Lesson 21: Other Conditions
Contents
INTRODUCTION
Congratulations for coming this far! You are now in the last unit of this course on child health. In the last two units, you learnt how to diagnose, manage and rehabilitate children with various types of disabilities. In this unit, you will learn about other conditions which affect children. Although these conditions are not very common, they have serious consequences on the health, normal growth and development of the children. These other conditions are:
- Bacterial meningitis
- Urinary tract infection
- Diabetes mellitus
- Typhoid
- Osteomyletis
- Septic arthritis
- Acute rheumatic fever
- Nephrotic syndrome
- Viral hepatitis
If these conditions are not recognized early and treated promptly, they can cause very high mortalities or serious complications in those who survive. That is why you need to equip yourself with the necessary knowledge and skills so that you can effectively contribute towards the reduction of deaths and complications associated with these conditions. Unfortunately, as you will discover, some of the above conditions do not have a cure. However, they can be prevented. And as you know, prevention is better than cure! So it is worth learning how to recognize all these conditions.
|
By the end of this unit you should be able to:
|
21.1 BACTERIAL MENINGITIS
What is Bacterial Meningitis?
|
Bacterial meningitis is the infection of the meninges, the membranes enclosing the brain and the spinal cord, by bacteria. Bacterial meningitis is among the most common and the most important causes of disturbed consciousness and coma in children. If meningitis is not recognized early and promptly treated, it is associated with high morbidity and mortality. |
Before you proceed do the following activity. It should take you 5 minutes to complete.
| 1
Think of the ways by which the bacteria reach the meningitis and write them down: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now read through the following discussion and see if your answers were correct.
Bacteria reach the meninges through the following ways:
- through the blood from such sites as lobar pneumonia, otitis media, septic arthritis bowel infection, and urinary tract infection;
- through direct spread from infected ear, mastoid or sinuses;
- through congenital or traumatic defects of the skull;
- through neurosurgical shunts.
Causes
The causes of bacterial meningitis are different in different ages.
- In the newborn, the causes of bacterial meningitis are:
- E. coli
- Group B beta streptococcus
- Listeria monocytogenes
- Staphylococcus aureus.
- In older children, the causes of bacterial meningitis are:
- Pneumococcus,
- Meningococcal,
- Haemophilus influenzae
- Mycobacterium tuberculosis.
Children with sickle cell disease, nephritic syndrome, and those who have had the spleen removed are likely to suffer from severe pneumococcal infection.
Clinical Manifestations
A child with meningitis presents with the following symptoms:
- fever,
- vomiting,
- inability to breastfeed or drink,
- headache or pain in the back of the neck,
- convulsions,
- irritability.
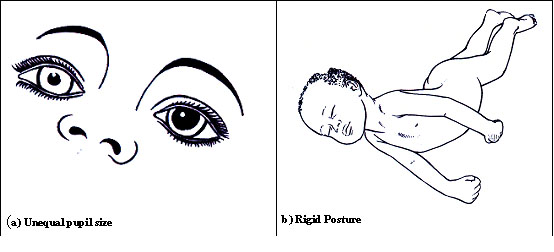
The signs of meningitis are as follows:
- stiff neck which may be absent or appear late in infants,
- repeated convulsions,
- lethargy,
- irritability,
- bulging anterior fontanels,
- petechial rash or purpura,
- a recent head trauma,
- unequal pupil size,
- rigid posture and opisthonos,
- focal paralysis in any limb and
- irregular breathing.
These last four signs show that the intracranial pressure is raised. Meningism means occurrence of neck stiffness without cerebrospinal fluid changes. Meningism is often seen in children with pneumonia, tonsillitis, retropharyngeal abscess, and severe otitis media and less commonly in children with hepatitis and urinary tract infection.
Figure. 21.1 Signs of meningitis
Investigations
When there are no signs of raised intracranial pressure, a lumbar puncture is done to obtain cerebrospinal fluid. A cloudy cerebrospinal fluid suggests meningitis. Microscopy shows more than 1000 leukocytes / mm3. Biochemistry shows more than 100mg of protein per deciliter. The glucose is less than 40% of the blood sugar which should be measured simultaneously. The culture of the cerebrospinal fluid shows the type of bacteria causing the meningitis.
Management
A child with meningitis should be urgently referred to the hospital. In the hospital, meningitis is treated with chloramphenicol 25 mg/kg intramuscularly or intravenously every 6 hours and benzyl penicillin 100,000/kg units intramuscularly or intravenously every 6 hours for a total duration of 10 days.
Complications
Complication of meningitis include the following:
- cerebral edema,
- hydrocephalus,
- brain abscess,
- hypoglycemia,
- deafness,
- blindness,
- convulsions,
- subdural effusion,
- subdural empyema,
- mental retardation,
- cerebral palsy and
- syndrome of inappropriate ADH secretion.
The syndrome of inappropriate ADH secretion is characterized by hyponatremia, low level of sodium in the blood, with water intoxication (excess water). This syndrome presents with restlessness, irritability, and convulsions. The treatment of a child with this syndrome consists of water restriction.
Prevention
Remember that early diagnosis and treatment of this condition is very important to avoid complications. Such complications as deafness and blindness interfere with the growth and development of a child. You should also give health education on the dangers of sleeping in crowded, badly ventilated houses to reduce the transmission of meningitis. Remember to emphasize the importance of early reporting and treatment. The Haemophilia influenzae meningitis is prevented by giving haemophilus influenzae vaccine to all children during immunization. Also, the pneumococcal and meningococcal vaccines are also available but are not yet being given routinely. You should report all cases of meningococcal meningitis to the district medical officer of health.
2: URINARY TRACT INFECTION
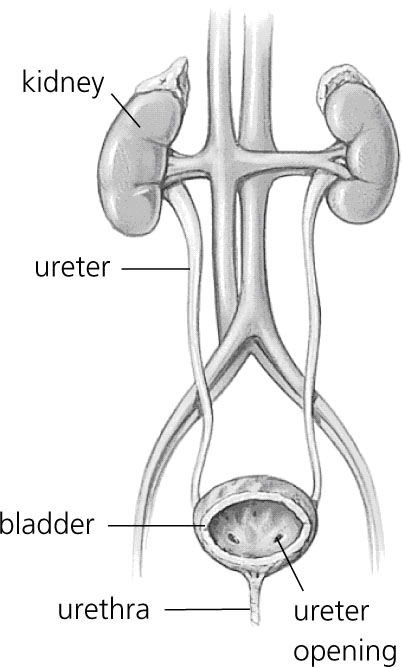
Urinary tract infection is the bacterial infection of the whole urinary tract from the urethra to the kidney. The infection of the urethra is called urethritis. The infection of the bladder is called cystitis. The infection of the pelvis and the kidney is called pyelonephritis. See these parts in Figure 2 below. Untreated, urinary tract infection may cause renal destruction and death. Urinary tract infection is often present in children with protein energy malnutrition
Figure 21.2: Structure of the urinary tract system
Causes
Urinary tract infection is caused by bacteria from the intestines and from the blood. The bacteria from the intestines include: E. coli, klebsiella, proteus, pseudomonas, enterococci and staphylococci. These bacteria ascend the urethra from the area surrounding the anus. The bacteria carried in the blood may lodge in the kidneys and then descend down the urinary tract.
