Lesson 20: Disability and Rehabilitation Part 2
Contents
- 1 INTRODUCTION:
- 2 15.1 DEFINITION:
- 2.1 20.2: CAUSES OF CEREBRAL PALSY
- 2.2 20.3 EARLY SIGNS AND SYMPTOMS OF CEREBRAL PALSY
- 2.3 20.4 MANAGEMENT AND INTERVENTION
- 2.4 20.5 PREVENTION OF DEFORMITIES
- 2.5 20.6 FACILITATING DEVELOPMENT OF MILESTONES
- 2.6 20.7 SPEECH AND COMMUNICATION
- 2.7 20.8 COMMUNITY EDUCATION
- 2.8 20.9 PREVENTION
- 2.9 20.10 SUMMARY
- 3 Assignment
INTRODUCTION:
This section will discuss the disorder known as cerebral palsy. We will describe the disorder, its causes, the different types of cerebral palsy, as well as diagnosis and management.
|
By the end of this unit you should be able to:
|
15.1 DEFINITION:
According to the WHO cerebral palsy (CP) is a disorder of muscle control that leads to difficulty in movement, positioning of the body, and performance of motor skills
This disorder in muscle control is due to permanent, non-progressive damage to parts of an immature brain that occurs before or after birth, or during early childhood. Due to the damage, muscles receive wrong impulses relayed from that area of the brain. These impulses, in turn, stimulate abnormal muscle contractions. Under normal circumstances muscles either contract or relax in order to carry out a function synergically. But in cerebral palsy, the wrong impulses cause muscle incoordination due to inappropriate muscle tone.
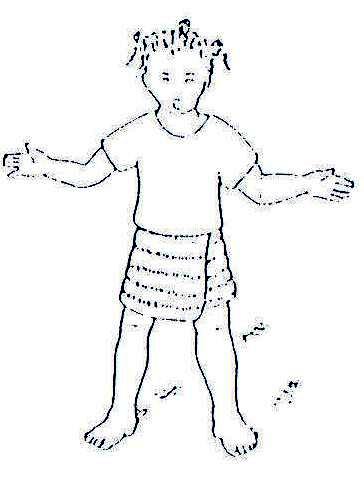
The muscles are either hypertonic (stiff) or flaccid (soft) and do not therefore have the desired tone for normal activity. This abnormal tone makes a child’s body become stiff or floppy. See Fig. 20.1 and Fig. 20.2.
.
Fig. 20.1: Muscles are Hypertonic (stiff)
.
Fig. 20.2: Muscles are Flaccid (soft)
These stiff or flaccid muscles hamper the performance of normal functions. Other parts of the brain which control vision or communication may also be affected, leading to difficulty in seeing, hearing, communication and learning.
Cerebral palsy is a permanent disability and affects each child differently. It is a major cause of developmental delay and physical disability.
Early intervention through rehabilitation exercises and training by physiotherapy and occupational therapy help to facilitate the developmental milestones in these children. Therefore, early intervention is necessary in order to reduce the disabling effects.
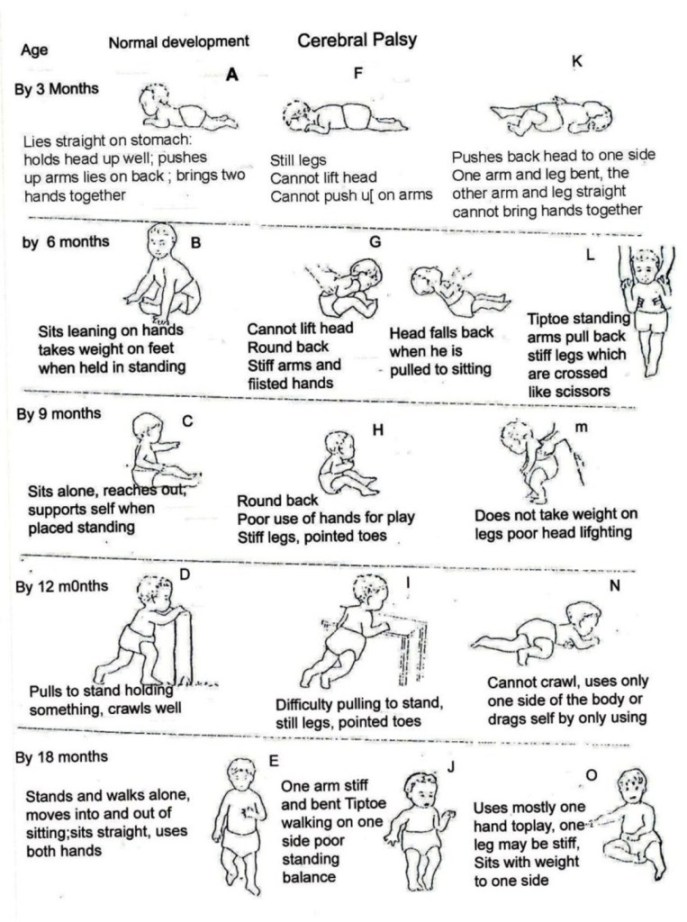
The attached development chart (Fig. 20.3) normal child development with the development of a child with cerebral palsy.
Types of Cerebral Palsy:
Different types of cerebral palsy are classified according to presentation:
- Spastic CP
- Ataxic CP
- Mixed CP
- Monoplegic CP
1. Spastic Cerebral Palsy:
This is the most common type of CP. Spastic is a condition of muscular rigidity or spasm that children with CP have. Muscle stiffness causes the body to adopt abnormal positions that the child cannot easily move out from. Movements are awkward and limited or restricted.
Muscle stiffness varies with the circumstances to which the child is exposed. It is worse when the child is either upset, exerting a lot of effort, moved quickly or roughly, or is subjected to sudden loud noise. Shifts in stiffness from one part of the body to another can also occur with changes in the head positions.
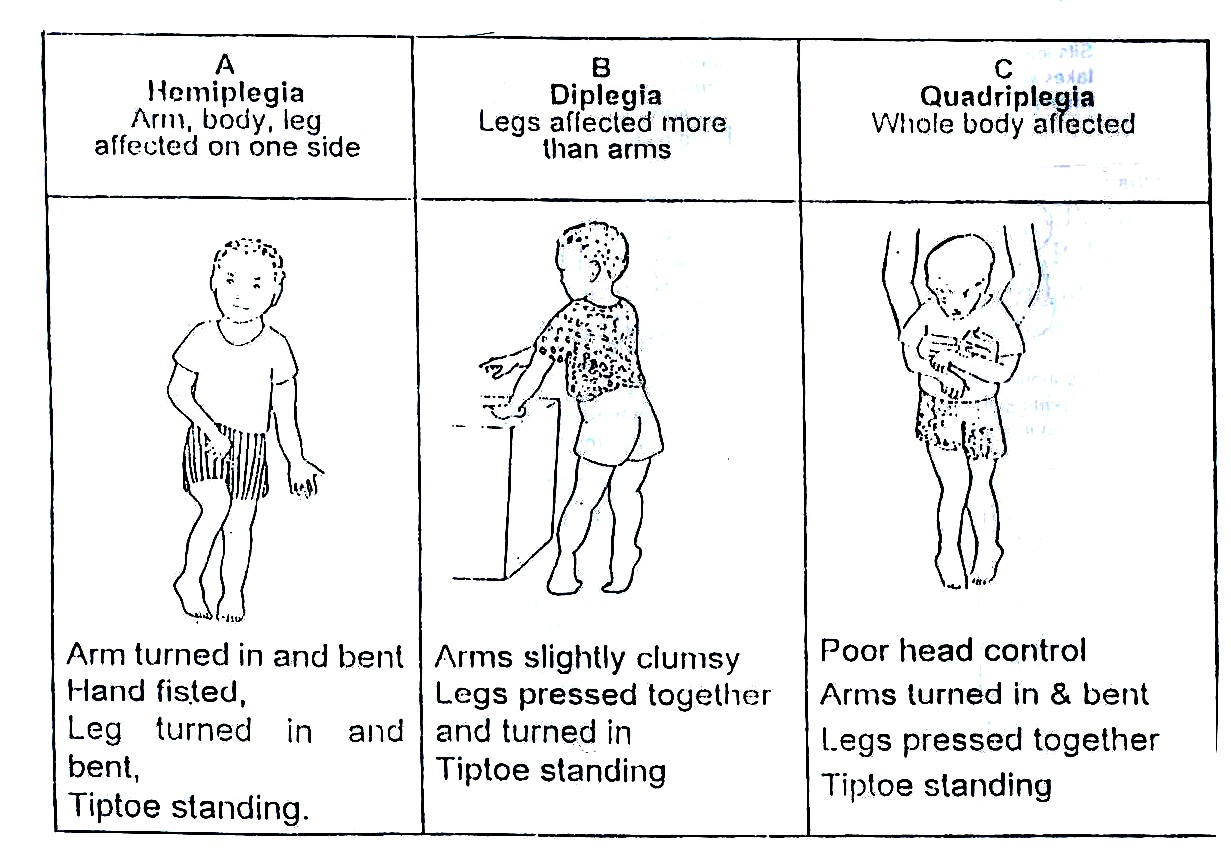
Spastic Cerebral Palsy is further classified according to which parts of a child’s body are affected, as explained later in this unit and shown in Fig. 20.4.
- Hemiplegia: In this type of CP, one half of the body is affected, such as an arm, leg and body (Fig.20.4A).
- Diplegia: Here, the legs are more affected than the arms (20.4B).
- Quadriplegia: In this type, the whole body is affected (Fig. 20.4C).
