Lesson 17: Children's Mental Health Problems
Contents
[hide]INTRODUCTION:
Welcome to Unit 17 about children’s mental health problems, child abuse and neglect. As you can see, you have done very well. You are nearly finishing the entire course. So keep on the good work. Let us strive to keep children within our borders healthy.
Mental health refers to the health of the mind. The mind and the body are two inseparable parts of a whole human being. We can then say that what affects the body affects the mind, and vice versa. When we speak of mental health problems, we refer to persistent prolonged interference with someone’s personality and life as a whole. For a long time, mental health problems, especially those of the children, have not been given much attention.
There is increasing concern among health workers about the problem of child abuse and neglect. Although the magnitude of the problem is difficult to assess, it is almost certainly more common than is thought. In this unit, we shall look at common mental health problems among children and also the issue of childrens’ rights in this country and how we can enhance them. Now you have the opportunity to understand this information and use it to improve the health of all children in Kenya.
|
By the end of this unit you should be able to:
|
17.1. WHAT IS MENTAL HEALTH?
According to the World Health Organisation (WHO), mental health is a state of emotional well being which enables one to function comfortably within society and to be satisfied with one’s own achievements. Mental health also refers to the ability of the individual to carry out his/her social role and to be able to adapt to his/her environment.
Thus the absence of good mental health in children interferes with their ability to develop their full potential in life. In this unit we shall discuss three common mental health problems among children. These are:
- Mental retardation;
- Strange behaviour;
- Epilepsy
We shall start our discussion by looking at mental retardation.
17.2. COMMON MENTAL HEALTH PROBLEMS
Mental Retardation
| 1
What do you understand by mental retardation? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now read the text that follows and see if your ideas are included.
Mental retardation is a developmental disability characterized by a significant limitation in both the intellectual function and adaptive behaviour. A mentally retarded child has certain limitations in mental functioning and in skills such as communicating, taking care of him or herself, and social skills. These limitations will cause a child to learn and develop more slowly than a typical child. Children with mental retardation may take longer to learn to speak, walk, and take care of their personal needs such as dressing or eating. They are likely to have trouble learning in school. They will learn, but it will take them longer. There may be some things they cannot learn.
The onset of mental retardation is before the age of 18 years.
Causes
Various factors cause mental retardation in the period before birth, during birth and after delivery. Let us look at the factors in each stage.
- Before birth:
- Infections like German measles (Rubella), cytomegalovirus infection, toxoplasmosis, Human immunodeficiency virus infection, herpes simplex infection and syphilis;
- Poor nutrition during pregnancy;
- Toxins: alcohol, herbs, cocaine, lead, maternal tobacco smoking;
- Hereditary causes: one or both parents may be of low intelligence;
- Placental insufficiency;
- Chromosomal disorders;
- Congenital malformations of the central nervous system.
- During delivery:
- Extreme prematurity;
- Hypoxic-ischaemic injury;
- Intracranial bleeding during difficult or forceps delivery;
- Low blood sugar;
- Increased blood bilirubin levels;
- Infections (herpes simplex, bacterial meningitis).
- After delivery:
- Infections (encephalitis, meningitis);
- Severe head injury;
- Lack of oxygen;
- Low blood sugar levels;
- High blood sodium levels;
- Toxins (lead);
- Intracranial bleeding;
- Malnutrition;
- Poverty and family disorganization;
- Dysfunctional infant-caretaker interaction;
- Parental psychopathology;
- Parental drug abuse.
A child’s brain needs stimulation to function properly. If a child is emotionally and/or intellectually deprived or neglected, his intelligence may suffer permanent damage.
Clinical manifestations
The delayed achievement of developmental milestones is the main symptom. If you see a child who is very late in achieving his or her milestone, you should suspect mental retardation.
Diagnosis
The diagnosis of mental retardation is made by looking at two main things. These are:
- The ability of a child’s brain to learn, think, solve problems, and make sense of the world (intelligence quotient or IQ); and
- Whether the child has the skills he or she needs to live independently (called adaptive behavior, or adaptive functioning).
Intelligence Quotient (IQ)
The diagnosis of mental retardation requires finding of sub-average intellectual functioning. A child who has an intelligence quotient of 70 or below is said to have a significantly sub-average intellectual functioning.
Intelligence quotient is the ratio between child’s mental age and his/her chronological age multiplied by 100. Mental age is the age level at which the child is functioning. For example, a 10- year-old who copes with normal activities at the level of a 5-year-old has a mental age of five. That child’s is intelligence quotient is 5 ÷ 10 x 100 = 50. Such a child has mental retardation. The normal intelligence quotient is 75 to 120.
A low IQ together with deficits in the following adaptive skills is indicative of mental retardation. These skill areas are:
- Communication
- Self care skills (eating, personal hygiene and toileting)
- House keeping/home living skills
- Social/interpersonal skills
- Using public transport
- Health and safety
- Self-direction
- Learning ability
- Leisure
- Working skills
Classification of mental retardation:
Children with mental retardation have uniformly low performance in all kinds of intellectual tasks including learning, short term memory, use of concepts and problem solving. Mentally retarded children can be classified under four main categories.
a. Mild retardation (IQ 55 – 70):
These children have normal language ability and social behaviour. They can go to school but will perform poorly.
b. Moderate Retardation (IQ 40 – 55):
Most of these children can talk, all of them learn to communicate and most learn to care for themselves with supervision.
c. Severe Retardation (IQ 25 – 40):
The development of these children is generally slow. Many of them can be trained to look after themselves under supervision and can communicate in simple ways.
d. Profound Retardation (IQ 20 – 25):
A few of these children learn to care for themselves completely. Some achieve simple speech and social behaviour.
Mentally retarded children may also have sensory/motor disabilities, epilepsy, and incontinence. They may also be prone to fits, burns and domestic/home accidents.
You can also identify a child with mental retardation by comparing him with children of a similar age or by going through the following development milestones.
Table 17.1: Development Milestones
| Age | Physical Development | Social Development |
|---|---|---|
| 3 months | Finger gripping | Smiles, recognises mother |
| 6 months | Sitting | Attachment to care takers, interests in toys and sounds |
| 9 months | Rolls over, able to stand | Begins to feed self |
| 1 year | Walks, runs | Drinks from cup, obeys simple instructions |
| 3 years | Can walk on tip toe, can grasp small objects | Toilet trained |
| 5 years | Hops on one foot, can throw and catch a ball | Helps with simple work, bathes and dresses self |
Well, we hope you are now able to diagnose a child with mental retardation. Next let us look at how you can manage a child with mental retardation. But first, complete the following activity.
| 2
The Local Council Chairperson (LC) reports that there are several mentally retarded children in his community 1. What would you do to help these children? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ 2. How would you prevent the occurrence of mental retardation in this community? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now confirm your answers as you read the following discussion.
Management:
The management of a child with mental retardation involves health education rather than drug intervention. You, as a health worker, are responsible for early detection of mental retardation and supporting the parents to cope with the problem. The management goal is helping the child achieve his/her maximum potential. This goal is achieved with the participation of the following people:
- Teachers from the Special Education Division of the Ministry of Education and the staff of the Education, Assessment Resource Services (EARS)
- Psychiatrists or psychiatric clinical officers.
- Physiotherapists
- Occupational therapists
- Speech therapists and
- Child psychologists.