Epidemiology
Urinary tract infection is common in the newborn period and early childhood.
Predisposing Conditions
- Obstruction of the urethra causes incomplete or infrequent emptying of the bladder. The incomplete or infrequent emptying of the bladder allows multiplication of bacteria;
- Vesicoureteral reflux, backflow of the urine from the bladder into the ureter, allows the bacteria to ascend the ureter and cause pyelitis and nephritis;
- Intrarenal reflux allows infection of the kidney. Each kidney infection leads to kidney destruction and formation of a scar. Extensive scarring from repeated kidney infections leads to chronic renal failure;
- Kidney or bladder stones facilitate the development of urinary tract infection;
- Congenital malformations such as hydronephrosis also facilitate the establishment of urinary tract infection. (Hydronephrosis is dilatation of the ureter and the pelvis with subsequent renal damage).
| 2
List the symptoms and signs of urinary tract infection: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Clinical Manifestations
In infants, urinary tract infection may manifest with the following symptoms:
- lethargy;
- refusal to feed;
- poor colour;
- apnoea;
- jaundice;
- anaemia;
- purpura and hepatosplenomegaly.
In young children, urinary tract infection manifests with non-specific signs such as:
- fever;
- vomiting;
- diarrhoea,
- abdominal pain;
- convulsions;
- poor appetite;
- irritability;
- jaundice and
- failure to thrive.
In older children, urinary tract infection presents with the following:
- passing urine more frequently than usual;
- pain while passing urine;
- acute retention of urine because of very severe pain;
- suprapubic pain or tenderness suggesting bladder infection;
- high fever;
- pain or tenderness in the flanks suggesting a kidney infection;
- cloudy smelly urine;
- haematuria and
- incontinence in a previously continent child.
Urinary tract infection may also be asymptomatic especially in infants and young children.
Investigations
Clean urine microscopy and culture where possible. In infants and young children, the urine specimen is collected by suprapubic aspiration or catheterization in older children, the urine specimen is obtained by clean catch of mid-stream urine. Urine specimens collected by plastic bags are inadequate and may give false results.
Diagnosis:
The diagnostic urine examination findings are:
- pus cells in the urine (more than 5-10 cells per high power field)
- growth of more than 105 colonies per ml of urine.
Complications:
The complications of urinary tract infection include septicaemia in newborns and young children and permanent renal damage
Management:
Urinary tract infection is treated with antibiotics for 5-7 days to eradicate the infection. The recommended antibiotics are cotrimoxazole, nalidixic acid, nitrofurantoin, and ampicillin.
Urinary tract ultrasound, micturition cystourethrogram are done to detect any vesocourethral reflux and obstructive abnormalities. Any anatomic abnormalities found are treated surgically.
Vesicourethral reflux is initially managed with continuous prophylactic antibiotics while periodically assessing the upper urinary tracts with ultrasound. The prophylaxis with antibiotics is only possible if there is compliance, regular system of follow-up and possibility of doing urine culture regularly for detecting infection. Successful prophylaxis with antibiotics is indicated by the child’s remaining free of urinary tract infections, absence of new renal scars and spontaneous resolution of the vesicoureteral reflux.
Development of urinary tract infection despite the prophylaxis with antibiotics, occurrence of new renal scarring, failure of the vesicoureteral reflux to resolve, non-compliance, allergic reaction, or side effects of the antiobiotics are the indications for surgical intervention to treat the vesicoureteral reflux.
Besides giving the antibiotics, the mother of a child with a urinary tract infection is advised to increase the child’s fluid intake. The child should be asked to pass urine frequently and to ensure that she or he completely empties the bladder. When possible, a urine culture should be done 48 hours after starting the antibiotics and one week after stopping the antibiotics. Even if no abnormalities are found, several follow-up urine examinations and culture are done for one year where possible.
3: DIABETES MELLITUS
Before you read on do the following activity, it should take you 5 minutes to complete.
| 3
What is diabetes? Write down your definition in the space provided below. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now read through the text below and see if your ideas are included.
Diabetes mellitus is a metabolic syndrome characterized by passing urine frequently, drinking frequently, eating many times, dehydration, weight loss, excessive blood sugar, and passage of sugar in the urine. An individual with diabetes is unable to use sugar normally. This explains why diabetes mellitus is also called sugar disease.
Causes There two types of diabetes mellitus: type I and type II diabetes mellitus.
(i)Type I diabetes mellitus
This the most common endocrine disorder of childhood and adolescence. Type I diabetes mellitus results from decreased secretion of insulin. The decreased secretion of insulin is due to progressive destruction of beta pancreatic cells by autoimmune mechanisms. Genetic factors and environmental factors also play a role in causing diabetes mellitus type I. The role of the genetic factors is supported by the occurrence of diabetes in family members. The environmental factors include viruses which may trigger the autoimmune destruction of beta pancreatic cells. There is a lifelong dependence on injected insulin to prevent complications of diabetes. Diabetes starts when about 85% of the beta pancreatic cells no longer secret insulin. The lack of insulin leads to failure of uptake of glucose into the muscle and adipose tissue. The glucose accumulates in the blood giving rise to hyperglycaemia (high blood sugar). Hyperglycaemia is worsened by utilization of proteins and formation of more new glucose. The hyperglycaemia leads to glycosuria (passage of sugar in the urine). Glycosuria is associated with excessive loss of fluids with frequent passage of urine. The loss of fluids leads to thirst. The thirst leads the child to drink a lot. Dehydration may occur if the fluid intake is inadequate. The lack of insulin also leads to increased oxidation of fat to provide energy with resultant abnormal increase in acetyl coenzyme A. The body uses the excessive acetyl coenzyme A to produce the ketone bodies. Excessive production of ketone bodies leads to the life threatening ketoacidosis, accumulation of ketone bodies in the blood, and ketonuria (passage of ketones in the urine). Ketoacidosis is life a threatening condition because of profound disturbances of the body functioning which leads to a gradually deepening coma which may cause death if not treated promptly.
(ii) Type II diabetes mellitus
This is caused by:
- the resistance of the skeletal muscle, liver, and adipose tissue to insulin;
- variable degrees of beta pancreatic cell impairment.
Type II diabetes mellitus is most common in the obese individuals. Ketoacidosis may develop during severe infections or other stresses. Then the patient may need insulin to correct hyperglycaemia
Symptoms:
The symptoms of diabetes mellitus are: polyuria, polidipsia, polyphagia and weight loss. Bed wetting in a previously toilet trained child may reveal polyuria. Ketoacidosis presents with vomiting, dehydration, deep sighing respiration, anxious appearance, abdominal pains and coma
Investigations:
- Determination of blood sugar
- Determination of urea and electrolytes
- Determination of serum phosphate
- Determination of acid base status
- Testing urine for sugar and ketones.
Diagnosis:
The diagnosis is based on clinical features, fasting blood sugar of 10 mmol/l and glycosuria (loss of glucose in the urine).
Management:
A diabetic child without ketoacidosis.