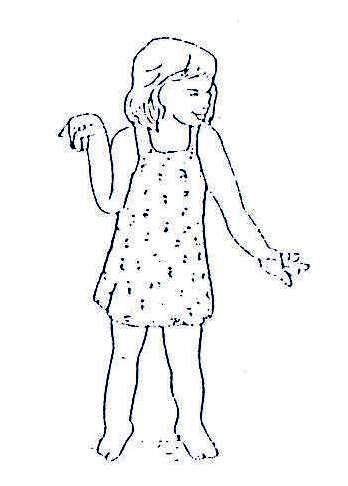
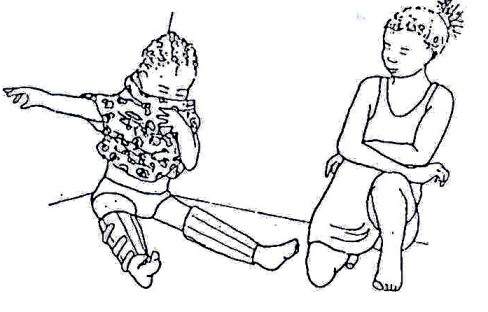
- Athetosis: Athetosis means uncontrolled purposeless movements. These may be jerky or slow wriggle movements of the child’s legs and arms, hands or face. These abnormal patterns of movements increase with excitement and are much less when he/she is calm (Fig. 20.5).
.
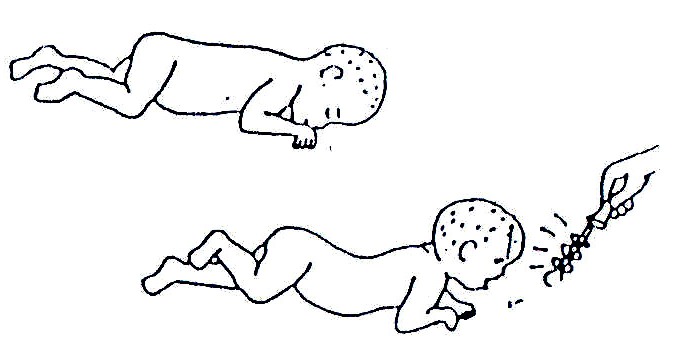
Fig. 20.3: The drawings on the left (A–E) show the way normal babies move at important stages of development. The drawings on the right show how the same movement might look when done by a child with cerebral palsy (To be sure that the child has cerebral palsy, see a doctor).
Muscle tone changes constantly from stiffness to floppiness resulting in abnormal posture or body positions. The constant change in muscle tone affects balance and the ability to speak clearly. See Fig. 20.5.
Children with athetosis are floppy or have soft muscles as babies but develop uncontrolled movements at two to three years. A few children may remain floppy for the rest of their life.
2. Ataxic CP: Ataxia means unsteady or shaky movements that are less pronounced than in athetosis. These unsteady movements are observed when a child tries to carry out an activity. For example, when he/she reaches for an object or a toy, he/she may miss the target in the first attempt. Due to poor balance, standing and walking may take longer to learn. See Fig. 20.6.
.
Fig. 20.4: Hemiplegia, Diplegia and Quadriplegia
3. Mixed Cerebral Palsy: Children with mixed CP show features of more than one type of cerebral palsy. For example, some children have spastic CP with athetosis.
4. Monoplegic: Occasionally a child has monoplegic CP, in which only one limb is affected. Monoplegic cases are few.
20.2: CAUSES OF CEREBRAL PALSY
Cerebral Palsy may develop before birth, during birth, immediately after birth or during early childhood before the age of seven. We shall look at the causes at each stage in turn.
1. Causes before birth: This may be due to infections or abnormal development, for example:
- German measles (rubella)
- Syphilis
- Congenital abnormalities
2. Causes during delivery: Difficulties during delivery of a baby may cause CP:
- Premature delivery
- Head injury to the baby
- Prolonged labour leading to brain anoxia.
3. Causes after birth: Lesions on the brain following:
- Meningitis
- Cerebral Malaria
- Encephalitis
- Dehydration from diarrhoea
- Head injuries
- Neonatal jaundice
In many cases the causes are not known. It could be due to hereditary factors, or other factors not yet known. This is called idiopathic.
Having learned the causes of cerebral palsy let us now discuss the presentation of how to identify or recognize a child with cerebral palsy
.
Fig. 20.5: Athetoid Cerebral Palsy
.
Fig. 20.6: Ataxic Cerebral Palsy
Identifying Cerebral Palsy:
It was pointed out earlier in the text that CP is a major cause of developmental delay. Therefore, when identifying a child with cerebral palsy it is necessary to have a thorough knowledge of the various stages of childhood development.
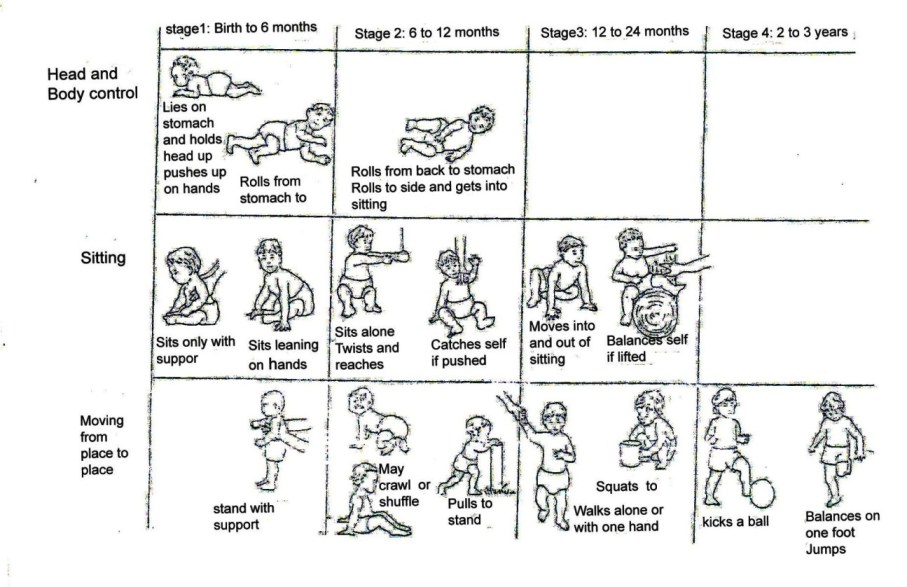
In normal development, developmental stages are reached in a particular order. Control of the body develops progressively from the head to the feet. Large movements (gross motor skills) develop before smaller more skilled movements. For example, a baby is able to control his/her head at 2-3 months whereas a child is able to put objects into a container and take them out at the age of 12-24 months. See Fig. 20.7. In a child with CP the stages are delayed and may not follow the same pattern.
Although a child with CP does not progress at the same rate as other children, the stages of normal development are still used as a basis for assessment, confirming diagnosis, training and stimulating the development of delayed milestones.
The particular development stages as outlined in Fig. 20.7 emphasises the development of movement, however, orientation is also achieved. The chart shows the order in which some abilities develop and the age at which most children learn them. Compare the information here with that indicated in the stages of development of a child with CP (See Fig. 20.3).
| 1
The development stages of a normal baby are used as one tool to recognise a child with cerebral palsy or development delay. Using your knowledge of these stages, list five developmental problems an 8-month-old child with CP is likely to have: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Compare your answer as you read on.
Assessment: A good understanding of normal child development helps you to identify children who are not developing as expected, to plan training, and to check on progress. Good assessment guidelines are a key to diagnosis of cerebral palsy:
- Take proper history, recording the date and age of the child and type of delivery.
- Watch what she/he can do and cannot do.
- Tick or circle what she/he can do on the development chart and cross what she/he cannot do.
- Carry out a thorough physical examination
- Try to work out the reason for a particular difficulty/problem.
.
Fig. 20.7: Developmental Stages In addition, use the information included in Table 20.1. In early stages of life, the child should be able to do the following with respect to age. Any deviation may mean that something is wrong. However, it is also very important to use the development charts that show the age at which some activities develop.
Table 20.1: Developmental Activities
| Activity | Appropriate Age |
|---|---|
| Postural control of the head when carried in arms | 6-8 weeks |
| Motor co-ordination of eyes and head | 16 weeks |
| Turning the head when a noise is made | 20 weeks |
| Transferring objects from one hand to the other | 28 weeks |
| Postural control of the head from lying prone | 6-8 weeks |
| Approach objects from lying prone | 16 weeks |
| Postural control of the head while body is pulled up | 8 weeks |
| Relationship of body with hands | 8 weeks |
| Feet to mouth | 20 weeks |
| Rolling over by him or herself | 20 weeks |
| Sitting by him or herself | 20-28 weeks |
| Crawling by him or herself | 24-28 weeks |
| Control the body in standing with maximum support | 6 months |
| Walk by him or herself | 12-15 months |
| Recognise mother’s face | 16 weeks |
| Smile at a mirror image | 20 weeks |
| Respond to a name | 28 weeks |
| Reach out persistently for toys | 32 weeks |
| Respond to words | 40 weeks |
| Show interest in pictures | 48 weeks |
A child with a developmental delay may have abilities spread over two or more stages. For example, a child with diplegia may be in Stage 3 for sitting, Stage 2 for getting to sitting and Stage 1 for standing. This means that training suggestions will have come from all three stages of child development. See Fig. 20.7.
20.3 EARLY SIGNS AND SYMPTOMS OF CEREBRAL PALSY
A baby with CP typically has abnormal muscle tone. The muscles may be either:
- Stiff (hypertonic)
- Floppy (soft, flaccid)
The early signs of stiffness or floppiness may be noticeable soon after birth. See Figs. 20.8 and 9. Other signs may take several months before they become obvious. To be sure that the child has cerebral palsy, take him to a doctor. The following signs are of concern if they are seen most of the time. Not every child will show all of these signs. In taking the history, listen for signs that the family has noticed.
Things Families Notice:
1. Sudden stiffening: In some positions, like lying on the back, it becomes difficult to bend the baby’s body, to dress or cuddle him/her. See Fig. 20.8.
Fig. 20.8: Hypertonic Muscle Tone
2. Unusual behaviour: He/she may be a crying, irritable baby who sleeps badly. Or he/she may be a very quiet baby who sleeps too much. He/she may not smile by the age of three months, as in normal development.