A child with mental retardation may have or develop other problems such as a physical disability, epilepsy, deafness or blindness or behaviour disorder. You should refer such a child to the relevant health facility for management. Depending on the developmental stage of a given mentally retarded child, you and the parents should carry out the following activities:
- Organise occupational therapy programmes in areas of self help, such as toileting and feeding;
- Refer to a speech therapist to assist the child with language and speech;
- Counsel and explain to the parents about the mental retardation and its outcome;
- Advice the parents to initiate activities of daily living like cooking, sweeping and washing;
- Provide opportunity for vocational/income generating activities such as tailoring, mat making, brick making etc;
- Advice the parents to help the child to learn to make use of leisure time playing such as games, story telling, singing etc;
- Show the parents exercises that stimulate physical development such as exercises to help the child to sit, stand and walk;
- Encourage the community to form self help parent groups that can help in supervising treatment programmes as prescribed in hospital such as occupational, physiotherapy, speech therapy and drug therapy;
- Advice the parents to encourage the establishment of regular habits like eating and sleeping;
- Advice the parents to encourage integration of the child in family activities;
- Encourage parents whose children are able to learn to send them to school;
- Educate the community about malaria, diarrhoea and vomiting since these medical conditions aggravate mental retardation. Stress the importance of their early diagnosis, prompt and thorough treatment;
- Encourage the establishment of relief care or part-time replacement .
Prevention
As we learned from the section on the causes of mental retardation, genetic factors, pre-natal factors, perinatal factors and postnatal factors contribute to the occurrence of mental retardation. So to prevent the occurrence of mental retardation, you should try to minimise the above causes.
Other measures of preventing mental retardation include the following:
- Genetic counselling: Explain to couples the possibility of having a similar child if they have one already. Discourage women from giving birth before 20 years of age or after 35 years.
- Provision of optimum antenatal care: Advise pregnant mothers to: have a balanced diet with supplements of folic acid; avoid alcohol and cigarettes; obtain proper immunisations; and be tested for syphilis and for HIV infection. If infected they should seek the appropriate treatment and adopt preventive measures of mother to child transmission of HIV infection. They should also be screened for cephalopelvic disproportion and organized to deliver in hospitals, maternity centres or with well trained traditional birth attendants.
- Postnatal prevention:
Treatable conditions such as hydrocephalus, high blood bilirubin levels, low blood sugar levels, high sodium levels and hypothyroidism should be recognized promptly and treated properly.
You should also advice the parents or caregiver to provide a nurturing and growth promoting environment especially by:
- providing appropriate stimulation;
- preventing trauma accidents and poisoning;
- Ensuring regular health supervision; and
- protecting children from communicable diseases such as malaria and diarrhoeal diseases.
Having looked at mental retardation, let us now discuss the second type of mental health problem in children.
Psychological Disorders
Psychological disorder is an abnormal behaviour. Here we shall learn about the following types of psychological disorders:
- A developmental disorder referred to as childhood autism;
- A behaviour disorder called attention deficit hyperkinetic disorder;
- Another behaviour disorder called conduct disorder;
- An emotional disorder with onset specifically in childhood such as separation anxiety, sibling rivalry, phobic anxiety or states.
There are general, but not specific, causes of psychological disorder or abnormal behaviour.
Before you read on do the following activity.
| 3
What are the likely causes of psychological disorders in children? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now read the text below about the causes of psychological disorders in children to see if your answers match with ours.
General Causes
There are a number of general causes of psychological disorders in children. These include:
- Hereditary Factors: These do not cause the disorders directly but rather they cause the predisposition to develop some kind of disorder such as autism or attention deficit hyperkinetic disorder;
- Physical Diseases: These are the same as the ones we mentioned in mental retardation. The amount of damage to the brain directly correlates with the rate of psychiatric disorder. Minimal brain damage can account for otherwise unexplained disorders such as overactivity, inattention, conduct disorder, and deficits in learning and perception.
- Environmental/Social/Cultural Factors: A child needs a stable secure family background with a consistent pattern of emotional warmth, acceptance, help and constructive discipline. Prolonged separation or loss of parents can have a profound effect on the psychological development of the child. Poor relationships in the family may also have similar adverse effects.
These family factors are:
- Discordant relationships such as violence, quarreling, deviance;
- Illness or personality deviance or loss of parents;
- Large family size – a child may not get enough attention;
- Child abuse practices such as physical violence, burning, and sexual abuse;
- Physical deprivation such as inadequate clothing or food can make a child emotionally depressed.
The rate of childhood psychiatric disorders is high in areas of social disadvantage. Examples of social disadvantage include:
- Inadequate social places such as social centres where children can meet and play indoor and outdoor games.
- Overcrowded living conditions with children sleeping under the parents’ beds in huts.
Having looked at the general causes of psychological disorders, let us now discuss each type of disorder and also its management
Types of Disorders and Clinical Features
1) Childhood Autism:
This is a severe mental disorder with onset before 3 years of age. It affects the brain and makes communicating and interacting with other people difficult. A child with autism often has delayed language development, prefers to spend time alone, and shows less interest in making friends. Another characteristic of autism is what some people describe as "sensory overload": Sounds seem louder, lights brighter, or smells stronger. Although many children with autism also have mental retardation, some are of average or high intelligence. This disorder occurs most frequently in males 3 – 4 years of age.
Thus autism is characterised by the following:
- impairment in reciprocal social interaction;
- impairment in communication;
- markedly restricted, repetitive and stereotyped behaviour.
Let us look at each in turn.
a) Impairment in Reciprocal Social Interaction
This impairement manifests with:
- Lack of awareness of existence or feelings of others (treats a person like a piece of furniture, does not notice another person’s distress, apparently has no concept of others for privacy).
- No or abnormal seeking of comfort at times of distress (does not come for comfort when ill, hurt or tired; seeks comfort in stereotyped ways).
- No or impaired imitation (does not wave bye-bye, does not copy mother’s domestic activities; mechanical imitation of others action is out of context).
- No or abnormal social play (does not actively participate in simple games: prefers solitary play activities; involves other children in play only as mechanical aids)
- Gross impairment in ability to make peer friendships (e.g. no interest in making peer friendships, lacks understanding of social conventions). In the autistic child this refers to impairment of eye contact, facial expression, body postures and gestures. This child will not develop normal peer relationships. He/She lacks the ability to spontaneously seek to share and enjoy the achievements of others.
b) Impairment in Communication
An autistic child has:
- Poor mode of communication such as communicative babbling, facial expression, mime or spoken language;
- Markedly abnormal nonverbal communication as in the use of eye-to-eye gaze, facial expression, body posture, or gestures to initiate social interaction (e.g. does not anticipate being held, stiffens when held, does not look at the person or smile when making a social approach, does not greet parents or visitors, has a fixed stare in social situations);
Absence of imaginative activity such as playacting of adult roles, fantasy characters or animals; lack or interest in stories about imaginary events;
- Marked abnormality in the production of speech, including volume, pitch, stress, rate, rhythm and intonation (e.g., monotonous tone, questionlike melody, or high pitch);
- Marked abnormalities in form or content of speech including stereotyped and repetitive use of speech (echolalia), use of ‘you’ when ‘I’ is meant;
- Marked inability to initiate or sustain a conversation with others ;
- Repetitive stereotyped use of language;
- Lack of make-believe play and social imitative play. In other words, an autistic child will not play-act “mother-father” games.
c) Restricted, Repetitive and Stereotyped Behaviour
This manifests with the following:
- Stereotyped body movements, e.g., hand -flicking or twisting, spinning;
- Head banging, complex whole body movements;
- Persistent preoccupation with parts of objects e.g., sniffing or smelling objects, repetitive feeling of the texture of materials, spinning wheels of a car
- Marked distress over changes in trivial aspects of the environment;
- Unreasonable insistence on following routines in precise detail;
- Markedly restricted range of interests and a preoccupation with one narrow interest, e.g., interested only in lining up objects, interested only in a toy which the child repeatedly dismantles and reassembles
- An autistic child is typically pre-occupied with one or more stereotyped and restricted range of interests with marked need for sameness.