A diabetic child who is able to feed without vomiting is managed with rapidly acting insulin (regular, insulin lispro, humalog) administered subcutaneously at a dose of 0.1 to 0.25 unit/kg every 6-8 hours before meals with simultaneous blood sugar measurement and adjustment of insulin dose. A period of 1-2 days is needed to estimate the total daily insulin requirements for guiding use of combined intermediate and short acting insulins as discussed in the following section.
Ketoacidosis with dehydration.
The treatment of ketoacidosis with dehydration involves correcting the fluid and electrolyte disorder, alkali therapy, initiation of insulin and nutrition. Let us briefly look at each in turn.
i) Fluid and electrolyte.
Giving intravenous normal saline, assuming a10% dehydration, replacing 50 to 60% of the calculated volume in the first 12 hours and the remaining 40-50% in the next 24 hours. Adding potassium supplements to the normal saline after the first 20 ml of normal saline /kg so as to give 3-5mmol of potassium /kg/24 hours.
Oral fluids (sugar free fluids and milk) are introduced as soon as the child becomes conscious and stops vomiting.
ii) Alkali therapy.
If pH is 7.2 or less, partially correct the acidosis with sodium bicarbonate 40mmol/m2 at pH 7.1-7.2 and 80 mmol/m2at pH less than 7.1 over a period of 2 hours
iii) Initiation of insulin.
Insulin can be administered either as a continuous intravenous infusion (the best) or intermittently through intravenous, intramuscular or subcutaneous routes.
In continuous intravenous infusion of insulin, a priming dose of insulin is given intravenously or intramuscularly at a dose of 0.1 unit/kg followed by a constant infusion of 0.1unit/ kg hourly until ketoacidosis is corrected. If ketoacidosis is not corrected in 24 hours, you should look for sepsis and treat it and then continue the insulin infusion.
The treatment must be monitored by careful fluid balance, hourly blood sugar and two hourly electrolyte acid status measurements.
When the acidosis is corrected, insulin infusion is discontinued. Subcutaneous insulin, 0.2-0.4 units/kg is immediately given while maintaining the 5% dextrose until the child can fully tolerate food. When the child can tolerate food, insulin 0.2- 0.4 units/ kg is given before meals every 6-8 hours when the child starts eating. Measure the blood sugar before and 2 hours after the meal. Adjust the insulin dose to maintain a blood sugar of 4.4 - 10 mmol/l.
Table 1: Intermittent administration of insulin.
| Blood glucose | Total insulin dose | Intravenous | Intramuscular or
Subcutaneous |
Frequency |
|---|---|---|---|---|
| 33mmol/l | 1 u/kg | 0.5 /kg | 0.5u/kg | 2- 4 hours |
| 17-33mmol/l | 0.5u/kg | 0.25u/ kg | 0.25/kg | 2- 4 hours |
Intermittent doses of insulin for diabetic ketoacidosis.
Intravenous, intramuscular or subcutaneous bolus injections of insulin may also be given in the treatment of ketoacidosis. (See Table 1 on intermittent insulin doses for diabetic ketoacidosis). Hourly blood sugar and 2hourly electrolyte and acid status are measured just as in the case of intravenous insulin infusion. When the blood sugar falls to nearly 17 mmo/l, insulin 0.2 -0.4 u/kg may be given subcutaneously every 6-8 hours while maintaining a 5% dextrose infusion in 0.2N saline with potassium added until the acidosis is corrected and the child can tolerate solid foods. Sips of clear fluid, broth or carbonated drinks may be given in the interval. The subcutaneous insulin dosages of 0.2-0-4 u/kg every 6-8 hours should be continued for 24 hours after the child is eating. Then you should make a switch to combined intermediate and short acting insulin.
After recovery from ketoacidosis, the daily insulin requirement should be estimated as 2/3 of the total daily dose of regular insulin administered before each meal. This dose is about 0.5 units/ kg. Both intermediate and rapid acting insulin are combined differently depending on whether the regime adopted is one daily injection or two daily injections.
With a single daily dose of the combined regimen, 2/3 of the dose is made of intermediate and the remainder is regular insulin. The injection is given ½ hour before breakfast or with breakfast if Lispro is the short acting insulin. Step increases or decreases of 10- 15% of the daily dose are made till the desired degree of control is reached. The increases or decreases are made on the basis of the blood sugar before each meal or urine glucose or both as follows:
- If hyperglycaemia is observed in the late morning, the dose of regular is increased by 10-15%.
- If hyperglycaemia is observed late in the afternoon or in the evening, the dose of intermediate insulin is increased by 10-15 %.
- Should hypoglycaemia occur late in the morning, the dose of regular is reduced by 10.15%.
- If the hypoglycaemia is noted late in the afternoon or in the evening, the daily dose of intermediate insulin is reduced by 10-15 %.
With a two daily injections regime, intermediate and regular insulin are combined in the ratio 2:1 to 3:1. Each injection consists of intermediate and short acting insulin in proportions 2: 1 -3:1. Two thirds of the total daily dose is given before breakfast and one third before supper. The two daily insulin injections regime is recommended for treating young children and adolescents. The optimum regimen is one intermediate combined with regular before breakfast and then regular insulin before each meal. Rapid acting insulin acts in half an hour, reaches a maximum in two hours, and has negligible effect in 6 hours. Intermediate insulin has a significant effect after 6 hours, has maximum effect in 8 hours and negligible residual effect after 16 hours.
iv) Nutrition
The nutritional requirements of a diabetic child are the same as those of a normal child. Therefore, the diet of a diabetic child is not special but a healthy eating plan that should be followed by the whole family. Partaking of the diet by the whole family would prevent the child from feeling different from the rest of the family. The diet must be balanced and adequate for normal growth, development and activities. A balanced diet is that which contains the right amounts of carbohydrates, fats, proteins, vitamins and minerals. Ideally, the child should be given three main meals (breakfast, lunch and supper and three snacks (midmorning, midafternoon and bedtime) per day. These meals and snacks (fruit, fruit juice, or cracker) must be given at fixed times with evenly spaced intervals each day. When the carbohydrates are so evenly distributed, the movement of glucose is more or less predictable.
The caloric mixture should consist of 55% carbohydrates, 30 % fats and 15 % proteins. About 70 % of the carbohydrate content should consist of complex carbohydrates (bran, oatmeal, whole cereals, legumes, root crops boiled or baked in their skins). These foods are also rich in fibre. The fibre in these foods slows down digestion and absorption of the complex sugars. Therefore, the blood sugar rises more slowly after a meal. Foods rich in fibre are, therefore, recommended as staple components of the diet because they help in the control of blood sugar levels. High dietary fibre may also helps in the control of the blood cholesterol levels. Other foods with a high fibre content are leafy green vegetables and fruits. Excesses of carbohydrates are to be discouraged. Again, ideally, the parent should select the carbohydrates in such way that the amount carbohydrate in each meal or snack is known. The daily carbohydrate intake can be estimated using the formular:
Daily carbohydrate intake in grams= 100 + 10 a, where a is age in years. When the amount of sugar in a meal is known, it is possible to match the dose of the insulin to the food taken. A unit of insulin should be administered for every 10 to 15 grams of glucose.
Table sugar and highly refined sugars, including those contained in sodas and sweets should be limited. The glucose in refined sugars is absorbed rapidly. Such a rapid absorption of glucose causes wide swings in blood sugar.