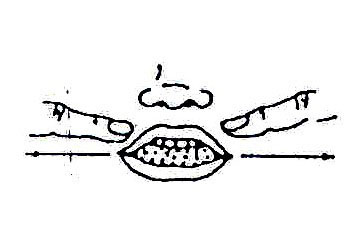
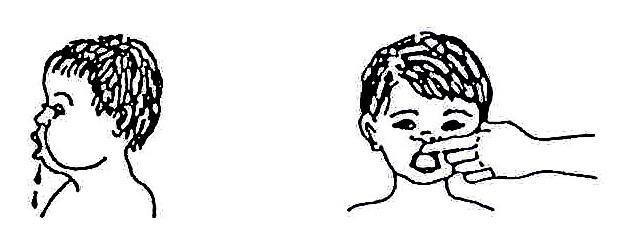
3. Poor feeding habits: The baby is not able to suckle properly and has difficulty in swallowing. Due to uncontrolled and uncoordinated muscle contraction, the tongue pushes milk and food out. The baby also finds difficulty in closing the mouth and using muscles of mastication.
4. Developmental delay: A baby with CP normally shows Slow development of milestones. For example, the ability to control the head may not develop after 2-3 months or even after six months. When a baby with CP is handled, the head falls from back to front and vice versa (See Fig. 20.3, Picture G).
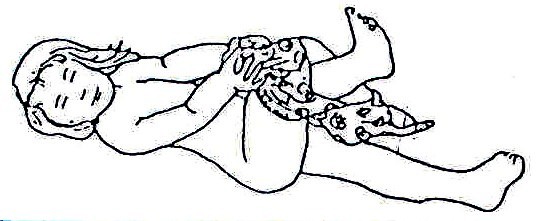
5. Floppiness: The baby’s head flops and he cannot lift it. His arms and legs hang down when he is held in the air. The baby moves too little. See Fig. 20.9.
Fig. 20.9: Floppy and Flaccid Muscle Tone
6. Unaware of some parts of the body: In the case of a child with CP who is also hemiplegic there is neglect of the paralysed half body. He/she is not aware of the affected side and therefore uses only the functioning side to perform all activities.
Other Problems:
Apart from the problems discussed above, other problems found in children with cerebral palsy include:
1. Visual impairment: The most common visual problem is a squint. It is important that babies with a squint are taken to an ophthalmologist for appropriate management. There may also be corneal opacities and blindness.
2. Hearing impairment and communication difficulty: Some types of CP, especially athetoid cases, have hearing impairment and communication difficulties. Such cases should be referred to ENT specialists and for speech therapy.
3. Personality/behaviour difficulties: Due to difficulties experienced by a CP child as a result of uncoordinated muscle action leading to delayed development, the child may become easily frustrated because he/she is incapable of carrying out tasks easily. She/he may give up. It is therefore important for the medical personnel, parents or carers to be patient and keep encouraging such children.
After recognising a child with cerebral palsy, the next step is to help them overcome their problems. Remember:
|
The principle objective of rehabilitation of these children is to train them to do what they are not able to do at a corresponding age. It is important for the medical rehabilitation workers to always talk with the child and his family, explain what is being done, why it is being done, and involve them in the process. Parental involvement is crucial. They need continuous support and counselling. |
| 2
List six activities you can carry out to help a child with cerebral palsy and his/her family to cope with their problems: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Do your plans of action include some of the ideas reflected in the following interventions?
20.4 MANAGEMENT AND INTERVENTION
While describing cerebral palsy in the earlier sections of this text, one of the major problems pointed out was developmental delay. Developmental delays interfere with the development of motor skills. The intervention which we shall discuss here will concentrate on facilitating development of milestones and training in motor skills: functional activities such as movement or mobility and other functional activities of daily living like self care, feeding, etc. This can best be done through physiotherapy, occupational therapy, and speech therapy services. The above named services are also referred to as medical rehabilitation services. It is important to start therapy as soon as the problem is noted. This is done when the child’s condition is stable. Always listen to parents when they think something is wrong they are often right.
| Parental involvement is crucial in the management of this child. Equally important is the counselling and continuous support to the parents/guardian of a child with CP |
Before discussing the techniques used in these services, let us state the aims of intervention or treatment. The main aims are:
- To train the mothers/parent/carer on proper and good handling of a child with abnormal muscle tone.
- To facilitate the development of milestones
- To train in motor skills and functional activities of daily living
- To prepare the child for social integration into the community
- Early detection and appropriate treatment of concurrent medical diseases
How best can these aims be achieved?
From the earlier sections of this text, you learned that abnormal muscle tone due to wrong impulses is the major cause of the movement and development problems had by a child with CP. To reduce or overcome these problems, the following physiotherapy, occupational therapy and speech therapy techniques are used.
Therapy aims at:
- Relaxing muscles
- Training in movement which encourages normal body postures
- Facilitating development of delayed milestones
- Training in activities of daily living. This involves working closely and effectively with the child, mother and family (Occupational therapy + Physiotherapy)
- Developing normal muscle tone and bulk (avoid disuse atrophy)
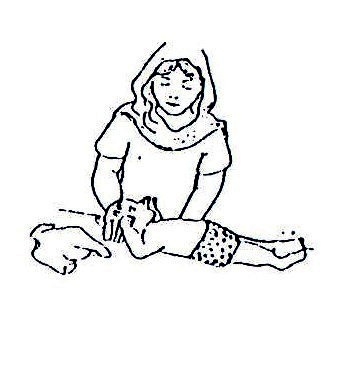
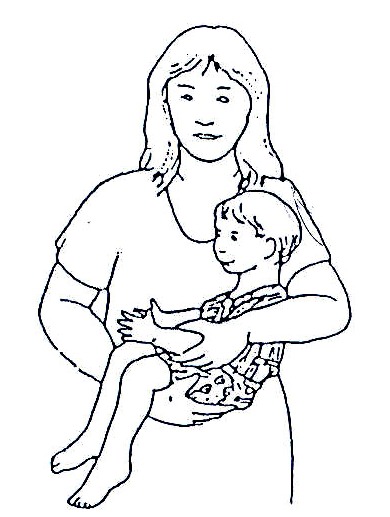
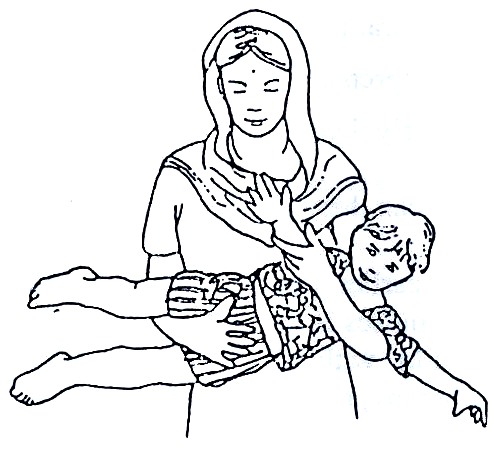
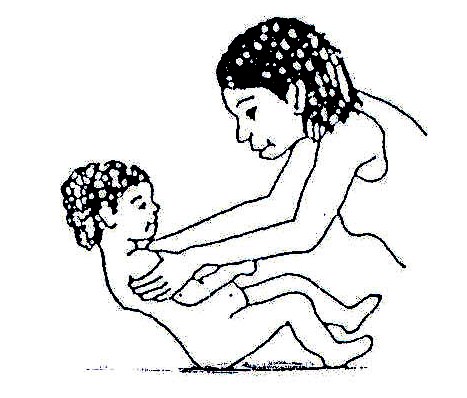
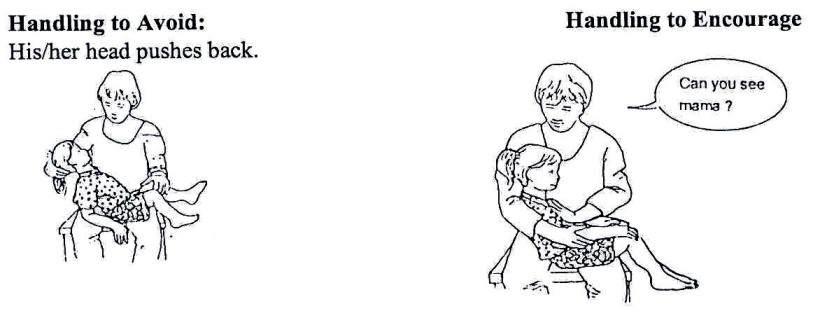
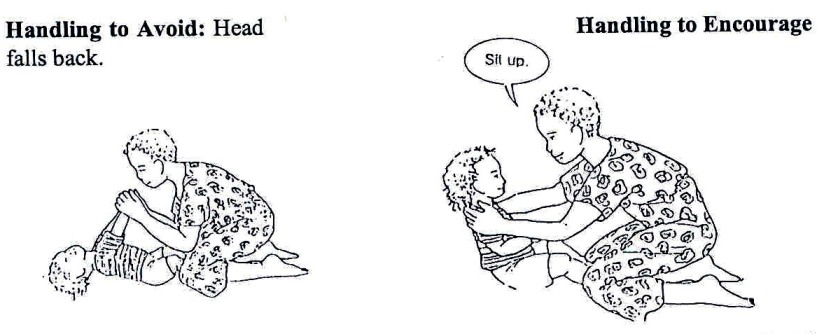
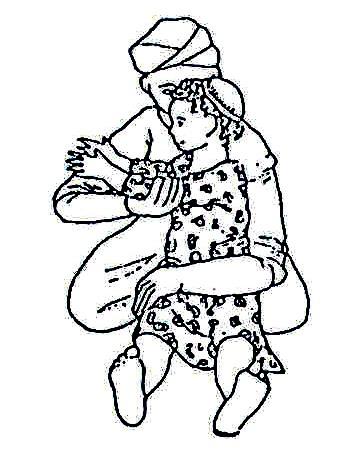
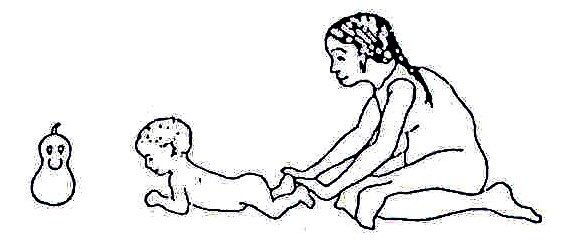
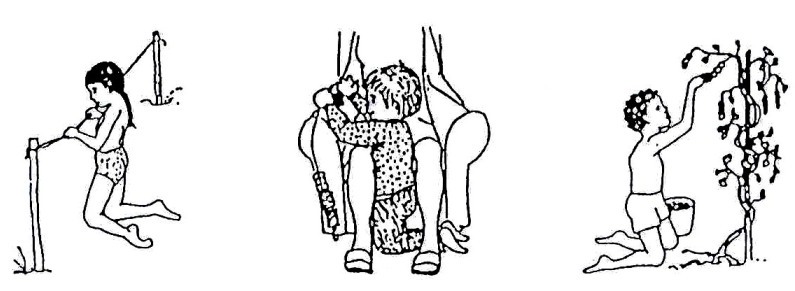
The first problem that a mother normally faces is how to carry and feed a baby with abnormal muscle tone. Through training the mother/carer, it is possible to overcome the problem. A pictorial illustration of good handling techniques is shown in Figs. 20.10 to 20.17.