Investigations.
In investigating an autistic child, you need to carry out a thorough history taking, physical examination and mental observations. This can give you a reliable diagnosis. You should also rule out the presence of malaria or syphilis with relevant laboratory investigations for effective management.
Management
Management consists of four main aspects:
- Intense behaviour therapy beginning before 3 years of age and targeting speech and language development. This improves language capacity and later social functioning. Behaviour therapy involves rewarding a positive behaviour and ignoring or discouraging a negative one also works.
- Providing special education services. An autistic child may need to attend a special school and can be placed through Education Assessment Resources Services (EARS).
- Social skills training. This involves training the child in self care and activities of daily living (feeding, hygiene and sleeping) and integrating the child in the community
- The family of an autistic child needs considerable help to cope with the child’s behaviour. You should continue encouraging the parents and offering them support because the outcome of the management is often minimal and parents need a lot of patience. The parents may obtain help by joining voluntary organisations. Local chapters or groups could be formed such as National Federation for Mental Health. Neighbours and other community members could help to take care of the child in order to give the parents some time off.
- Pharmacotherapy with risperidone or olanzapine is indicated when autism is associated with hyperactivity, tantrums, physical aggression, self-injurious behaviour, panic attacks, stereotypes and anxiety symptoms especially obsessive-compulsive behaviours.
2. Attention Deficit Hyperkinetic Disorder
This is a behavioural disorder characterised by inattentiveness, impulsivity and motor overactivity. A child with this disorder usually has learning disabilities, irritability, aggression, temper tantrums and destructiveness, recklessness and proneness to accidents. Such a child has poor concentration which leads to learning difficulties. He or she may also have minor forms of anti-social behaviour such as disobedience, temper tantrums and aggression. The onset is early, usually between the ages of 1-5 years.
Management
In the management of a child with hyperkinesis, it is important to identify the danger signs. These signs include:
- Extreme and persistent restlessness
- Impulsiveness and recklessness
- Temper tantrums
- Aggression
All these make such a child prone to accidents and require immediate attention. Just as we saw in an autistic child, you may need to carry out laboratory investigations to rule out malaria and syphilis. The management of a child with attention deficit hyperkinetic disorders involves provision of behaviour therapy; special education; parent counselling, group, family and individual psychotherapy; occupation therapy and drug treatment. Let us describe each of these management approaches in turn.
a. Behaviour therapy:
This involves modification of behaviour in order to reduce a targeted behaviour such as over-activity. It starts by establishing a regular daily routine that a child is expected to follow. Both the parents and teachers are advised to reward the child consistently with praises and giving of tokens whenever the child demonstrates the required behaviour and permitting consequences whenever the child does not meet the goal. The rules are kept simple, clear and as few as possible. These rules are coupled with setting of firm limits and are enforced fairly and sympathetically. Dangerous or breakable things should be kept out of reach of the child. Overstimulation and fatigue should also be avoided You should advise the parents to reward by praising them and giving tokens.
b. Parent counselling
Educating the parents about the child’s difficulties can help them change from seeing the child as “bad boy or girl” to seeing his or her need for help. This change may reduce punitive attitudes and help in emphasizing the child’s need for structure and consistency.
c. Occupational therapy:
This involves gradual introduction of normal activities to distract the child from the unwanted behaviour. You should advise the parents to encourage the child to concentrate on a given activity. They should do this by rewarding her/him when he/she remains with the activity for a longer period.
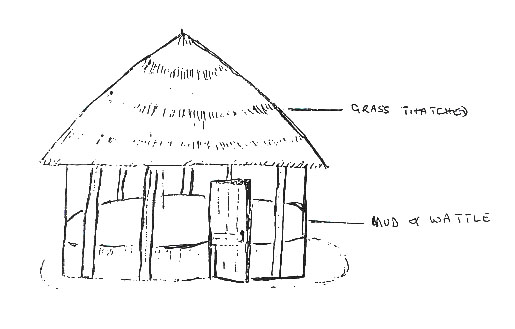
Some parents may be tempted to tie the child to a tree or tie the child’s limbs together. This should be discouraged. A better way of occupying a hyperactive child is by providing a play house with toys (see figure 17.1 for an illustration of a simple play house).
Fig.17.1 Play house for a child with attention deficit hyperactivity
The house is made of mud and walled up to the child’s eye level. This allows the child to play in a well-lighted environment and when she/he is tired she/he is able to look around. The level of the wall should not be so low as to allow the child to climb and jump over. You should select toys that will not harm the child or cause accident.
Drug therapy
Drug therapy for hyperactive children is sometimes effective. You should refer these children to a hospital where they can be managed. Drug management through Methyl-phenidate is prescribed at a referral hospital. Start with 2.5mg morning × 4/7. Then 2.5mg morning, 2.5mg noon and gradually increased to 10 mg morning and noon. Side effects include irritability, depression, insomnia, headache, upper abdominal pain, and poor appetite. High doses lead to suppression of growth. Therefore the growth of a child on this drug should be closely monitored. Drug free periods (weekends, holidays) should be used when practical to reassess the need for continued medication. 66% of children treated show improvement with the drug, but it is usually reserved for severe cases due to side effects. You need to give support to parents as it may be difficult to change the child’s behaviour.
Advising the teachers
Teachers have a vital role in the management of children with attention deficit hyperactive disorder since they can be supportive and assist with behaviour modification. You should therefore:
- Explain the condition of the child to his/her teachers;
- Encourage the teachers to accept and be patient with the child;
- Advise the teachers to reward positive behaviour;
- If the child is on any drug, explain the likely side effects.
Special education
Children with severe learning disabilities need special education. So you should recommend and refer them to specialists.
Conduct Disorder
A conduct disorder is a repetitive and persistent pattern of behaviour in which either the basic rights of the others or major age-appropriate norms or rules of the society are violated. Children and adolescents with this disorder have great difficulty following rules and behaving in a socially acceptable way. Conduct disorders form the largest single group of psychiatric disorders in older children and younger adults. Children with conduct disorders are often viewed by other children, adults and social agencies as "bad" or delinquent, rather than mentally ill
Before you read on do the following activity. It should take you 5 minutes to complete.
| 4
List 4 possible causes of conduct disorders: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Now read the following discussion and check if your answers were correct.
Causes of Conduct Disorder
The causes of conduct disorders are many and include the following:
- Genetic factors;
- Frustration;
- attention deficit hyperactivity disorder;
- brain damage;
- unrecognized low intelligence;
- product of teenage pregnancy;
- single motherhood;
- severe reading retardation;
- parental examples of antisocial behaviour;
- parental discord;
- depression in the mother;
- early maternal deprivation;
- early institutionalization;
- unemployment
Manifestations of conduct disorder
The manifestations of these disorders include:
- stealing more than once;
- running away from home at least twice or once without returning;
- lying often (except for avoiding physical or sexual abuse);
- fire setting;
- truancy;
- breaking into a house, a building or a car;
- destroying others’ property;
- cruelty to animal;
- rape,
- fighting using a weapon (stone, bat, gun, knife etc) more than once;
- initiating physical fights often;
- stealing with confrontation of the victim (mugging, purse snatching, extorsion, armed robbery);
- cruelty to people;
- conning;
- staying out at night despite parental prohibition.
A child with a conduct disorder has significant impairment in academic, social and occupational functioning.