The diet must be low in animal fats which are rich in saturated fatty acids. Animal fats are avoided and replaced by vegetable oils which are rich in unsaturated fatty acids. Butter and whole milk are discouraged. Whole milk is replaced by skimmed milk.
Protein, especially animal protein, is usually limited by cost. Ideally, poultry, veal, lean meat, fish and dried beans, good sources of proteins, are recommended as substitutes for red meat for keeping saturated fat low. Visible fat is removed from the lean meat. Fatty meats such as bacon are avoided. The number of egg yolks eaten is also limited. All these measures reduce the cholesterol which predisposes to artherosclerosis in adulthood.
The total daily calories should be distributed as follows:
- Breakfast 20 %
- Lunch 20%
- Supper 30 %
- Three snacks 30%
- Each snack provides 10 % of the total daily calories).
- Before an unusual activity, extra carbohydrates are given.
The regularity of food intake and constancy of carbohydrates intake is very mportant.
v) Parent education
It is important to teach the parents or caretaker on the following:
- how to monitor the blood sugar and urine ketones;
- how to prepare the injections;
- how to inject insulin subcutaneously 30-60 minutes before breakfast and supper;
- how to recognize and treat hypoglycaemia and maintain good hygiene.
Optimum control of diabetes requires combination of lente to provide background insulin and 4 daily injections of lispro or as part insulin analogues. These analogues act rapidly at each meal. The peak of the analogues is fast and there is little overlap and short tail effect. The parents should measure blood glucose before each meal (3 times a day).
Insulin induced hypoglycaemia presents with weakness, pallor, diplopia, sweating and twitching. The hypoglycaemia is treated with 1 mg of subcutaneous glucagon. Advice the parents to treat an impending hypoglycaemia with sugar, orange juice or sweetened beverages.
The children should be encouraged to engage in normal activities and their diet adjusted with extra carbohydrates to compensate for any unusual exercise. It is not the insulin which is adjusted to compensate for the unusual exercise. There are holiday camps for diabetic children organized by the Diabetics Association. Advice the parents to encourage the children to attend these camps.
The indicators of good control are:
- Normal growth and activity;
- Lack of polyuria;
- Lack of any severe hypoglycaemic episodes.
Management:
Patients with type II diabetes mellitus are given oral antidiabetics.
Complications:
Diabetic coma is a common complication of diabetes. You should urgently refer the child to a hospital. If the child has a hypoglycaemic coma, give glucose and then refer the patient
Next, let us look at another common condition, known as typhoid
4. TYPHOID
Typhoid fever is caused by Salmonella enterica, a highly virulent and invasive enteric pathogen traditionally referred to as Salmonella typhi. Only humans are affected, and most often, acquisition of S. typhi occurs via ingestion of food or water contaminated with excreta from carriers of the bacterium.
Cause
Typhoid is caused by Salmonellae. These are transmitted as follows:
- most commonly by ingestion of food or drink contaminated with the faeces of carriers or patients.
less commonly, by direct contact with the carriers or patients.
- transplacentally from the mother to the baby in case of congenital typhoid.
- during birth in case of intrapartum typhoid.
| 4
Think of circumstances that favor the spread of typhoid and write them down. _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ _____________________________________________________________ _____________________________________________________________
|
Now compare your answers with the following information.
Typhoid is common where:
- there are unsanitary conditions;
- the personal hygiene is poor;
- there is inadequate hygiene in food handling industries;
Manifestations
The incubation period of typhoid bacteria is 1-3 weeks, usually 2 weeks. The patient presents with high fever (except in the malnourished), malaise, headache, lack of appetite, abdominal pain, constipation, vomiting with or without diarrhoea, mental dullness, delirium and confusion, meningeal irritation signs, cough, sore throat, nose bleeding (epistaxis), respiratory distress (if pneumonia develops), muscle and joint pains, sometimes jaundice.
In infants and young children, typhoid may present with vomiting and bloody diarrhoea. Typhoid may also present as encephalopathy with meningism, delirium, convulsions and coma. Sometimes it may present as septicaemia with drowsiness, shock and jaundice.
Signs The signs of typhoid fever are mild abdominal distension, epistaxis, bradycardia, haemorrage which may cause shock, hepatosplenomegaly.
Complications
If typhoid is not well managed, it can lead to the following complications:
- Intestinal perforation;
- intestinal haemorrhage;
- convulsions in infants;
- myocarditis;
- arthritis;
- osteomylitis especially in sickle cell disease;
- meningitis;
- pneumonia;
- urinary tract infection;
- glomerulonephritis;
- acute tubular necrosis;
- haemolytic anaemia;
- hepatitis;
- abscesses.
Investigations
Once typhoid is suspected, the investigations carried out include:
- Widal test,
- Blood culture,
- Stool culture,
- rectal swab culture, urine culture,
- and cerebrospinal fluid culture.
Blood culture is usually positive early in the disease and rarely positive after two weeks of infection.
Diagnosis:
Diagnosis is based on rising Widal test titre and isolation of salmonellae from any of the above specimens.
Management:
You should start treatment immediately on suspicion after collecting the laboratory specimens. The mainstays of management are:
- Administration of antibiotics such as chloramphenicol 25mg/kg every 6 hours, given for 2-3 weeks. Other useful antibiotics are amoxycillin or cotrmoxazole;
- Maintenance of fluid and electrolyte balance;
- Isolation and barrier nursing;
- Providing nutritious diet;
- Surgery if bowel perforation occurs.
Prevention
Typhoid can be prevented with good sanitation and purification of water. You should advice the parents and caretakers to observe good personal hygiene and to cook food properly. Carriers should be identified, treated carriers and excluded from handling foods until the infection clears.
5. ACUTE OSTEOMYELITIS.
Acute osteomyelitis is the infection, usually bacterial, of the bone and the bone marrow. The infection usually occurs near the end of the long bones
Causes
The most common bacteria causing osteomyelitis is Staphylococcus . But streptococci, Haemophilus influenzae, pneumococci, and salmonellae may cause osteomyelitis. In the newborn, E.coli, pseudomonas, proteus and klebsiella may also cause osteomyelitis.
Osteomyelitis usually arises as a result of the spread of the bacteria through the blood from a clinically unapparent focus of infection. This focus may be:
- infected skin,
- A boil,
- dental abscess,
- a wound with a retained foreign body
It is important to search carefully and locate the focus. Direct spread of bacteria from a wound of a compound fracture may also result in osteomyelitis. Osteomyelitis occurs at any age but most commonly between the ages of 3-12 years.
| 5
Write down the symptoms and signs of osteomyelitis: ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________ ____________________________________________________________
|
I hope your answer included the following clinical manifestations of osteomylitis. In infants, the clinical manifestations of osteomyelitis may be non-specific. They include irritability, refusal to feed, not moving a hand, arm or leg (pseudoparalysis)
Older children may complain of fever, pain or limp.
The signs of osteomyelitis include:
- tenderness on pressure over the involved bone, usually at the metaphysis (end of the shaft),
- swelling over the subperiosteal abscess,
- redness,
- regional lymphadenitis,
- septic arthritis of the nearby joint or sympathetic effusion of the nearby joint.