Fig. 20.10: Lifting a Child with Abnormal Muscle Tone
LIFTING: To make it easier to lift the child and to prevent abnormal positions: a. Roll the child to one side and support the head b. Bend his/her legs c. Lift him/her close to your body d. Put him/her down the same way.
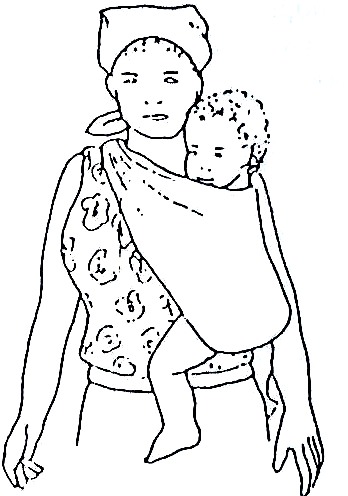
CARRYING: Carry him/her in a way which corrects abnormal positions and which brings both his/her arms forward. A more upright position helps him/her learn to hold his/her head up and look around.
Fig. 20.11: All very young children like to be held like this.
Fig. 20.12: A good position to straighten a spastic child
Fig. 20.13: A good position to carry a spastic child whose legs cross, or a floppy child
Fig. 20.14: A child can be carried on your back. If he/she needs more support or his/her head is floppy, carry him/her on your side.
Fig. 20.15: A good position to carry a spastic child whose legs cross, or an athetoid child. Use this for short distances. You can swing him/her from side to side in this position.
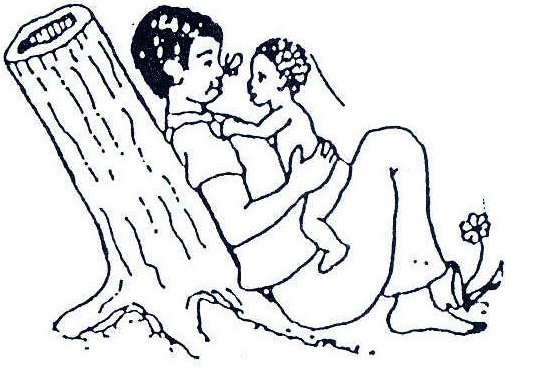
Fig. 20.16: As the child develops better head control, play with him/her, supporting his body firmly but with his/her head and arms free. Attract his/her attention with interesting objects and sounds, so that he turns his/her head first to one side and then to the other.
Fig. 20.17: If the child has trouble lifting his/her head when lying face down, lay him/her against your body so that he/she is almost upright. This way he/she needs less strength to lift his/her head
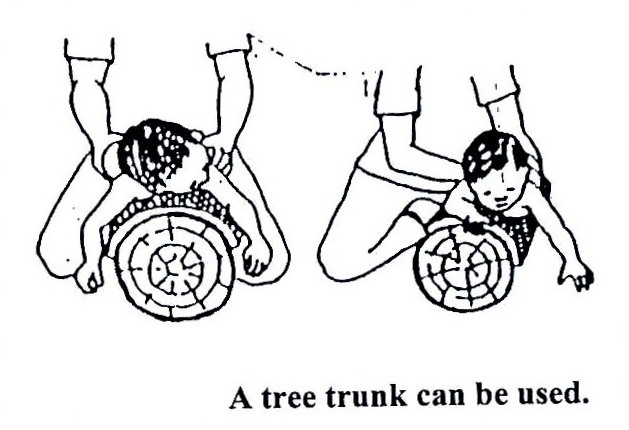
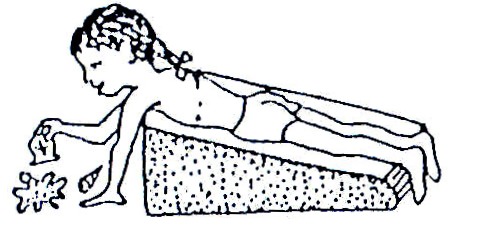
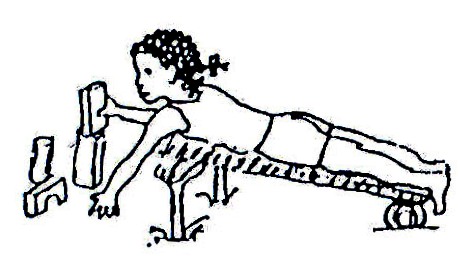
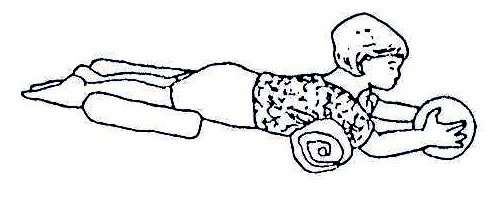
Lying face down is a good position for a child to begin to develop control of the head, shoulders, arms and hands, and also to stretch muscles in the hips, knees, and shoulders. However, some children have difficulty in this position.
You can encourage parents and caretakers to use some of the positions and ideas in the following pictures.
Fig. 20.18: Lying face down is good for development
Fig. 20.19: You can help the child with a wedge. Wedges can be made from stiff foam, plastic or layers of cardboard.
Fig. 20.20: A wedge can be made with a log, a board and a soft foam cover.
Fig. 20.21: A wedge can be made from a stick frame.
Fig. 20.22: A tree trunk can be used.
Fig.20.23: Or you can do the same thing with the child on your belly.
There are a number of activities that can help the child lift and control his/her head (and use his/her eyes and ears):
Fig. 20.24: To encourage the child to raise his/her head when lying down, attract her attention with brightly coloured objects that make strange or pretty sounds.
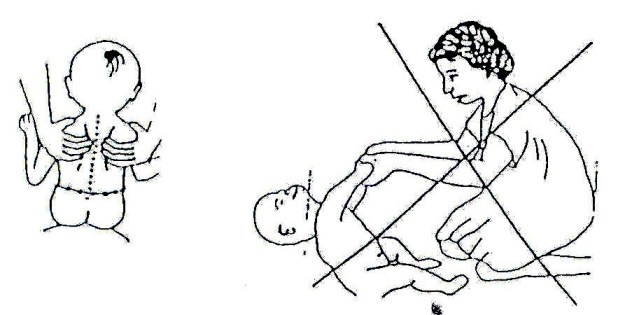
Fig. 20.25: If he/she does not raise his/her head, put him/her like this. Press firmly on the muscles on each side of the backbone and slowly bring your hand from his/her neck toward his/her hips.
Fig. 20.26: If the baby has trouble raising his/her head because of a weak back or shoulders, try placing a blanket under his/her chest and shoulders. Get down in front of him/her and talk to him/her. Or put a toy within reach to stimulate interest and movement
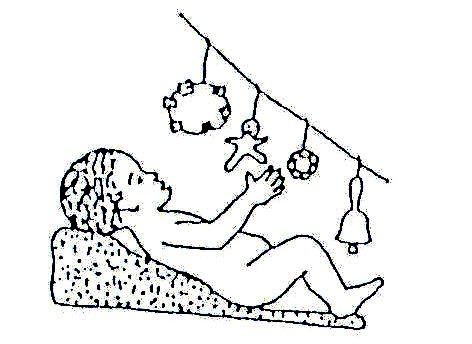
Fig. 20.27: Hang interesting toys, bells and rattles in front of him/her where the child can see and reach for them. This way the child learns to move his/her hand forward to take hold of the toy
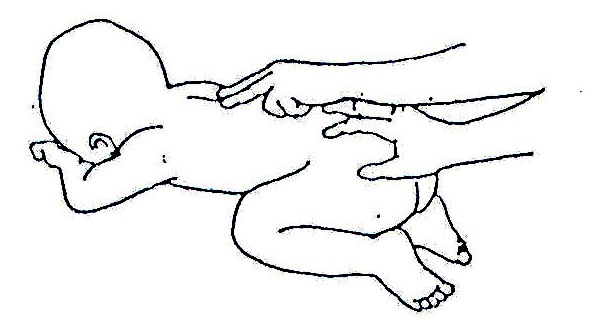
Fig. 20.28: To help him/her develop head control while lying face up, take his/her upper arms and pull him/her up gently until his/her head hangs back a little, then lie him/her down again.
Fig. 20.29: Do not pull the child up like this if his/her head hangs back! If a child with cerebral palsy stiffens as you pull his/her arms, try pulling the shoulder blades forward as you lift him/her up.