Diagnosis
A child has a conduct disorder if he or she displays any three of the above manifestations for at least 6 months. Psychological testing should be done to exclude an emotional condition masking as conduct disorder. Neuropsychological tests are done to exclude learning disability.
Management
Mild disorders subside with no treatment. The more severe ones are treated with a combination of educational support, individual psychotherapy, family therapy, parent management training, and psychopharmacotherapy. Lets look at each type of treatment in turn.
- Educational support is given in the form of remedial education and special education in some cases.
- Individual psychotherapy focuses on alliance building and conflict resolution. It is somewhat effective in establishing the basic trust necessary for a positive therapeutic outcome. The individual is also trained in problem solving. The training in problem solving involves modelling, role playing, and practising to help the children to become more successful in interpersonal relations. It enables the children to modify maladaptive styles of relating and behaving.
- Parent management training enables the parents to develop specific skills for altering the interaction patterns maintaining the aggressive and antisocial behaviour. Inadequate child rearing skills are an example of such patterns. The parents are trained to change their preoccupation with conduct problems to emphasize on promoting prosocial behaviour at home. You should encourage the family to set clear rules of what is acceptable and unacceptable behaviour, to enforce the rules strictly, to define predictable patterns of punishment when a rule is broken, to provide positive reinforcement, to learn and carry through a programme of practical problem solving for the difficulties that arise, and to ensure that they know where the child is at any given time and ensure that the rules are being obeyed.
- Family therapy is designed to improve communication among family members and explore the underlying conflicts (difficulties) so that they can be more equitably resolved. Family therapy is particularly useful for maintaining the gains acquired when the child is hospitalized or placed in another setting. Without family therapy, the problem would recur when a child returns home.
- Pharmacotherapy is indicated in those children whose conduct disorder is associated with attention deficit hyperactivity disorder, depression or anxiety. The treatment of conduct disorder and follow up must be prolonged.
So far we have discussed mental retardation, psychological disorders and conduct disorders. Next let us discuss anxiety disorders.
Anxiety Disorders
Anxiety disorder is a condition in which excessive anxiety is the principal symptom. Anxiety is a complex emotional response to an unknown or a known very minor danger.
As a group, the anxiety disorders are the second most common disorders, after conduct disorders, with onset in childhood. Examples of anxiety disorders include the following:
- Separation anxiety disorder;
- Sibling rivalry: This is when children who follow each other closely fight for mother’s attention and love;
- Phobic status: A fear of specific objects or situations, such as high height, darkness, water;
- Selective mutism: This is a deliberate way of refusing to talk when there is no physiological cause;
- School refusal.
Let us briefly elaborate on the anxiety disorder known as separation anxiety.
Separation Anxiety
Of the above examples, separation anxiety disorder is the most common. Separation anxiety disorder is inappropriate and stems from excessive fear concerning separation from home or from those to whom a child is attached to. It manifests with:
- Recurrent signs or complaint of excessive distress in anticipation of being separated from home;
- Persistent refusal or reluctance to go to school because of fear of separation from attachment figure;
- Persistent reluctance to go to sleep without being near the major attachment figure;
- Persistent avoidance of being alone with clinging to the mother wherever she goes;
- Repeated dreams and nightmares about separation;
- Persistent complaints of symptoms such as nausea, vomiting, stomachache, headache, dizziness, polyuria and enuresis on many school days or other occasions that involve separation from attachment figure. ;
| 5
Describe how you would manage a child with separation anxiety in your community: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Read on to see if your answer is the same as ours.
Management
You should manage separation anxiety as follows:
- Identify the possible stressors (causes) so that you can reduce or remove them;
- Together with the carer, you should counsel the child by encouraging him or her to talk about his/her worries or fears;
- Counsel the family to help them understand their own anxiety or overprotection and how it affects the child;
- Use a behaviour therapy approach of rewarding good behaviour, as we have already discussed;
- Refer the child to the hospital. In the hospital, imipramine tablets are prescribed. The dosage of imipramine tablets is 12.5 mg every 12 hours or each night for a child aged 6-10 years. is tablets
Next let us look at another mental health problem among children, known as epilepsy.
Epilepsy
Epilepsy, commonly known as “falling sickness” is a brain disorder that causes people to have recurrent seizures (convulsions). A seizure (convulsion) is a single, sudden, transient, spontaneous and stereotyped neurologic event such as abnormal movements, abnormal posture, abnormal behaviour, sensory disturbance and autonomic dysfunction with or without loss of consciousness. The seizures happen when clusters of nerve cells, or neurons, in the brain send out the wrong signals. People may have strange sensations and emotions or behave strangely. They may have violent muscle spasms or lose consciousness Seizures occur in 0.3-0.5 percent of the population. The incidence is highest in infancy.
Causes
A seizure is caused when clusters of nerve cells, or neurons, in the brain send out the wrong signals. In the majority of cases (primary or idiopathic seizures), the cause of the abnormal electrical activity in the brain is unknown, and the children are developmentally normal. In secondary seizures, the children are neuro-developmentally abnormal with a static or progressive lesion or metabolic disorder. The following are some of the causes of secondary seizures:
- Head injury;
- Birth trauma;
- Brain tumours;
- Infections like cerebral malaria, meningitis, encephalitis, etc.;
- Alcohol and drug abuse;
- Abnormal nerve cell organisation (some people are born with it).
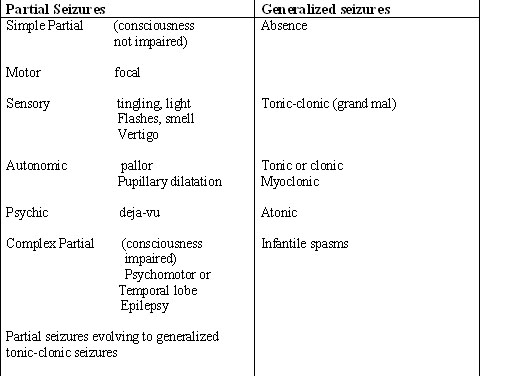
Classification of Seizures
The modern system of seizure classification draws an essential distinction between partial and generalised seizures. If the excessive electrical discharge is restricted to a given (localised) area in the brain, the seizure is termed partial. If the entire brain is involved, the seizure is generalised Table 17.2 gives the differences between the two.
The classification is essential for determining the causes, selecting appropriate therapy and giving important information on long term outcome. Depending on the epileptic focus, partial seizures manifest with motor, sensory, autonomic and psychic disturbances. In simple seizures, consciousness is not altered. In complex partial seizures, and in partial seizures with secondary generalization, as in the generalized seizures, there is loss of consciousness. Generalized seizures on the other hand result from abnormal electrical activity that is bilateral and manifests with abnormal movements and loss of consciousness so that the subject is not aware of the occurrence of a seizure.
Table 17.2: Classification of Seizures
The following are the various types of epilepsy:
- Grand mal (generalised tonic clonic seizures);
- Petit mal (absence seizures);
- Jacksonian seizures;
- Temporal lobe epilepsy
Let us look at each in turn.
Grand mal (Generalised tonic clonic seizures)
Grand mal (generalized tonic-clonic seizures) are the most common childhood seizures.
Signs and Symptoms:
A characteristic aura (irritability, myoclonic jerk, or cry) introduces an attack. The aura is followed by a sudden loss of consciousness, a fall from a standing or seating posture, generalized stiffness, arrest of breathing with cyanosis, and upward deviation of the eyes. There may be biting of the tongue as well as passage of stool and urine. Jerking movements of the whole body and frothing at the mouth follow. After an attach or fit, the child may sleep or appear confused for some time. Attempts to restrain these children may provoke violence or aggression.
