition as well and if she has any problem treat or refer her for treatment. You should inform the mother and counsel her about the following:
- The infants birth weight;
- The condition of the infant at birth;
- Neonatal problems including all the procedures done, diagnosis and treatment that you have undertaken;
- Counsel her about the importance of breastfeeding the baby;
- Discuss with her future expectations of the infant and if they is any need for special follow-up;
- Ensure the child has been given all the necessary immunisation;
- Prepare a good discharge summary and tell mother when to return.
SUMMARY
In this Unit you we have covered some aspect of care of the newborn. We have concentrated on the common causes of morbidity and mortality among the newborns. I hope that you now feel confident to recognise a sick neonate, manage and institute the correct care. Remember, if any baby is not doing well, presume infection and take the appropriate steps to contain it before it is too late.
You can now take a break before you proceed to do the attached assignments.
Good Luck!
PRACTICAL ASSIGNMENT
Visit a labour ward or a newborn nursery and learn the following:
- Resuscitation of a newborn
- Passing a nasogastric tube and feeding
- Calculate feeds or IV fluid
- Learn about kangaroo mother care
- How to design a feeding and observation chart
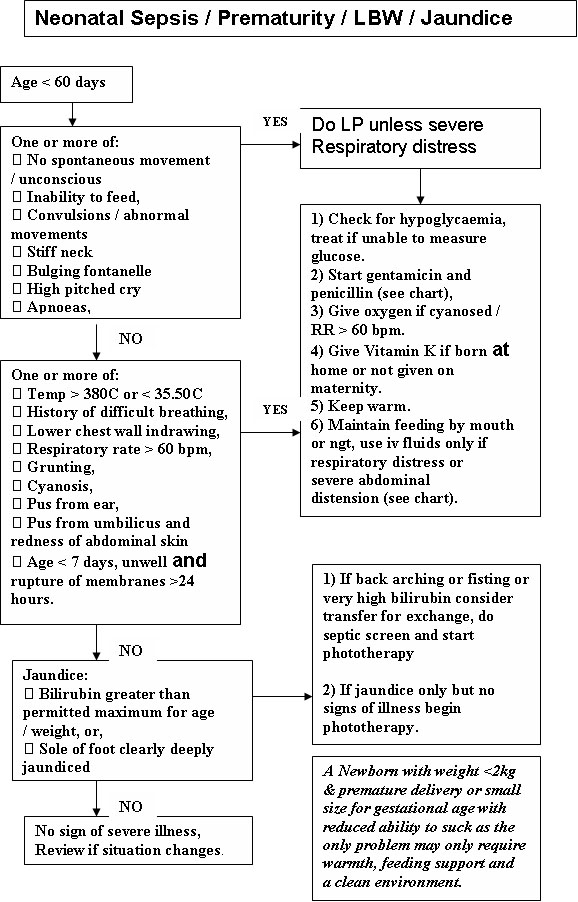
The following flow charts will help you in your practical assignment. Study them carefully as you practice in the clinical areas.
Figure 4.3: Neonatal Sepsis/Prematurity/LBW/Jaundice
|
DIRECTORATE OF LEARNING SYSTEMS DISTANCE EDUCATION COURSES
Student Number: ________________________________ Name: _________________________________________ Address: _______________________________________ _______________________________________________
Unit 4 Assignment Common Health Problems of the Newborn
1. A mother brings her 5 hour old premature baby to a health facility. She delivered herself in the night and the baby has refused to feed. a. Describe how you would assess this baby. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ b. What is your immediate management of this baby? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ 2. A 2 day old baby was born at term and weighed 3600g in a private clinic. Mother was not given any information but she says the delivery was difficult. Despite this she was discharged within hours of delivery. a. What further information would suggest birth asphyxia? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ b. What signs would suggest serious bacteria infection? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ 3. What factors would help you to determine the severity of jaundice. What modalities of treatment are available? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ Congratulations! You have come to the end of this unit. You can post or bring this assignment in person to AMREF Training Centre. We will mark it and return it to you with comments. Remember to quote your student number in the space provided.
|
Our address is as follows:
Directorate of Learning Systems
AMREF Headquarters
P O Box 27691-00506
Nairobi, Kenya
Email: amreftraining@amrefhq.org