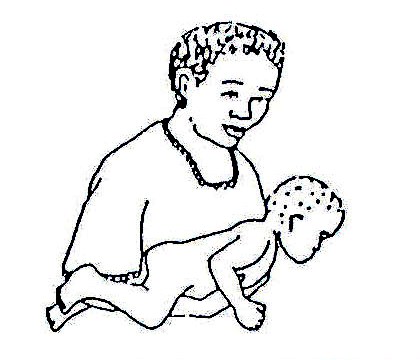
CARRYING THE CHILD
LIKE THIS HELPS!!!
Fig. 20.30: Carrying the child like this helps develop good head control, when she/he is face down.
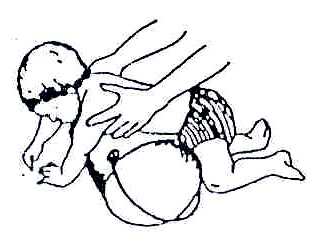
Fig. 20.31: Positions that keep the hips and knees bent and knees separate help relax and give better control to a child with cerebral palsy whose body straightens stiffly and whose knees press together
Fig. 20.32: Carrying baby like this frees his/her head and arms to move and look around.
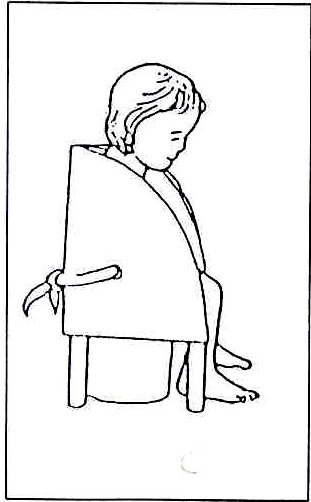
Fig. 20.33: A CP chair or corner seat can be made from wood, foam or cardboard.
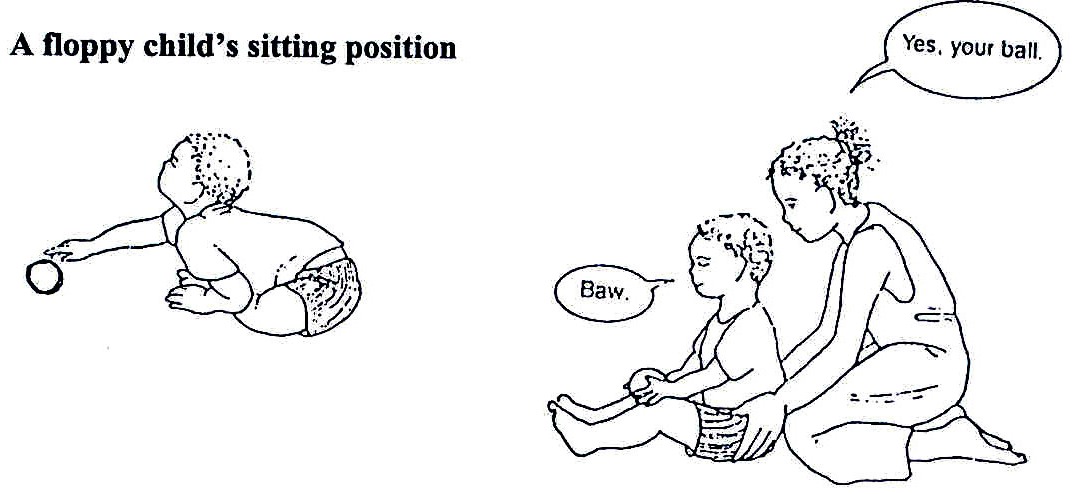
20.5 PREVENTION OF DEFORMITIES
Abnormal postures can lead to deformities. Let us discuss how deformities can be prevented.
Put the child in good position to avoid deformities and to allow him/her see what is around. A child sitting in a cerebral palsy chair (Fig. 20.33) is able to see what is going on around him/her compared to a child who is always lying down.
Fig. 20.34: Front Lying
Always handle the child carefully and gently so as not to evoke abnormal movements.
Let the mother hold, feed, bathe and dress the baby as you watch her and correct her where you feel she has done wrong and encourage her where she has done well.
Good Positions: A good position enables a child to do more for him or herself in a normal way. Allow him/her some movement rather than fixing him/her completely with equipment. Too much support does not allow him/her to learn to move. Change his position regularly.
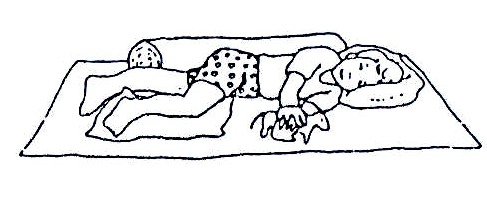
Lying Positions: Choose the position that corrects your child best. See Figs. 20.34 through 20.37.
Fig. 20.35: Front Lying with Blanket Roll between Legs
Lying on the front:
When lying on his/her front, place him/her on a roll, wedge or cushion. This keeps his/her arms forward and helps him/her to lift his/her head.
Hold floppy legs together with cushions or sandbags. Hold stiff legs apart with a blanket roll.
Straighten bent hips with two sandbags joined with a strip of material.
Lying on the side:
Keep both arms forward to bring his/her hands together. Bend one hip and knee. This stops the legs from pressing together and relaxes his/her body.
Fig. 20.36: Side Lying
Fig. 20.37: Lying on the back: Bring his/her head and shoulders forward. Bend the hips and knees. This prevents his/her body from becoming stiff and straight.
20.6 FACILITATING DEVELOPMENT OF MILESTONES
We have already discussed good handling and positioning techniques. Now it is time to consider the second aim of treatment: facilitating the development of milestones.
Head control is the first milestone that should be facilitated. This is because the child will not be able to learn other activities unless he/she is able to control the head and sit up to observe his/her surroundings.
After developing head control, progress can then be made in developing other milestones. Before continuing with the discussion, complete the following activity.
| 3
List the other essential milestones that should be developed: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
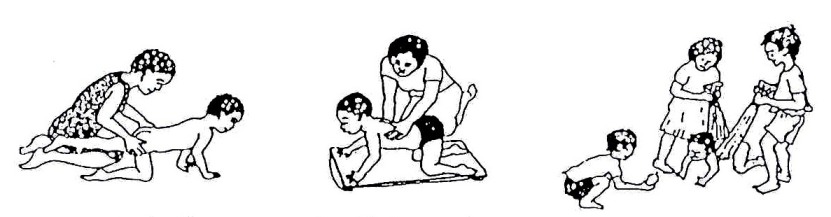
After developing head control, other milestones to be developed include sitting, crawling, standing and walking.
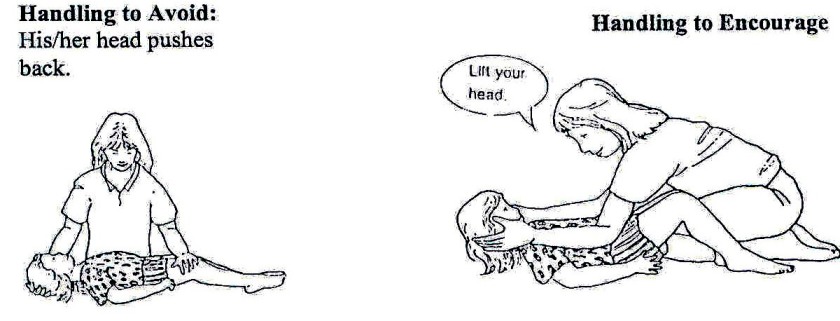
Handling and Training: Handling is a way of supporting and guiding a child so that his/her movements become more normal. Good handling relaxes a stiff child. It supports a floppy or athetoid child. It allows ataxic and athetoid children to control their movements more.
| Good handling is the basis of ALL training suggestions. It makes it easier to care for your child. |
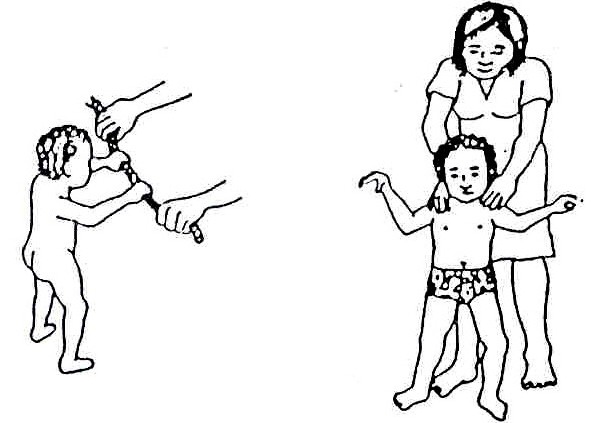
Handling the Head:
Fig. 20.38: Press down on the shoulders and tilt the head forward
Fig. 20.39: Bring both arms forward. Press on the chest to tilt the head forward.
Fig. 20.40: Hold the shoulders and lift slowly. Turn child to one side as you lift. This helps bring head forward.
Handling the Body:
Fig. 20.41: Handling to Encourage: To relax a spastic child: Twist the child’s body from side to side as shown. Twisting can also be done while the child is lying. For a bigger child, straighten his/her knees by putting your legs over them.
Fig. 20.42: To straighten the back, hold him/her around the hips. Press down. If he/she is very floppy, support the chest with one hand. Press down on the lower back with your other hand.
Fig. 20.43: To support his/her sitting, hold around his/her shoulders. Press them down and in to bring the arms forward. When his/her sitting is steady it is easier for him/her to look and listen.