Immediate Management:
To manage a child with a grand mal seizure, you should advice the parents or caretakers to:
- Keep calm;
- Prevent the child from hurting himself/herself by removing him/her from fire, water, traffic and other dangers;
- Protect the child’s head with something soft or with the hands;
- Loosen tight clothing around the neck, waist and chest;
- After the seizure turn the child on the side to help breathing;
- After the seizure subsides, to stay with the child to comfort him or her. The child may be tired and may need to rest;
- Allow the child to continue with what he or she was doing after recovery;
- Dress or attend to any cuts that may occur during the seizure;
- Record the seizures in a book set up as an epileptic chart;
- Seek medical attention from the nearest health facility;
- Encourage the child with epilepsy to take drugs as advised by medical personnel and to continue to do so until advised otherwise. Provide regular follow-up of a child with grand mal epilepsy.
|
DO NOT DO THE FOLLOWING:
|
| 6
How do members of your community view epilepsy? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Well done! Now read through the text below and see if your ideas are included.
Common misconceptions of epilepsy
You should educate the community that epilepsy is not infectious and dispel the common misconceptions in the community. Reassure them that one cannot catch epilepsy from another person. Epilepsy is not caused by witchcraft or evil spirits. Coming in contact with urine, faeces and saliva passed during a seizure will not pass on the illness to you. The gas/wind passed by a child having a seizure is not infectious. Sharing utensils with a child with epilepsy will not pass the illness to you.
Long Term Management
A child with epilepsy must take the drugs continuously as prescribed for a long time. Children with epilepsy should participate in normal community activities. Children with epilepsy should be discouraged from drinking alcohol (that is in older children). Recovery is only partial. When drugs are discontinued, 40% or more suffer recurrences of seizures.
Safety for the Child
You should advise parents of a child with grand mal epilepsy to do the following:
- Make simple arrangements at home, at school, or at work to keep the child from being hurt while having a seizure.
- Discourage a child with epilepsy from going to the well alone and he/she should not swim alone.
- Raise and/or protect fireplaces.
- Discourage climbing of trees and ladders.
- Discourage driving vehicles.
Differential Diagnosis:
There are other conditions that present with a seizure but are not necessarily grand mal epileptic seizures. These conditions include:
- migraine,
- fainting,
- breath holding spells,
- hyperventilation,
- pseudoseizures, etc.
As a health worker you need to be able to differentiate an epileptic seizure from other sorts of seizures. The following features are useful in helping you to make a clinical diagnosis of grand mal seizure.
- Two or more fits in the last 12 months occurring in the absence of fever, alcohol or other drugs, or intoxication withdrawal;
- Loss of consciousness lasting one minute or more;
- Tonic movements, such as generalised stiffening;.
- Clonic movements such as thrashing about and one or more of the following:
- Sphincter disturbance: loss of urine or faeces during the seizure
- Sleep, drowsiness or confusion after the seizure
- Muscle soreness after the seizure
- Injuries such as tongue biting or head cuts
- Froth coming out of the mouth
- Falling
Older children, for example children eight to twelve years of age, may experience pseudo-seizures that may be confused with grand mal seizures. The following guidelines may help you to differentiate pseudo-seizures from grand mal seizures.
Table 17.3: Differentiating Pseudo Seizures from Grand Mal Seizures
| Pseudo Seizure | Generalised Tonic Clonic Seizures |
|---|---|
|
|
A child with grand mal epilepsy may have complication of status epilepticus. This is a condition characterized by continuous, recurrent seizures without regaining consciousness in between the seizures. It is a medical emergency.
Management of a child with status epilepticus:
- Position the child on his/her side and keep the upper airway clear;
- Insert a firm but soft object, like rubber piece, between the teeth;
- Insert rectal valium 5 mg to start. If no response, repeat the dose;
- If no response, give an injection phenobarbitone loading dose of 15 mg intramuscularly or intravenously– 8 mg per kg body weight. Then continue with oral medication as per drug treatment of epilepsy.
Next let us look at the other type of epileptic seizure known as absence seizures or petit mal.
Absence seizures (petit mal):
“Absence seizures” are generally rare. They are more common in children than in adults. Absence seizures are characterized by sudden brief loss of consciousness, stopping of whatever activity the child is doing, a blank facial expression, and flickering of the eyelids. They last 10-20 seconds. Immediately after the attack, the patient resumes the preseizure activity. The child usually does not fall but he/she does not respond during the seizure. There is frequent unexplained dropping of things by the affected child. A child may have 5 - 200 attacks in a day.
Management:
Children with petit mal seizures will not present with recognisable seizures, and what may be observed is only the unexplained dropping of things. Advise the parents to be observant and identify other signs of the condition. You should then refer the child for further management.
Jacksonian Epilepsy (Partial Motor Seizure)
In this type, uncontrolled movement begins in one part of the body (usually one hand) and spreads to the face and the leg of the same side. Sometimes the attack may generalise, ending in grand mal seizure. Unless it becomes generalised, the child remains fully conscious. The child experiences weakness of the convulsing limb sometimes for several hours following a seizure.
Management
You should advise the caretaker to move the child away from dangerous situations or objects at the onset of the seizures as the movement spreads. You should encourage the child/caretaker to seek medical attention.
Temporal Lobe Epilepsy (Complex partial seizure, psychomotor epilepsy)
A child with temporal lobe epilepsy experiences an aura warning. He/she may experience a feeling of fear, stomach upset, or odd smell and taste. The child may also hear or see things that are not there, exhibit abnormal behaviour such alteration of consciousness, arrest of activity, staring, automatisms, violence or aggression. Automatisms includes swallowing, chewing, licking, lip smacking, rubbing the face, mumbling and fumbling with objects. Complex automatisms include moving in circles, removing clothes or continuing ongoing activity aimlessly. At the end of the seizure the child does not remember what happened and consciousness returns slowly. Many children with temporal lobe epilepsy have generalised clonic seizures as well. In a given child the sequence of events in the seizure is almost always the same from one seizure to the next.
Management
You should advise the parents to take the following measures:
- Move the child away from dangerous things or situations at the onset of aura;
- Restrain the child in case of psychological disorders;
- Encourage the child/caretaker to seek medical attention;
- Refer such a child to hospital for investigations to be done. An electroencephalogram is done to confirm the diagnosis and a head x-ray is done to rule out fracture of skull.
This type of epilepsy is difficult to control and high doses of drugs are required.
So far we have described the four types of epilepsy: grand mal epilepsy, petit mal epilepsy, Jacksonian epilepsy and temporal lobe epilepsy. For each of these conditions, we have also discussed the general management. We shall now describe the drugs used in the treatment of epilepsy. But before then you should do the following activity.
| 7
List the drugs you have used or seen being used to treat epilepsy: _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
I hope your answers included the following drugs which are used in the treatment of epilepsy.
Drug Treatment
*Phenobarbitone
Phenobarbitone is useful in the treatment of grand mal epilepsy. It is cheap, effective and readily available. Table 17.4 shows the doses of phenobarbitone according to a child’s age and weight.
Table 17.4: Phenobarbitone Dosage for Children
| Dose | 2 – 5yrs
up to 15 kgs |
6 - 10yrs
15 - 20kg |
|---|---|---|
| 1st dose (starting dose) | 15 – 30 mg | 15-30mg |
| 2nd dose (maintenance dose) | 15-30mg | 30-60mg |
| 3rd dose (maximum dose) | 45-60mg | 75mg |
At the start of treatment you should review every child every month. At every visit you should check the response to the drug, compliance and ask about any side effects. If at the next visit there are no seizures reported, you should maintain that dose and review progress every four weeks. The maximum dose for each child will depend on control of seizures and tolerance of side effects. Give a child 5 mg per kg body weight in one or two divided doses. A child may present side effects of phenobarbitone. The most common side effects are:
- Drowsiness
- Tiredness
- Poor balance
- Poor concentration
- Restlessness
In most cases side effects of phenobarbitone wear off with time and some are tolerable to patients. In some children, phenobarbitone causes overactivity.