Investigations:
The investigations done are blood culture, Gram staining of the needle aspirate of the abscess, full blood count and X-ray of the affected part.
Diagnosis
The diagnosis is based on the clinical findings, blood culture, and X-ray findings. Early in the illness, X-ray may shows only soft tissue swelling. Subperiosteal calcification becomes evident after 10 -14 days.
Treatment
Osteomyelitis is treated with:
- Intravenous flucloxacillin 50 mg/kg every 6 hours, or higher doses intramuscularly where intravenous drug cannot be given, for 1-2 weeks and continued orally for a total of 6 weeks;
- Rest;
- Paracetamol for relieving the pain;
- Elevation of the limb;
- Support in a partial plaster;
- Physiotherapy is offered in the recovery phase;
- Aspiration of the abscess or joint.
Complications
Osteomyelitis may be complicated by:
- Septic arthritis;
- Chronic osteomyelitis;
- Septic meningitis or epidural abscess;
- Pathological fractures;
- Lengthening and thickening of the limb with postural scogliosisi;
- Shortening with postural scogliosis;
- Flexion contractures.
- Arrest of growth of the limb
Differential Diagnosis
A number of conditions are considered in the differential diagnosis of osteomyelitis. These are:
- sickle cell disease,
- septic arthritis,
- cellulitis,
- local abscess,
- acute rheumatic fever,
- incomplete fracture,
- leukaemia,
- bone tumours and
- secondary metastasis.
Next let us learn about septic arthritis.
6. SEPTIC ARTHRITIS
Septic arthritis is infection of a joint by bacteria.
What Causes Septic Arthritis?
Septic arthritis is caused most commonly by Staphylococcus pyogenes. Other bacteria which cause septic arthritis are gonococcus, streptococci, haemophilus influenzae, pneumococci, meningococci, and salmonellae. The bacteria in the blood may reach a joint and cause septic arthritis. The bacteria may also reach the joint by direct extension from a neighbouring osteomyelitis. Direct extension through the epiphyseal centre is most likely to occur in infancy. This is because in infancy vessels from the metaphysis penetrate through the growth plate.
Clinical Manifestations:
Symptoms of septic arthritis include fever, irritability, and apprehension. The signs of septic arthritis are pallor, tachycardia, fluctuation, swelling, tenderness, redness (except the hip because it is hidden), limitation of movement, muscle spasm in a position of flexion and intense pain on movement.
Investigations
The investigations include obtaining a joint aspirate for culture and Gram staining, blood culture, and X-ray.
Diagnosis
Diagnosis is based on finding of bacteria on Gram staining of the aspirate, and isolation of the bacteria in the blood or joint aspirate cultures. Early in the infection X-ray shows soft tissue swelling and increased joint space. After 10-14 days, the X-ray shows osteoporosis, bone erosion and decrease of the joint space.
Management
Septic arthritis is managed with high intravenous antibiotics as in osteomyelitis for at least 4 weeks. If there is no improvement in 24 hours of starting the antibiotics, surgical decompression is done to prevent the destruction of the articular cartilage, necrosis of the epiphysis and dislocation which may cause permanent disability in the hip and shoulder. The other joints are decompressed with daily aspirations with large bore needle. Traction is applied to maintain good functional position. Physiotherapy is done to rebuild the muscle and regain mobility. Oral therapy is started when there is marked improvement
Complications.
A disabling ankylosis may occur in neglected cases.
7. RHEUMATIC FEVER
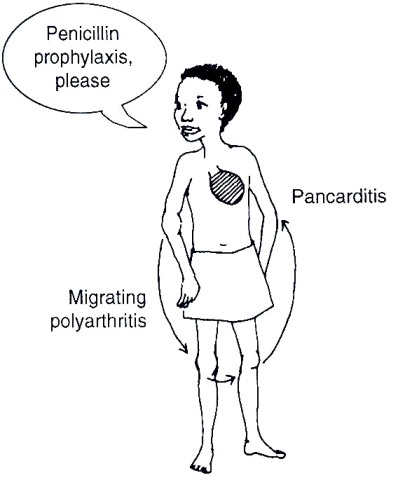
Rheumatic fever is a generalized inflammatory connective tissue disease characterized by fever, joint pains, and heart disease with less frequent involvement of the skin, nervous system and the subcutaneous tissues. Rheumatic fever has a tendency to recur and is due to an immune reaction following Group A beta haemolytic streptococcal throat infection.
Epidemiology
Rheumatic fever is common among the children of the poor, where there is overcrowding and delay in the treatment of throat infections. Rheumatic fever is extremely rare under 2 years of age. Most cases of rheumatic fever occur in children aged 5-15 years.
Cause
Acute rheumatic fever is related to a previous Group A beta haemolytic streptococcal throat infection. The interval between the throat infection and the attack of acute rheumatic fever varies from 4- 6 weeks.
Clinical Manifestations:
The clinical manifestations of rheumatic fever include:
- fever
- polyarthralgia (discomfort in the joints without objective evidence of pain, redness or swelling)
- migratory polyarthritis: this asymmetrical and involves the large joints (knees, ankles, elbow and the wrist). The affected joints are painful, red, hot, and swollen for about 24 hours. After the recovery of one group of joints, the attack moves on to other groups of joints. This movement of the attack from one group of joints to the other explains the description of the arthritis as migratory. The polyarthritis lasts 1-4 weeks and subsides without leaving any residual damage in the affected joints.
- Carditis: the most serious manifestation of rheumatic fever, involves all the layers of the heart wall simultaneously The inflammation of the pericardium (outer coating of the heart) is called pericarditis. The inflammation of the myocardium (heart muscle) is called myocarditis. The inflammation of the endocardium (internal lining of the heart wall) is called endocarditis. The involvement of the heart is revealed by the occurrence of new mitral and aortic murmurs and cardiomegaly. Very severe rheumatic heart disease may lead to heart failure. The heart lesions may remain and worsen with every recurrence of the acute rheumatic fever.
- Subcutaneous nodules: are several tender swellings 0.5-2cm in diameter. These nodules are found on the extensor surfaces of the bone prominences of the knees, elbows, shoulders, scapulae, the occiput and the spinal processes. The subcutaneous nodules occur in less than 15% of the cases and are indicators of a severe disease.
- Sydenham chorea: is characterized by jerky, involuntary and irregular movements of the limbs and face, emotional instability, inattentiveness, clumpsiness and crying out loudly. The movements are usually bilateral but may also be unilateral. The chorea is worsened by stress and disappears when the child is asleep. Sydenham chorea is rare and affects girls more commonly than boys. After several weeks or months, spontaneous remission occurs.
- Erythema marginatum: consists of non-pruritic macules or patches with central pallor and a well defined irregular margin on the trunk and the proximal parts of the limbs. Erythema marginatum occurs in 10 % of the cases of acute rheumatic fever.
The laboratory findings include acute phase reactants (leukocytosis, raised erythrocyte sedimentation rate, and elevated C-reactive protein), evidence of a preceding streptococcal infection (elevated or rising antistreptolysin titre, isolation of streptococci from throat swab culture, and positive streptozyme test) and prolonged PR interval in the Electrocardiogram (ECG).