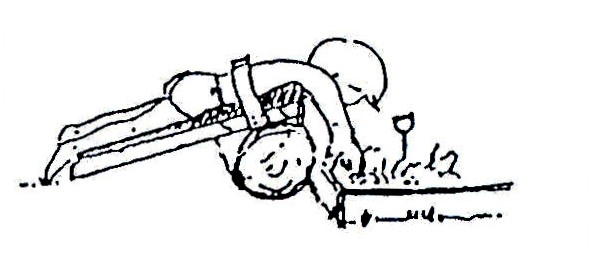
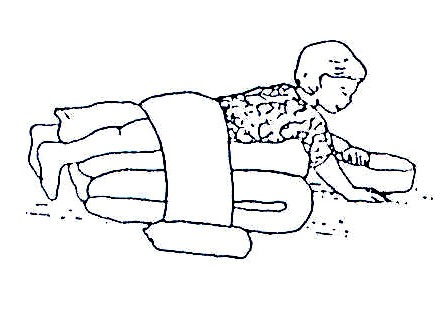
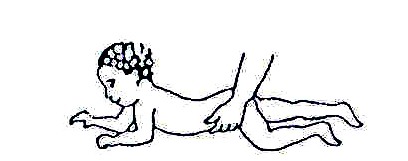
If the child can lift his/her head when lying on his/her stomach, encourage him/her to begin creeping in this way:
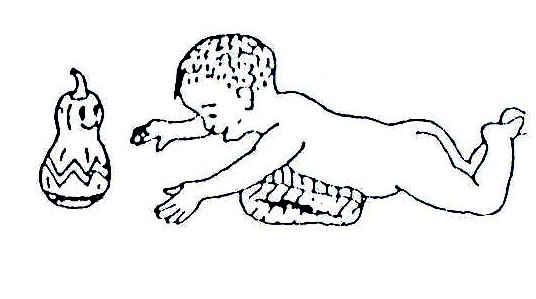
Fig. 20.44: Put a toy or food the child likes just out of reach. At first it may help to support his feet.
Fig. 20.45: If the child cannot bring his/her leg forward to creep, help him/her by lifting the hip.
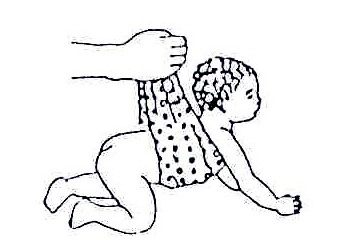
If the child has difficulty in beginning to creep or crawl:
Fig. 20.46: Let him/her “ride” your knee. Play “horsy” and slowly move your knee up and down and sideways so that he/she shifts his/her weight from side to side.
Fig. 20.47: Or put the child over a bucket or log. To help him/her bear weight with his/her elbows straight, firmly push down on his/her shoulders and release. Repeat several times
If the baby has trouble beginning to crawl, hold him/her up with a towel as in Fig. 20.49. As he/she gains strength, gradually support him/her less.
Fig. 20.48: Move the child from side to side so he/she shifts weight from one arm and leg to the other. Encourage the child to first reach, and later crawl, for something he/she wants.
Fig. 20.49: To encourage the child to crawl you can suggest these exercises.\
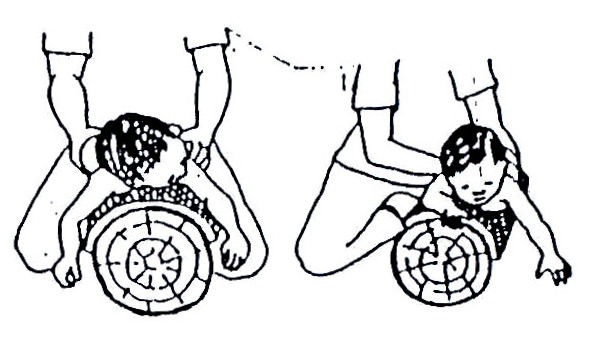
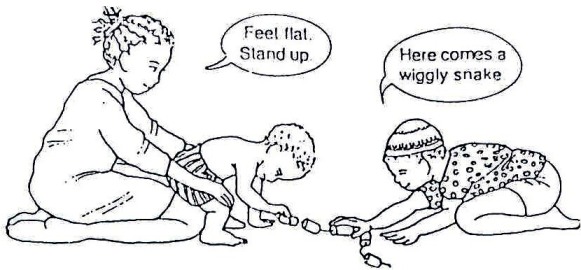
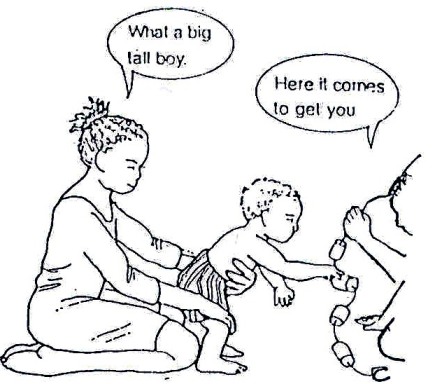
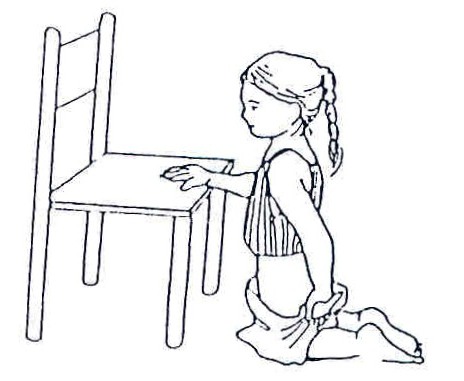
Moving Around: Pull to Stand: When pulling to stand, children need to lean well forward. Often they push back and this will make standing difficult. To move from sitting to standing correctly:
Fig. 20.50: Step One: Place his/her feet flat and underneath the knees. Press down on the knees while the child leans forward.
Fig. 20.51: Step Two: As he/she stands, support his/her chest and knees.
DO NOT LET HIM/HER LEAN BACK!
Fig. 20.52: Step One: To move from kneeling to standing, press down on one knee. Keep the other knee well back while he/she leans well forward. As he/she stands support his/her chest.
Fig. 20.53: Step Two: When standing, support him/her with your leg. Hold his/her hips straight and forward over his/her feet. Sift his/her weight from side to side.
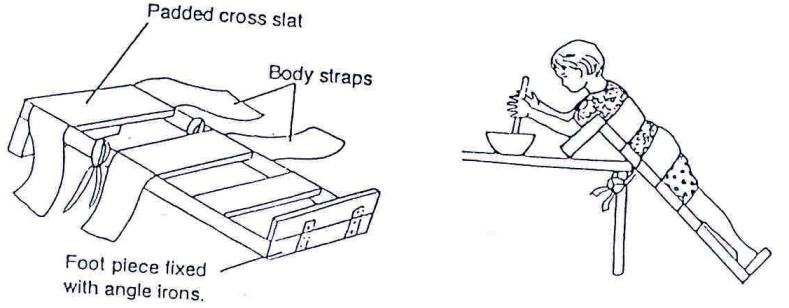
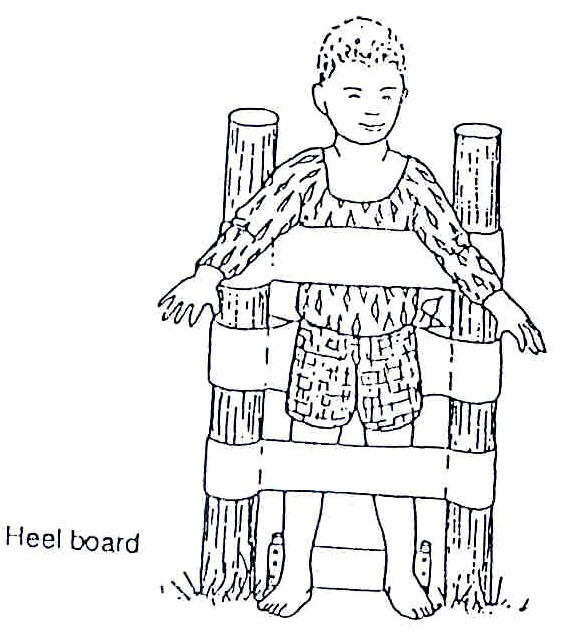
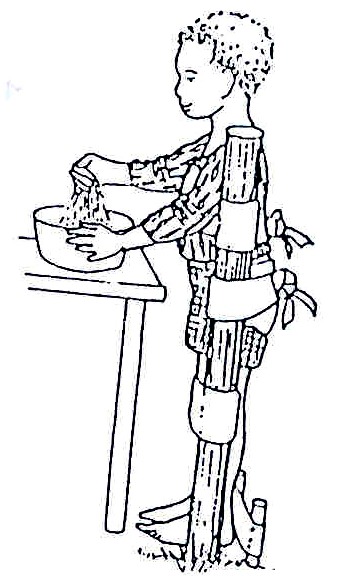
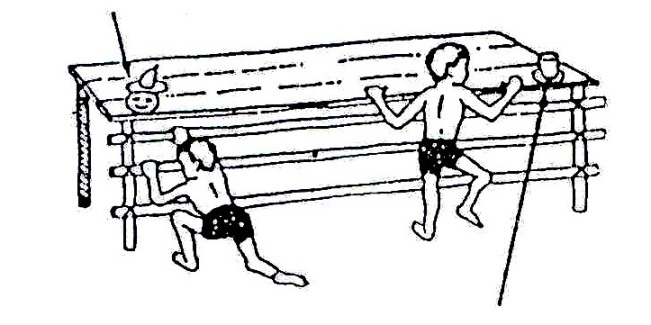
Position when standing: Children with delayed standing can benefit from standing supported in a good position. Many children will need equipment to be able to stand. Local artisans can make the equipment shown in Figs. 20.55 to 58 if directed by a therapist. Practise standing when washing, dressing, and playing.
Standing encourages the muscles that hold the body up to work. It prevents contractions and strengthens leg bones. The child has his hands free for play, can see and can communicate more easily with others.
Good Standing: Body in a straight line and feet flat with equal weight on both.
Fig. 20.54: If the child needs support to stand and his/her body is bent, or he/she cannot keep his/her heels on the ground, use a forward lean stander.
Fig. 20.55: If he/she needs less body support, use an upright stander. Make sure the upright poles are pushed well into the ground or fix them to a large square base for use indoors.
Fig. 20.56: For children who lean back, bring the chest strap right around the body. Tie at the back. Pull the ends of the bottom strap firmly to straighten the hips. Tie the ends securely over the bottom.