*Phenytoin sodium (Epanutin): This drug is indicated in grand mal and temporal lobe epilepsy. Ask the caretaker when the child has a seizure. For example, if he/she has seizures mostly at night, then give a single dose at night. If the child has seizures during the day and at night, then give the drug in the morning and at night.
The dosage is 5 – 8 mg per kg of body weight in one or two doses. Some children on this drug may experience side effects such as nausea, vomiting, dizziness, headache, tremor, transit nervousness, ataxia (unsteady gait), gingival-hypertrophy and anaemia. Phenytoin sodium is indicated for grand mal epilepsy when the child has failed to respond to phenobarbitone.
*Ethosuximide (Zarontin)
This is indicated in absence seizures (petit-mal). You should give ethosuximide as follows:
- Below six years give 250 mg every twelve hours.
- Above six years give 500 mg every twelve hours.
Some children on this drug may experience side effects such as nausea, vomiting, drowsiness, dizziness, and ataxia.
*Carbamazipine (Tegretol):
This is the drug of choice for temporal lobe epilepsy. You should give this drug to children 5 years old and under, 100 – 200 mg every 6 - 12 hours. The side effects are like those of phenytoin.
| 8
What important health messages should you give to a child or caretaker about treatment of epilepsy? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Health Messages in Treatment of Epilepsy
You should educate the child/caretaker about the following:
- Medication controls the seizures but does not cure epilepsy;
- The aim of treatment is to reduce the seizures to the possible minimum. For some patients this could mean no seizures, but for others, this means fewer seizures. Treatment is completely effective in only 70-80% of patients;
- Treatment does not produce immediate effects. It takes two to six weeks before the drugs reach a protective level;
- Parents should not alter prescribed drugs regardless of degree of seizure control. Only health worker can modify the prescribed doses;
- Parents should avoid abrupt stopping of drug intake as this may precipitate continuous seizures;
- The parents should ensure that they have a constant supply of drugs before they run out;
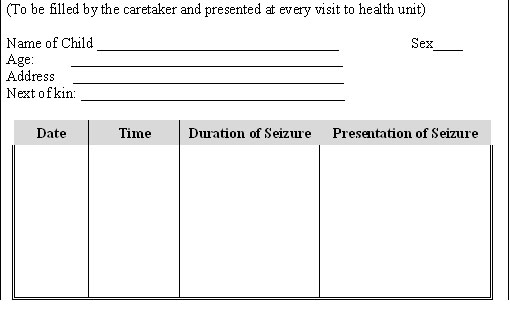
- Child or caretaker should fill in the epileptic chart indicating the date, time, and duration of seizures and describing the presentation of the seizure. Such a chart would look like the one in Fig. 17.5.
17.5 Epileptic Chart
So far we have looked at the common mental health conditions in children. We discussed quite a number of them and I hope you have learnt quite a lot from that section. In the next section we shall discuss child abuse and neglect.
17.3: CHILD ABUSE AND NEGLECT
A child is totally dependent on the parents or guardians for care right from birth to the time they become an adult. This care is enshrined in the rights to which the child is entitled. A society or community protects its children through observing and respecting these rights.. However, child abuse and neglect have existed all over the world and for many centuries.
In many cultures, deformed children were neglected and hidden away from public view. This practice still exists even today. Every culture has some form of punishment for disciplining children, but child abuse and neglect are outside the normal formal punishment.
Compare your answer with the definition given below:
Child abuse is the inflicting of, or allowing the infliction of physical or mental harm to a child under 18 years by a person who is responsible for that child or who should provide love, security, and trust. Child abuse and neglect may be in the form of non-accidental injury, emotional trauma, sexual abuse, incest, neglect, abandonment, child labour or administration of drugs or alcohol.
Child neglect means leaving a child under 18 years without the care of responsible parents or guardians.
Factors causing child abuse and neglect
Child abuse and neglect can be caused by the following factors:
- Socio economic factors
- Parental factors
- Child factors
Socio economic factors include the following:
- Poverty
- Social isolation
- Single parenthood
- Unemployment
- Poor housing
- Limited education
- Marital tensions
- Birth of child
- Relocating
Parental factors include
- Abused as a child
- Depression
- Self-indulgence and compulsiveness
- Alcoholism and drug addiction
- Inconsistent or punishment oriented discipline
- Low self-esteem
- Wife beating
- Wife rape
- Unplanned parenthood
- Single parent
- Teenage parenthood
- Dependency on the child for emotional support
- Expecting a child to behave like an adult and obey immediately
Child Factors include:
- Prematurity,
- Low birth weight
- Mental retardation
- Physical handicap
- Illegitimacy
- Difficult temperament
- Difficult pregnancy, labour, and delivery
- Separation from the mother in neonatal period
Rights of the Child
In Unit 1 we defined a child and child rights. Can you remember what we said? We said that a child in Kenya is any person below the age of 18 years. Child’s rights mean the basic things to which the child is entitled to in order to be able to grow and develop normally.
In Kenya, the rights of children have been specified in the Child’s Act 2000.
Before you proceed do the following activity.
Compare what you have written with the following basic rights of children in Kenya:
- A child in Kenya has survival rights. Rights to live with the parents. A child must be provided with adequate living standards, access to medical care, clean water, immunisation, given proper food, clothing, and a home by his/her parents, guardians or custodians.
- A child has development rights. That is rights to be educated and guided (to be shown the proper way to behave), access to play, leisure, and cultural activities. A child must have right to freedom of thought, conscience and religion.
- A child has the right to be protected from all forms of exploitation, violence and cruelty, arbitrary separation from family and abuses in criminal justice system. A child is to be protected from any mistreatment and any behaviour that might show a lack of care or interest in the child.
- A child has the right to be protected from any form of discrimination, defined as different treatment because of his/her sex, religion, cultural or social background.
- A child has the right to be protected from any social or customary practices that are dangerous to the child’s health.
- A child has the right not to be made to work or take part in any activity, whether for pay or not, which is likely to injure the child’s health, education, mental, physical or moral development. For example, all children have to help out in household work, but they must do so according to their age and ability.
- The parents of a child with a disability (such as the deaf, dumb, lame or blind) have the duty to have the child examined to find out the type and extent of the disability as early as possible. The child shall then be treated and given facilities to help him/her live as normal a life as is possible.
FORMS OF CHILD ABUSE AND NEGLECT
| 11
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
The common types of child abuse and neglect in our communities include the following:
- Physical abuse
- Child neglect and abuse
- Sexual abuse and incest
- Emotional or psychological abuse.
1. Physical abuse:
Physical abuse is the easiest to recognise. It is also a form of child abuse that has become very common in our society. Very often, physical abuse occurs in the context of other types of family violence (sexual abuses, wife beating, and spousal rape). Physical abuse was in the past referred to in medical terminology as the “battered-child syndrome” or the “battered-baby syndrome” and the resulting injuries are considered to be non-accidental. The term child abuse is now preferred because many of the abused patients are not babies. The victims are most commonly infants and pre-school children. They are defenceless, extremely demanding of their parents and guardians and are not able to express their wishes and fears.