In children aged < 2 years the clinical course of the disease tends to be mild and the correct diagnosis may often be missed in this age group.
Figure 21.3: Clinical features of rheumatic fever
Diagnosis.
No single clinical feature or laboratory test can establish the diagnosis of rheumatic fever. The diagnosis of rheumatic fever is made using some selected clinical features, the major and minor criteria published by Jones.
The five major criteria are:
- migratory polyarthritis;
- carditis;
- Sydenham chorea;
- Subcutaneous nodules; and
- erythema marginatum.
The minor criteria include:
- fever
- Polyarthralgia in the absence of polyarthritis as a major criterion;
- prolonged PR interval on the electrocardiogram
- Acute phase reactants (leukocytosis, raised erythrocyte sedimentation rate, and elevated C-reactive protein),
- evidence of a preceding streptococcal infection (elevated or rising antistreptolysin titre, isolation of streptococci from throat swab culture, and positive streptozyme test)
| 6
Write down the usage of the above criteria for making diagnosis of acute rheumatic fever: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
The diagnosis of rheumatic fever is based on the presence of two major criteria or one major criterion and two minor criteria, together with evidence of a preceding streptococcal infection
Investigations:
The investigations done on suspecting acute rheumatic fever are throat swab for culture, Antistreptolysin O titre (ASOT), and blood for acute phase reactants
Complications.
The development of rheumatic valvular heart disease is the major complication of acute rheumatic fever.
Treatment:
After taking the throat swab, the first intramuscular dose of benzyl penicillin is given. The intramuscular injections or oral penicillin are then continued for 10 days.
Children with painful joints and carditis often lie still. As they recover, they are not allowed to walk until the joint involvement has subsided, heart size diminished and rapid pulse diminished. Thereafter, the children are progressively allowed more activity. If there has been heart failure, the convalescence may be more prolonged and activity is restricted until the evidence of rheumatic activity has been absent for 2 weeks.
Anti-inflammatory treatment.
The anti-inflammatory treatment is effected with salicylates 100mg/kg/24 hours divided in 4 doses for 3-5 days followed by 75mg/kg/24 hours divided in 4 doses for 4-6 weeks. Patients with carditis or congestive cardiac failure are also given predisone, 2mg/kg/24 hours divided in 4 doses for 2-3 weeks. Thereafter, predisone is tapered over a period of 2 weeks by giving 5mg/24 hours every 2-3 days. While predisone is being withdrawn, salicylates are given. Mild rebounds after the discontinuation of the anti-inflammatory drugs are left alone. Those with severe rebounds are given salicylates or steroids once more.
Congestive cardiac failure is treated with digoxin, diuretics, fluid and salt restriction and oxygen. The slow digitilization dose of digoxin is 0.04 -0.06 mg/kg in 4 doses. The maintence digoxin dosage is 0.01 mg/kg in two divided doses. Furosemide 2 mg/kg intravenously per dose is given when there is pulmonary oedema.
Prevention of rheumatic fever.
a)Primary prevention.
Primary prevention means treatment of the streptococcal upper respiratory infection with antibiotics to prevent the first attack of rheumatic fever. Antibiotic therapy started up to the 9th day of the onset of symptoms of the upper respiratory infection can prevent rheumatic fever.
b)Secondary prevention.
Secondary prevention means prevention of infection of upper respiratory tract with group A beta haemolytic streptococci in persons who have had an attack of rheumatic fever. The preferred method of secondary prevention is regular monthly intramuscular injections of benzathine penicillin G, 1.200,000 units. Patients with rheumatic carditis need a lifelong secondary prophylaxis. The individuals with no carditis continue with secondary prophylaxis until early twenties provided that at least 5 years will have passed since the last attack of rheumatic fever. Before dental or surgical procedures, patients with rheumatic carditis also need additional antibiotics to prevent infective endocarditis. The secondary prophylaxis of rheumatic fever is not enough for preventing infective endocarditis. The additional antibiotics (gentamycin, amoxycillin, cephalexin, azithromycin or erythromycin) are given within half an hour before the procedure. I hope you now understand how to diagnose and treat rheumatic fever. Remember that it can be prevented by treating a sore throat early with antibiotics. So advice parents not to ignore a child with a sore throat but to bring them for treatment as early as possible.
Before you proceed to read the next section, do the following activity.
| 7
Write down the features of nephrotic syndrome: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
8. NEPHROTIC SYNDROME.
Nephrotic syndrome (NS) is a condition that is often caused by any of a group of diseases that damage the kidneys' filtering system, the glomeruli. The structure of the glomeruli prevents most protein from getting filtered through into the urine. Normally, a person loses less than 150 mg of protein in the urine in a 24-hour period. If a person has a urination of more than 3.5 grams of protein during a 24-hour period or passes 25 times the normal amount, then this indicates that they have nephritic syndrome.
The nephrotic syndrome frequency reaches a peak between 5 and 8 years.
Causes
In 90% of the cases, the cause of nephrotic syndrome is unknown, this type of nephrotic syndrome being called idiopathic nephrotic syndrome. In the remaining 10%, the nephrotic syndrome is secondary to acute glomerulonephritis, purpura, lupus erythematosus, drugs, hepatitis, acquired immunodeficiency syndrome, syphilis, quartan malaria, schistosomiasis hydatid disease, and diabetes mellitus. There is also a congenital form of nephrotic syndrome.
All types of nephrotic syndrome are characterized by increased permeability of the glomerular membrane to proteins. This increased permeability of the glomerular membrane to proteins leads to heavy loss of proteins in the urine. The protein loss is at a greater rate than the liver can produce the serum proteins. This imbalance between protein loss and the production leads to low levels of albumin in the blood. In turn, low albumin in the blood leads to oedema. The low levels of albumin in the blood stimulates generalized protein synthesis including lipoproteins, the carriers of the lipids in the blood. The increased synthesis of lipoproteins together with decreased breakdown of the lipid owing to reduced levels of plasma lipoprotein lipase, the enzyme that removes lipids from the plasma, account for the high level of lipids in the nephrotic syndrome .
Clinical Manifestations
A child with Nephrotic Syndrome has these signs:
- High levels of protein in the urine;
- Low levels of protein in the blood;
- Swelling resulting from buildup of salt and water
There is gradual appearance of oedema over a period of days or weeks. The oedema first appears in the face early in the morning and progresses to the feet later in the day. Other symptoms are loss of appetite, lethargy, passage of little urine (oliguria) and abdominal swelling and pain due to ascites. The signs of nephrotic syndrome are oedema, ascites, and pleural effusion.
Investigations
The investigations include determinations of serum protein, proteins in urine, serum cholesterol.
Diagnosis
Nephrotic syndrome is based on the clinical features and finding of gross proteinuria (40 mg /hr/m2)
Management
Patients with severe oedema, pleural effusion, ascites or genital oedema are hospitalized. Sodium intake is restricted until oedema resolves. If oedema is severe, fluid intake is also restricted. In some instances of severe oedema, 25% human albumin 1g/kg/ 24 hours is given intravenously. Predinisone is given at a dose of 60mg/m2 /24 hours divided in 3 or 4 doses. Usually after 2 weeks of predinisone administration, response to predinisone occurs. The response to predinisone is indicated by cessation of proteinuria. The nephrosis is steroid resistant if the child continues to have proteinuria after a month of treatment with predinisone.