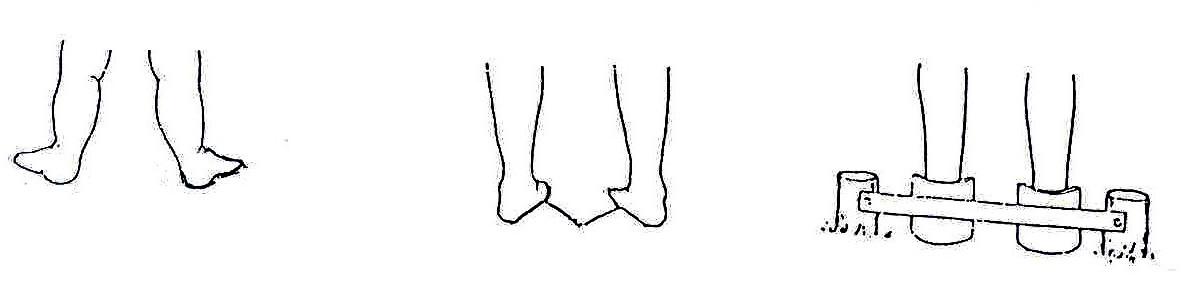
Fig. 20.57: If the feet turn out, as in the first picture, use wedges, foam or burnt bricks to correct the feet, as in the second picture. Make heel cups (in the third picture) from three layers of cardboard glued together, or from a piece of plastic drainpipe. Heel cups keep the feet straight.
After the child gets his/her balance on hands and knees, you can help him/her begin to stand – and walk – on her knees. He/she can walk sideways along a rope. There are many ways the child can practice standing on his/her knees and shifting his/her weight in ways that are fun and include him/her in family activities. See Figs. 20.59 to 20.63.
Fig. 20.58: Various ways a child can practice getting balance on knees
Fig. 20.59: When a child begins to stand, support the hips with your hands. Spread his/her feet apart to form a wide base. First do this from in front, later from behind. Move him/her gently from side to side, so that he/she learns to shift his/her weight from one leg to the other.
Fig. 20.60: Or have the child hold a hose or rope. Because it is flexible, he/she needs to balance more.
Fig. 20.61: To encourage a child to pull up to standing, put a toy he/she likes on the edge of a table.
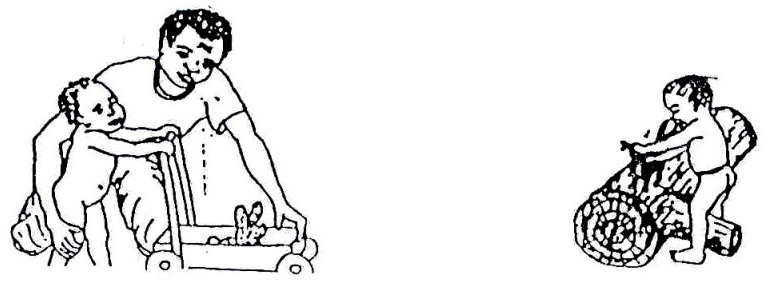
Fig. 20.62: Home made pushcarts or walkers can provide both support and independence for a child who is learning to walk or who has balance problems.
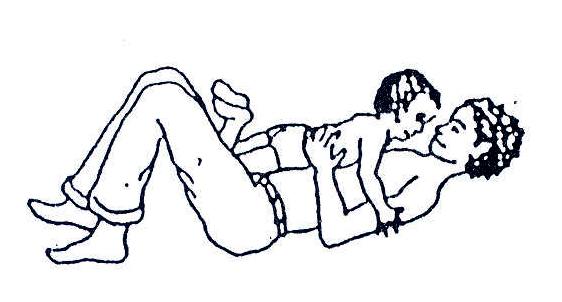
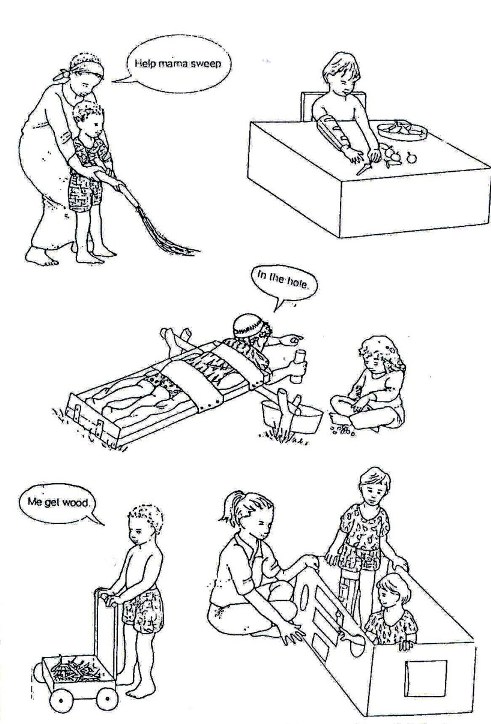
After training in movement skills, the next important activity is self care because the ultimate aim of rehabilitation is to help a child with cerebral palsy become independent and as self reliant as possible. See Figs. 20.64 to 66.
Fig. 20.63: Your child may find it easier to use a chair for support while dressing.
Dressing: If your child has learned to dress him or herself, he/she may need to hold onto things or lean against a wall for support. He/she should dress himself or herself while lying, kneeling or sitting. He/she can choose the position that is easiest.
Fig. 20.64: Or he/she can dress while lying down.
DRESS THE MOST AFFECTED SIDE FIRST AND UNDRESS IT LAST.
Fig. 20.65: Some children will be able to dress themselves while sitting.
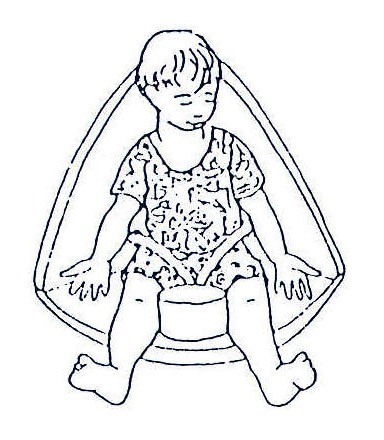
Toileting: As the child’s sitting balance improves, give him/her less support. Encourage him/her to help as much as possible with undressing and dressing when going to the toilet. If he/she can move onto and off the potty or latrine he/she should be encouraged to do this too.
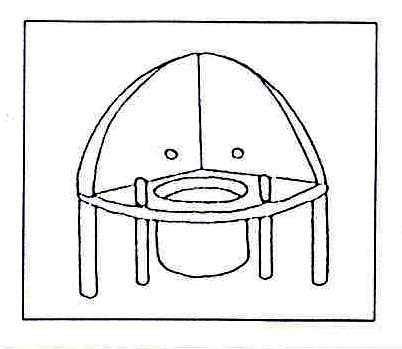
Fig. 20.66: A corner potty can be built that provides support for your child.
Fig. 20.67: Rods are used to keep the legs apart. A pear-shaped seat hole is better for boys.
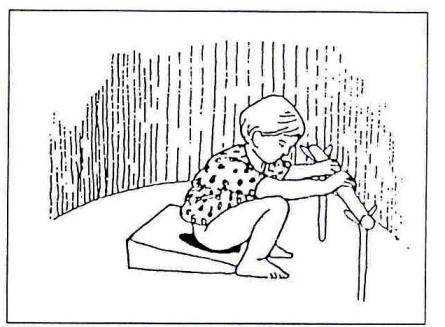
Fig. 20.68: If squatting balance is poor, give him/her a stick to hold and a wooden wedge or two bricks to sit on.
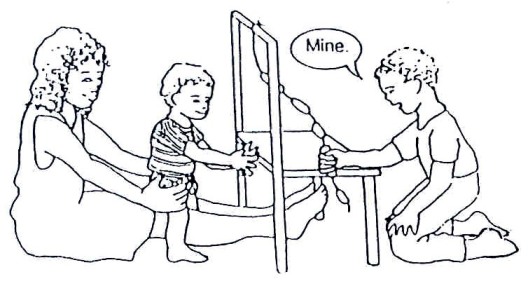
Opportunities to Play: Like other children, a child with cerebral palsy should be given an opportunity to play. See Fig.20.70. This can be done by:
- Designing some of the rehabilitation activities in the form of games or play
- Using brightly coloured toys
- Encouraging games with normal children.
After each treatment or rehabilitation session, the therapist should always design a follow up home programme for the mother or carer for continuity.
Fig. 20.69: Rehabilitation exercises can be designed in the form of games and play. Likewise, play with other children benefits the CP child socially and physically. While in play, the CP child can practice walking, improve his/her balance, step up and down, and integrate with other children.
Fig. 20.70: More examples of how a CP child can combine rehabilitation with play and self-help exercises.
Fig. 20.71: Using hands and playing. The therapist should always design a follow up home programme for the parents or caregivers for continuity.
20.7 SPEECH AND COMMUNICATION
While solving the problems of movement and functional activities, it is important to solve other associated problems that normally occur. These include visual impairment or blindness, hearing impairment or deafness, and communication or speech difficulties. For such problems please refer appropriately either to an ophthalmologist, ear, nose and throat specialist or to the speech therapist.