What are the Risk factors for child abuse and neglect? Child abuse and neglect results from an interaction of the following social, environmental, parental and child factors. Let us look at each in turn starting with socio environmental factors.
Socio-environmental factors:
- Poverty
- Social isolation
- Single parenthood
- Unemployment
- Poor housing
- Limited education
- Marital tensions
- Birth of a child
- Relocating
Parental factors include the following:
- Abused as a child
- Depression
- Self indulgence and impulsion
- Alcoholism/drug addiction
- Inconsistent or punishment oriented discipline
- Low self-esteem
- Wife beating
- Wife rape
- Unplanned parenthood
- Single parent
- Teenage parenthood
- Dependency on the child for emotional support
- Expectations of adult behaviour and immediate obedience from the child
Child factors:
- Being born prematurely
- Being mentally retarded
- Being physically handicapped
- Being illegitimate
- Having a difficult temperament (restlessness, continuously crying and sleeplessness
- Difficult pregnancy and delivery
- Physically unattractive
- Separation from the mother during the neonatal period
- Unwanted child
An unwanted newborn of a single parent has the highest risk of being battered by the mother who, because of guilt and shame, has no desire to keep the baby. Some babies are killed, dropped into a latrine, left in the bush, abandoned or even buried alive. Injuries inflicted on a battered child range from mild to severe. They include burns, cuts, bruises, lacerations, fractures and bites. The injuries often occur in unusual places such as on the back, on the buttocks, or on the face as well as on more obvious places like the limbs, abdomen or head. Abused children may also show evidence of physical neglect such as malnutrition, filthy clothes or diapers, chronic diaper rash or not being immunized. Multiple fractures may be present. No bone or organ is immune to battering. Brain injuries and rupture of internal organs such as the spleen and liver may occur and may result in death in severe cases. A young baby may have injuries on the hands and feet that are swollen and bruised. The guardian may have beaten them repeatedly with a blunt object. Cases are known to occur in which a child is severely scalded with hot water or burned severely when his hand is held over a charcoal flame or burned with a hot flat iron. Some parents, usually fathers, use lighted cigarettes or heated car cigarette lighters to burn a child or whip a child with his belt, buckle, electrical cables etc. Most parents and guardians who abuse the children will deny it. Therefore, to recognise child abuse, you need to have a high index of suspicion and distinguish genuine accidental injuries from child abuse.
You need to obtain history from:
- The child if he/she is big enough to give history, but do so in the absence of the battering individual;
- Neighbours who may recall how on several occasions the child has cried while being battered. The neighbours, too, may know whether the parent or guardian is alcoholic or mentally ill or behaves abnormally.
You should suspect physical abuse if the injury is unexplained, implausible, incompatible with the history or with the child’s development, if there is delay in seeking treatment and if there is history of past injuries. Injuries which are bilateral, symmetrical, geometric, of various ages or types, or in relatively well protected parts should also raise the suspicion of physical abuse. Most intracranial injuries in the first year of life are due to physical abuse. The intracranial injuries may present as coma, convulsions, apnoea (suddenly stopping to breathe) and increased intracranial pressure.
The long term effects of child abuse include low self-esteem, lack of trust, anxiety and poor peer relationship and predisposition to abuse one’s children.
|
Suspect physical abuse if the injury is unexplained, implausible, incompatible with the history or child’s development or if there was delay in seeking treatment.
|
Management of Physical Abuse
Management should be directed towards three factors:
- The child
- The abusing individual
- The environment.
The abused child should be removed and separated from the abusing parent or guardian. Staying together exposes the child to further abuse. Subsequent injuries tend to be more severe and even fatal.
The abused child should be admitted to a health facility where assessment and treatment of the injuries can be carried out. The children are often malnourished and anaemic, so nutritional and psychiatric assessment should be carried out. It is also important to measure their haemoglobin levels. . After management of the child’s acute condition, he/she should be discharged to a foster home until the parents have been evaluated and treated.
Emotional and psychological support for the family is always much needed but should be given by skilled counsellors. Tolerance should be exercised while dealing with the abusive adult. They should be treated courteously with the maintenance of a helpful hand.
2. Child Neglect and Abuse
Child neglect is failing to provide the proper care that a child should get from the parents or guardians for optimum growth and development. Child abandonment is leaving the child completely without any care the child should get from the parents or guardians. A major cause of child abuse, neglect and abandonment is the breakdown of the extended family. Other factors contributing to child neglect and abuse are:
- Poverty of the parents
- Unmet social and economic needs of the family
- Social isolation
- Being one of the twins
- Marked prematurity
- Being a fostered or adopted child
- Being a step child
- Single parenthood
- Unplanned parenthood or teenage parenthood
- Mental handicap of the child
- Physical handicap of the child
- Mothers with psychiatric illness (depression, anxiety, hostility)
- Mother’s imprisonment with children being left unattended
- Drug abuse
- Alcoholism
- Broken families
- Parent having been abused as a child
- Unrealistically expecting the child to behave like an adult
- Stress relationship in the family
- Parent’s personal serious conflict
An increasing number of teenage mothers are abandoning their newborn babies in maternity units. The teenage mothers are emotionally immature and have no means of rearing their babies. Some of them drop their babies into the pit latrines, dustbins, bush, while others kill them outright.
Unfortunately, an increasing number of abandoned newborns have HIV infection and hence there is resistance to their admission to institutions caring for orphans. Nobody is interested in adopting them. The abandoned children are poorly nourished and unhealthy. They have emotional and psychological disturbances. Many have gone for several days without food.
Some neglected children try to meet their needs by becoming street children, stealing or offering child labour. They are at high risk of being molested sexually by adults who take advantage of them.
Since neglecting and abusing parents do not complain, it is therefore very important for you and social workers who deal with the problems of neglected and abandoned children, to understand their needs foremost and show attitudes of caring and emotional support.
Abandoned and neglected children should be given shelter and food and be made to feel wanted. The child should be checked for malnutrition and other diseases and treated appropriately.
Sexual abuse and incest
Sexual abuse is any activity with a child, before the age of consent, for sexual gratification of an adult or significantly older child or sibling. Most victims are girls who range from infants of only a few months to adolescents close to the age of consent at 15 years. Sexual abuse may be a single episode or repeated over a period of time. Sexual abuse is often accompanied by violence, coercion (force), or threat to kill or hurt the child should the incident be revealed. In most cases the child and mother are so horrified by the act that they may not gather courage to report it; so only a few cases come to light.
Sexual abuse takes the form of rape, defilement, incest, sodomy, assault or violation, prostitution, use of children in pornography, exhibitionism, and genital fondling. The offender may be an apparently normal individual or someone with a psychiatric disorder. The offence usually takes place in the child’s or in the home of the offender. The offender is most commonly a male. This male is usually known by the child and has free access to the child. In a majority of the cases the offender has been found to be either a parent, relative, neighbour, baby sitter, mother’s boyfriend or family friend. Sexual attacks are less commonly inflicted by a stranger totally unknown to the child. Up to 50% of the offenders drink excessively or are alcoholic. Incest is the most common form of sexual abuse. Very often, it is not reported because girls fear revealing it. Girls fear revealing incest because they fear they may not be believed, will be blamed, will be punished, father will be imprisoned and the family will be destroyed. Even girls abused by strangers may not reveal the sexual abuse for shame, fear of retaliation by the offender or fear of punishment by the parents. It has been shown that if sexual abuse occurs before the age of sexual consciousness the child is more likely to report the matter. Children are more reluctant to confide the matter to their parents after sexual consciousness has been achieved, usually from the age of 12 years and above. Sexual abuse has very serious consequences on the child. Physical injuries range from bruises, lacerations and bleeding from the external genitalia, anus or throat, pain during urination, painful swelling of the external genitalia, vaginal or penile discharge, sexually transmitted disease, urinary tract infection, infection of the rectum, to severe tearing of the external genitalia. The more severe injuries may be fatal. The majority of the victims have no physical signs of sexual abuse. The adolescent may become pregnant. There are also permanent and devastating emotional (psychological) effects. The type of emotional (psychological) effect depends on the age of the child and developmental stage of the child. An infant or toddler manifests sleep disturbances, irritability and feeding difficulties. The older child develops anxiety, withdrawal, school phobia, selective mutism, depression, nightmares and problem in peer relationships, regression (with enuresis, encopresis, clingingness, temper tantrums), aggression, running away, promiscuity, drug abuse, suicide attempt, difficulty in sexual adjustment, preoccupation with sexual matters, homosexuality, interpersonal problems, low self-esteem, vulnerability to child sexual abuse, and other behaviour problems listed in the section on emotional abuse. Because of fear of disclosing the problem, or if the victim feels powerless to prevent the abuse, many cases are discovered only after the act has been repeated several times.