After five days of protein free urine, the dosage of predinisone is reduced to 60 mg/m2 to a maximum of 60 mg every other day with breakfast. This alternate day regime of predinisone is continued for 3 – 6 months to maintain the remission. After such a period of alternate predinisone therapy, the drug may be stopped abruptly.
Relapses may occur. A relapse is recurrence of oedema and proteinuria and is treated as above. If repeated relapses occur, cyclophosphamide therapy is given.
Complications
The complications of nephrotic syndrome include:
- infections and pneumonia for immunoglobulin loss and increased catabolism;
- pulmonary embolism, arterial and venous thrombosis for hypercoagulability ;
- iron resistant microcytic anaemia for loss of transferring;
- rickets for loss of cholecalciferol binding protein.
The hypercoagulability, that is an increased tendency to form clots in the blood, is partly due to:
- loss of antithrombin III (an anticoagulant protein) in the urine;
- increased levels of fibrinogen in the blood;
- increased tendency of the platelet to collect into a mass (aggregability);
- and damaged ability to break down the fibrin (fibrinolysis), fibrin being the main component of the blood clot
Prognosis:
Many of the children with steroid sensitive idiopathic nephrotic syndrome have repeated relapses until recovery toward the end of the second decade of life. The recovery is indicated by passage of urine without proteins for at least 5 years. In the other types, full recovery does not occur and the disease progresses to end stage renal failure.
Prevention
There is no known way of preventing idiopathic nephrotic syndrome. However, secondary nephrotic syndrome can be prevented by:
- preventing the primary diseases: hepatitis, acquired immunodeficiency syndrome, syphilis, quartan malaria, schistosomiasis and hydatid disease;
- avoiding such drugs as captopril, troxidone and mercurial diuretics and penicillamine;
- Carefully controlling diabetes mellitus in childhood.
9. VIRAL HEPATITIS
Hepatitis is inflammation of the liver most commonly caused by the hepatitis viruses. These viruses are so called because of their special preference for the liver cells for multiplication.
Causes
As mentioned above, the hepatitis viruses are the commonest causes of hepatitis. The hepatitis viruses which have so far been identified include:
- hepatitis A virus (HAV)
- hepatitis B virus (HBV)
- hepatitis C virus (HCV)
- hepatitis D virus (HDV)
- hepatitis E virus (HEV)
- Hepatitis G virus (HGV)
Their commonly used abbreviations are indicated in brackets. As yet hepatitis F virus has not been identified. As I mentioned earlier, all the hepatitis viruses have a special liking for the liver cells. The disease caused by each of the hepatitis virus is called after that particular virus. Thus we speak of hepatitis A, hepatitis B etc. Other viruses, such as cytomegalovirus, Epstein-Barr virus, rubella virus and enteroviruses, may also cause hepatitis.
Let us look at each type of hepatitis in turn starting with Hepatitis A,
Hepatitis A
Hepatitis A is the infection of the liver by hepatitis A virus. Hepatitis occurs all over the world but most cases are found in the developing countries. Hepatitis A virus is most commonly transmitted by the faecal oral route. Rarely, hepatitis A virus is transmitted through the blood products or through the skin. The incubation period of hepatitis A averages 4 weeks with a range of 2 to 6 weeks. From the liver, the virus reaches the blood, bile and the stools. Maximum faecal excretion of hepatitis A virus occurs late in the incubation period with a minimum occurrence after the onset of the symptoms. Up to two thirds of all the cases are asymptomatic. Two thirds of the symptomatic cases are without jaundice.
Clinical manifestations
Fever, anorexia, nausea, vomiting, diarrhoea and headache may precede jaundice by one week. In infants and young children, these symptoms may also pass unnoticed. The symptoms are more likely to appear in older children. The jaundice is associated with liver enlargement and tenderness. The peak of the jaundice occurs one to two weeks after the onset and then begins to subside. Darkening of the urine may precede the jaundice. The stools may become light or clay coloured. Hepatitis A outbreak in the asymptomatic infants and young children is recognized when the symptoms appear in several children in a school.
Diagnosis:
A history of contact, detection of anti-HAV IgM (immunoglobulin M) antibodies, elevated aminotransferases especially the alanine aminotrasferase, and elevated conjugated and unconjugated bilirubin.
Complications
99 % of the children recover. In very rare occasions, fulminant hepatitis does occur. Aplastic anaemia is another rare complication.
Treatment
There are no specific measures. Light diet at the start of the illness is preferable. Low fat diet is offered during the period of jaundice.
Fulminant hepatitis has a very high fatality. The prognosis is particularly poor if coma with deepening of jaundice and ascites develop. Incomplete resolution leads to prolonged hepatitis or chronic cholestatic hepatitis but not cirrhosis. 6 to 10 weeks after resolution, benign relapses may occur for several months in 10% to 15% of the cases.
Prevention
Hepatitis A can be prevented through isolation of cases, careful hand washing, careful handling of the stools, diapers and other contaminated clothes. Isolation is necessary because the patient remains contagious for 7 days after the appearance of jaundice. An inactivated hepatitis A virus vaccine is available. But this vaccine can be administered only in children aged above 2 years of age.
B) Hepatitis B.
Hepatitis B is caused by hepatitis B virus. This virus possesses three antigens: hepatitis B surface antigen, hepatitis B core antigen, and hepatitis B e antigen. The abbreviations for these antigens are HBsAg, HBcAg and HBeAg respectively.
Epidemiology:
Hepatis B virus, too, has a world-wide distribution. But most cases are found in the developing countries. High concentrations of hepatitis B virus occur in the blood, serum, serous exudates, saliva, vaginal fluids, and semen. Hepatitis B virus is most commonly transmitted vertically from an infected mother to her baby before birth (intrauterine infection) or during labour and birth (perinatal infection). It can also be transmitted by blood, blood products or other body fluids through contact with contaminated needles, skin piercing, tattoos intravenous drug abuse, haemodialysis or through sexual contact. The lower the age at the time of infection is, the higher the risk of developing chronic HBV infection. Chronic infection is defined by being HBsAg positive for six months. Finding HBsAg in a patient is diagnostic and indicative of infectivity. Presence of HBe antigen indicates infectivity. On the other hand, the appearance of anti-HBs antibodies indicates recovery (termination of viral multiplication), non-infectivity and immunity. Hepatitis B virus is transmitted through the blood products or the skin. The incubation period of hepatitis B averages 4 months range of 2 to 6 months.
Symptoms
Hepatitis B presents with:
- Gastrointestinal upset, lethargy, and malaise;
- Jaundice in only 25% from the eighth week of exposure and lasting for 4 weeks;
- Liver enlargement and tenderness. Sometimes the liver is not palpable below the costal margin. Gentle striking of the rib cage with a closed fist over the liver may then elicit the liver tenderness;
- Splenomegaly and lymph nodes enlargement are common;
- Macular rash, maculopapular rash, urticarial lesions and arthritis may precede jaundice.