In discussing communication problems let us start with the following activity.
| 4
Communication and speech are problems that children with CP have to overcome. If you were asked to teach or train a child with CP how to speak, how would you do it? List six methods you would use to train such a child in communication skills _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
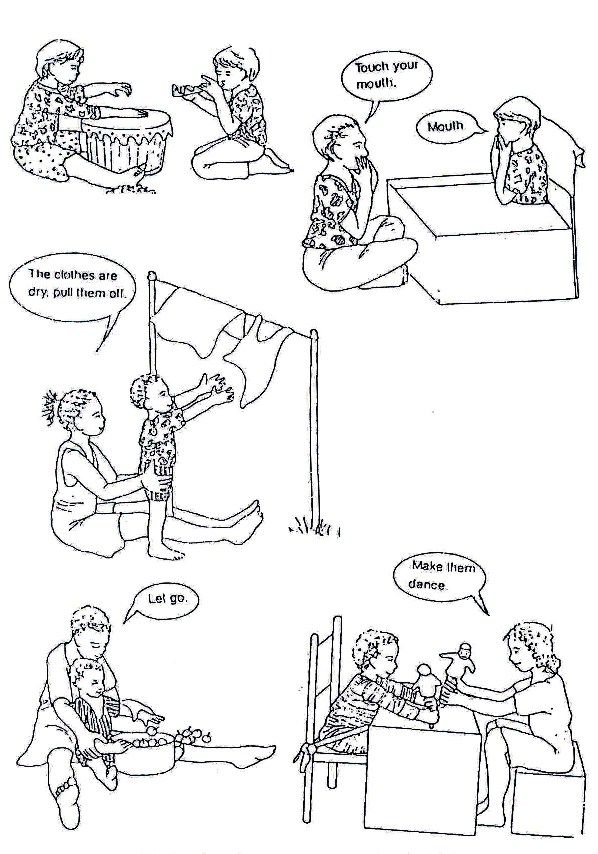
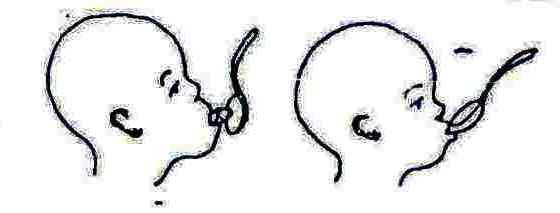
Learning in preparation for speech begins early, long before a baby says his/her first word. Speech develops out of body movement such as when using the mouth and tongue in eating or when using other senses. Speech develops also through interaction with people and things.
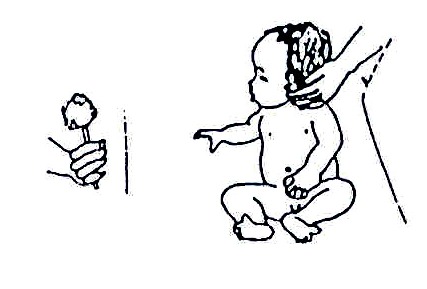
Fig. 20.72: Use a rattle to stimulate a delayed child.
One of the early stages in a baby’s development of speech is reacting and responding to different sounds. A delayed child may need extra help and stimulation.
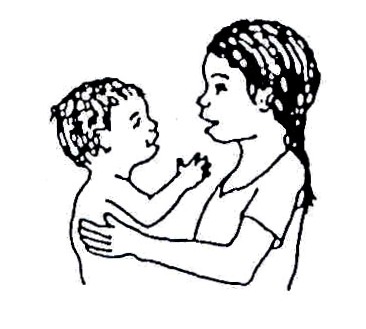
Make noises with bells, rattles, clickers and drums, first directly in front of the baby, then to one side, so that he/she turns his/her head. If he/she does not turn his/her head, bring the toy forward so that he/she can see it, and move it away again. Or, gently turn his/her head so that he/she sees what makes the sound. Help him/her less and less until he/she turns his/her head alone. Repeat the babble of the child. Have conversations with him/her in his/her language. When he/she begins to say words, repeat and pronounce them clearly and correctly – do not use “baby talk.”
Fig. 20.73: Speak with the child frequently.
To get the child used to the language, explain everything you do with him/her. Use clear, simple words, and use the same words each time. Name toys, objects, body parts. Repeat often.
Fig. 20.74: Explain everything to him/her.
Understanding language depends not only on hearing but also on watching lips and looks. So speak to a child on his/her level.
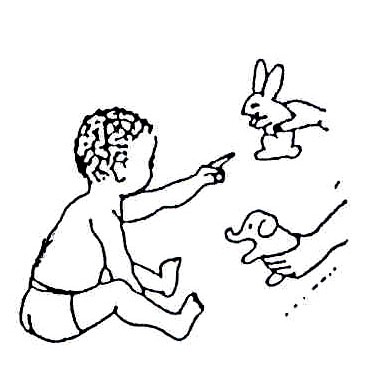
A child understands words before he/she can speak them. Play question games to help him/her listen and learn. He/she can answer your questions by pointing, nodding, or shaking his/her head.
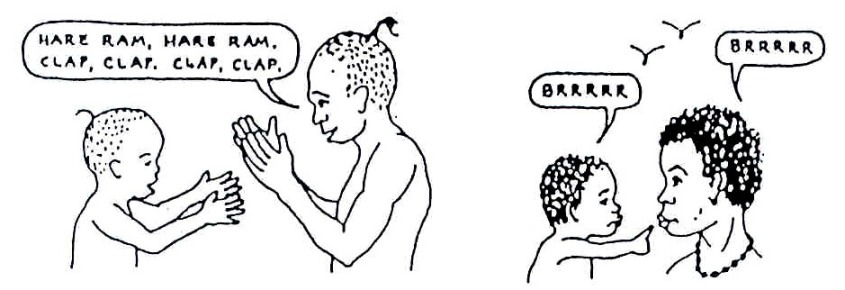
Rhythm is important to language development. Sing songs, play music, and have the child imitate body movements. Clap your hands, touch your toes, or beat a drum.
Imitate the sounds that baby makes and have him/her copy the same sounds when you make them. Then say words similar to those sounds. Also imitate use of the mouth: open your mouth wide, close it tight, stick out your tongue, blow air out, push lips in and out.
Fig. 20.75: Get down on your child’s level
Fig. 20.76: Play question games If the child’s mouth hangs open and he/she drools, do not keep telling him/her to close it! This will not help and will only frustrate the child.
Here are some suggestions to help correct the problem of drooling and to help strengthen the mouth, lips, and tongue for eating and speaking ability:
- Stroke or tap the upper lip, or gently press the lower lip several times.
- Gently stretch the lip muscles.
This may help the child to close his/her mouth. To strengthen the tongue and lips, put honey, a sweet or any sticky food on the upper and lower lips. Have the child lick it off.
Fig. 20.77: Clap hands, imitate sounds
Fig. 20.78: Stroke the upper lip or gently press the lower lip several times
Fig. 20.79: Or gently stretch the lip muscles. This may help the child close his/her mouth
Have the child lick sticky food from a spoon or suck sticky foods or candies.
Put food into the side of the mouth and behind the teeth so that the child exercises the tongue.
Fig. 20.80: Put sticky food on the upper lip
Have the child try to take food off a spoon with his/her lips. At 6 months, begin to give the child solid foods and foods he/she needs to chew. This helps to develop the jaw and mouth.
Fig. 20.81: Have the child lick food off a spoon to exercise muscles of the mouth
Note: a number of children with CP also have fits. Refer or treat these as part of therapy. Sometimes the fits may be difficult to control. In all ways progress may be very slow or not at all. Remember to encourage and counsel the parents and the child at each visit. Praise every milestone achieved.
20.8 COMMUNITY EDUCATION
In the previous discussion, we have concentrated on the role of the health worker towards the child, the mother and family. Let us now consider your role in the community and the role of the community towards a family with a cerebral palsy child.
| 5
List five areas of responsibility for the health worker to the community with respect to the issues of cerebral palsy: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Compare your lists with as you read on:
The responsibility of the health worker towards the community with respect to cerebral palsy includes educating the community as follows:
- Sensitisation and counselling of the community about CP and its disabling effects
- Causes and dispelling cultural beliefs
- Available interventions
- Positive attitude towards these children and their families
- Positive activities they can carry out to contribute to the well being of the child and family
- Preventive measures to reduce the occurrence of cerebral palsy and disability in general.
The responsibility of the community towards a family with a CP child includes providing morale support to families with disabled children by:
- Participating in all activities that create awareness in order to avoid stigmatisation,
- End the isolation of families with disabled children
- Advocate for equalisation of opportunities for children with disabilities
- To participate in community rehabilitation programmes.
20.9 PREVENTION
There are several things that can be done to prevent cerebral palsy. This can be done through:
- Encouraging mothers to attend antenatal clinics on schedule.
- Encouraging mothers to plan to be delivered by a trained health professional
- Encouraging mothers not to wait for too long while trying to deliver at home
- At the health facility ensure prompt delivery or referral if problems occur
- Good nutrition and enough rest for expectant mothers
- Girls avoiding pregnancy until 18 years of age
- Full immunisation for both mother and baby
- Practicing breast feeding
- Encouraging health seeking behaviour for all parent
- Prompt and appropriate treatment at the health facility
20.10 SUMMARY
In discussing this section the major areas covered included a detailed description of what cerebral palsy is, pointing out the various types and the disabling effects of this syndrome. The major causes were listed and available interventions described with illustrations. Roles played by rehabilitation health professionals and those played by the family and community were described. Finally, preventive measures were discussed. Always refer early any problem you cannot cope with.
PRACTICAL
In your health facility, identify a child with a disability. Make a point of visiting an occupational health unit and learn what they do. Visit a school near you and talk with the teachers on how they manage children with various disabilities.
Now take a break. Then complete the Tutor Marked Assignment.
|
DIRECTORATE OF LEARNING SYSTEMS DISTANCE EDUCATION COURSES
Student Number: ________________________________ Name: _________________________________________ Address: _______________________________________ _______________________________________________
CHILD HEALTH COURSE Unit 20: Assignment Disabilities And Rehabilitation Part 2:
1.Mukwana is a seven-year-old boy who is an athetoid CP (mild). Because of his unsteady, jerky, and wriggly movements, children who go to school with him always tease and laugh at him. He has now refused to go to school. What can you do to solve this problem? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
When you have finished this assignment, send it. It will be returned with comments together with the next unit. Remember to indicate your Personal File Number, names and address.
|
Our address is as follows:
Directorate of Learning Systems
AMREF Headquarters
P O Box 27691-00506
Nairobi, Kenya
Email: amreftraining@amrefhq.org