Management of sexual abuse victim This involves the following:
- Prompt surgical repair of any injuries remembering that the more extensive injuries may require several stages of operations;
- Looking for sexually transmitted diseases as they need prompt treatment and administering prophylactic antiretroviral drugs;
- Intensive counselling and giving emotional support;
- Psychiatric and social rehabilitation and very careful assessment before returning to normal society;
- Giving prolonged follow- up;
- Ensuring that the child does not appear in court proceedings during the recovery time.
Emotional or psychological abuse
Emotional or psychological abuse is intentional deprivation of the emotional support that a child needs for normal emotional development. An emotionally abused child is denied love, acceptance, security, recognition and praise for good behaviour in play or learning, encouragement, loving discipline, stimulation and opportunities for learning and developing independence. A parent can also emotionally abuse the child by teasing, belittling, verbal attacks, rejection, fear inducing language or behaviour, scolding, discouragement, criticism, comments about shortcomings and appearance, threats of punishment or desertion and by not allowing establishment of relationships outside the family.
Manifestations of emotional abuse and neglect are both physical and emotional.
The physical manifestations of emotional abuse include failure to thrive, bed wetting, sleep disorder, encopresis, voracious appetite, feeding disorder (early rumination), crying spasms, temper tantrums and self stimulatory behaviours (biting, rocking, sucking fingers etc).
The emotional signs of emotional abused children include the following:
- self-destructive behaviour, e.g. attempted suicide, running away, promiscuity;
- Apathy, withdrawal, depression;
- Academic failure;
- Emotional and intellectual developmental delay and regression (thumb sucking, bed wetting, demanding to be fed, talking like a baby, asking to be carried like a baby, aggression, being quarrelsome, destructiveness and negativism);
- Hyperactivity, temper tantrums, conduct disorder;
- Pseudomaturity;
- Lack of trust;
- Rigid, compulsive and disorganized behaviour;
- Low self-esteem and feelings of inadequacy;
- Role reversal (the child takes care of the parent);
- Poor peer relationship or peer dependence;
- Unusual fearfulness and hyper alertness;
- Lack of creativity;
- Excessive fantasy;
- Lack of familial attachment;
- Gender confusion;
- Lack of empathy;
- Excessive anxiety and night terrors;
- bliviousness to hazards and risks;
- Stuttering.
Diagnosis
Observing the above signs is essential for recognition of emotional abuse. Careful questioning and a high index of suspicion will facilitate the diagnosis
Management of emotional abuse.
This involves:
- Identifying the source of the problem in order to be able to give the help the child desperately needs;
- Counselling and supporting the parents;
- Family therapy and support. This aims at enhancing the mental health of the whole family and is key to prevention.
The children who are most vulnerable to abuse and neglect are those born into family environments where the stress level is high. Typically, they are:
- Children born to parents or guardians who stay in stressful environments where they lack support;
- Children of unemployed, poor parents;
- Children belonging to single parents or those who stay with step parents;
- Children living with divorced, alcoholic, drug-addicted or parents/guardians who suffer psychiatric illness.
Quite often the abusing and neglecting individual did not have a normal childhood upbringing and may have been battered him or herself during childhood. That is to say battering begets battering.
You, the health worker, have a very important role to play in reducing the problem of child abuse and neglect.
Prevention of child abuse and neglect
| 12
What role can you play in preventing child abuse and neglect? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
As a health worker, you have the responsibility to help reduce child abuse and neglect. You should:
- Inform authorised officers, such as probation and social workers, about cases of child abuse, neglect and abandonment;
- Advise the child’s parents on how to make the situation better;
- Work together with the parents or guardians of the child in planning for the future of the child;
- Take any necessary steps to reduce or stop harm to a child;
- Provide medical care where warranted;
- Carry out family counselling;
- Create awareness among communities about dangers of child abuse and neglect.
THE ROLE OF THE COMMUNITY IN PREVENTION AND MANAGEMENT OF CHILD ABUSE
The community has a big role to play in prevention and management of child abuse. Unfortunately, child abuse occurs in communities! NO MATTER what form of abuse, the community can join in the fight against child abuse and/or manage the cases in the following ways:
- Protecting the children, especially those vulnerable to abuse. The community is the voice to the voiceless (children);
- Contacting the relevant authorities whenever child abuse happens. The relevant authorities include local councils, medical authorities, the police, etc;
- Not leaving the children alone at home without a trusted adult person;
- Encouraging children to report any incident that occurs to them. The parents should take the initiative every evening to find out what happened to the child during the day;
- Educating children on Children’s Rights and local legal systems such as local councils, police, etc;
- Recognizing the children’s rights, and cooperating with organisations that advocate and promote children’s rights at community and national levels;
- Identifying potential abusers and instituting supportive interventions during antenatal and perinatal periods. The potential abusers, as mentioned earlier, are those who were abused as children, those with negative attitude towards the pregnancy, those with unrealistic future expectations for the child, the depressed, those with no support, single mothers, those who attempt to deny the pregnancy, those disinterested in bonding to their babies and those concerned about the sex of the baby. The potential abuser should be counselled and instructed on effective child rearing, needs of the child, normal development and care of the baby. Bonding is fostered by encouraging the mothers to hold the newborn, look at the newborn, care for the newborn and promoting the parent’s self-esteem.
SUMMARY
Congratulations! You have now come to the end of this Unit. In this unit we looked at common mental health conditions in children. We saw that early detection and treatment, good antenatal and postnatal care, counselling, health education and diligent care of our children can prevent many of these conditions. Remember to refer all the conditions that you are not able to manage to a specialist. Children are the leaders of tomorrow so let’s take good care of their mental health.
Well, you can now take a well deserved break before you complete the attached tutor marked assignments.
Good Luck!
Assignment
|
DIRECTORATE OF LEARNING SYSTEMS DISTANCE EDUCATION COURSES
Student Number: ________________________________ Name: _________________________________________ Address: _______________________________________ _______________________________________________
CHILD HEALTH COURSE Unit 17: Assignment Children’s Mental Health Problems
Instructions: Answer all the questions in this assignment. 1. How would you identify a child who is mentally retarded? _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
3. List five factors that influence child abandonment. _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
_____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________ _____________________________________________________________________
|
Once you complete this assignment, post or bring it in person to AMREF Training Centre. We will mark it and return it to you with comments.
Our address is as follows:
Directorate of Learning Systems
AMREF Headquarters
P O Box 27691-00506
Nairobi, Kenya
Email: amreftraining@amrefhq.org