Diagnosis
The diagnosis of hepatitis B is based on the presence of HBs antigen in the blood, anti-HBc IgM antibodies together with elevated alanine and aspartate aminotransferases and bilirubin (both conjugated and unconjugated). Presence of HBs antigen alone signifies infection or a carrier state.
Treatment
A patient with hepatitis is given:
- Rest
- Nutritious diet,
- Alpha interferone 5-6 million units/m2 body surface area three times a day for 4 to 6 months is recommended.
Prognosis:
10 % of the cases develop chronic hepatitis. Chronic hepatitis B predisposes to cirrhosis and hepatocellular carcinoma more in adults than in children.
Prevention Hepatitis B is prevented by:
- Immunization with Hepatitis B vaccine.
- avoiding sharing of needles.
- Proper disposal of needles
- Screening of blood for Hepatitis B surface antigen
- Careful sterilization of instruments
- Wearing gloves during withdrawal of blood
c) Hepatitis C
Hepatitis C is the infection of the liver by hepatitis C virus. This virus has numerous subtypes and subspecies and is transmitted in the same way as the hepatitis B virus. In hepatitis C, seroconversion (change from a negative ELISA to a positive one) may take as long as 6 months to develop.
Clinical Manifestations
The clinical manifestations of hepatitis C are similar to those of other hepatitis viruses. There may be manifestations of small vessels vasculitis, cerebritis, membranoproliferative glomerulonephritis and peripheral neuropathy.
Diagnosis:
The diagnosis is based on detecting IgG antibodies. Recombinant immunoblot assay (RIBA) detects antibodies to multiple hepatitis C virus antigens. Polymerase chain reaction becomes positive in three days.
Treatment:
A combination of alpha interferone and ribavirin has been recommended.
Complications:
There is a low risk of developing fulminant hepatitis but there is a high risk of developing cirrhosis and hepatocellular carcinoma.
Prevention:
There is no vaccine available. To minimize further liver damage, the patients should be given hepatitis A and hepatitis B vaccines.
d) Hepatitis D.
Hepatitis D virus is the smallest animal virus. Because it is incomplete, HDV alone cannot multiply or cause an infection. To be able to multiply and cause infection, HDV must associate HBV. From the excess of hepatitis B surface antigen, HDV acquires an envelop. This explains why hepatitis D occurs only in subjects with hepatitis B. The HDV and HBV infections occur either simultaneously (coinfection) or the HDV infects a subject already having a chronic HBV infection (superinfection).
Epidemiology:
HDV is transmitted in the same ways as hepatitis B virus but the vertical transmission is rare. The incubation period of a coinfection of HDV and HBV is 90 days. The incubation period after superinfection HDV on HBV infection is 1-2 months
Clinical Manifestations:
The symptoms of hepatitis D resemble, but are more severe than, those of other hepatitis viruses. The coinfection is common and manifests as an acute infection that is more severe than hepatis B alone. The risk of coinfection resulting in fulminant hepatitis is 10%. However, there is a low risk of a patient with coinfection to develop chronic hepatitis.
In contrast, the risk of superinfection resulting in fulminant hepatitis is 20%. The superinfection may manifest with a severe chronic hepatitis that rapidly progresses to cirrhosis. The superinfection also leads to hepatocarcinoma at a younger age and at a higher rate than HBV infection alone.
Diagnosis
The diagnosis is based on the detection of anti-HDV IgM antibodies, HDV antigen and or HDV RNA by polymerase chain reaction.
Prevention
HDV infection is prevented through hepatitis B vaccine. This is because HDV only infects humans who are infected with HBV. HDV infection cannot be prevented in those already infected with HBV.
e) Hepatitis E.
HEV is transmitted through the faecal oral route. Hepatitis E virus may cause outbreaks associated with contamination of water supplies. Hepatitis E virus causes acute hepatitis primarily after the first decade of life. The incubation period is 2-6 weeks
Clinical manifestations
The clinical manifestations of hepatitis E are anorexia, nausea, vomiting, fever, pruritus, hepatomegaly and abdominal pain. These symptoms may persist for weeks before the jaundice appears. The acute infection resolves 1-6 weeks after the onset. Chronic disease does not occur.
Diagnosis:
The diagnosis is based on ELISA for detection of anti-HEV IgM antibodies.
Treatment and Prevention
No treatment is available and there is no vaccine available for its prevention.
f) HEPATITIS G
Hepatitis G virus was discovered recently. It is transmitted parenterally and is found more commonly in patients who have received blood products, clotting factors concentrates (that is, substances which are essential for coagulation of blood and which are missing in patients with bleeding disorders), haemodialysis or transplants. Hepatitis G is also spread through intravenous drug abuse, sexual contact and vertically from mother to child.
Symptoms
Infection with hepatitis G virus is mostly asymptomatic despite the very high level viremia. There is little evidence of direct hepatic involvement. It is not associated with fulminant or chronic liver disease.
Diagnosis:
The diagnosis of hepatitis G virus infection is based on the detection of HGV RNA by polymerase chain reaction.
Treatment:
No treatment is available.
Prevention:
No vaccine is available.
SUMMARY
In this unit, we have discussed several important common conditions that affect children. We have looked at Bacterial meningitis, Urinary tract infection, Diabetes mellitus, Typhoid, Osteomyletis, Septic arthritis, Acute rheumatic fever, Nephrotic syndrome, and Viral hepatitis. We hope you are now able to diagnose, manage and prevent these conditions as some of their complications are not only life threatening but can also cause lifelong disability, failure to thrive and hepatocellular carcinoma.
Congratulations! You have also come to the end of this course. We hope you are now well equipped to provide comprehensive and integrated health care services to the children in your catchment area.
Now take a short break and then complete the attached assignment.
|
DIRECTORATE OF LEARNING SYSTEMS DISTANCE EDUCATION COURSES
Student Number: ________________________________ Name: _________________________________________ Address: _______________________________________ _______________________________________________
Instructions: Answer all the questions in this assignment. 1 a) A one and a half old child is brought for excessive crying and refusal to feed. You examine him and find that he has a stiff neck. Outline how you would investigate and manage this child. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ b) List any five complications the child may get. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ 2. A child whose mother died recently of a disease characterized by a bloody cough is brought because of night sweats. Examination reveals wasting. Which 6 factors will you consider for establishing the diagnosis? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
3. a. A one year old boy has dribbling of urine from birth. What are the 5 likely complications of the above condition? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ 4. Match the terms in list A with the corresponding ones in list B by writing the letters a. b. etc in List B in the space provided in list A. List A i. Nephrotic syndrome ii. Osteomyelitis. iii.Urinary tract infection iv.Hepatitis B v.Delayed type hypersensitivity vi.Ketoacidosis vii.Typhoid fever viiiAcute rheumatic fever ix. Raised intracranial pressure x.Hyperlipidemia List B a. unequal pupil size b. serum lipase c. polyarthritis d intestinal perforation e. hepatitis A f lente insulin g. hepatocellular carcinoma h. vescicourethral reflux i. staphylococcus j.schistosomiasis k.primary complex l. glucagons m.hypoglycaemia
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Our address is as follows:
Directorate of Learning Systems
AMREF Headquarters
P O Box 27691-00506
Nairobi, Kenya
Email: amreftraining@amrefhq.org