Lesson 15: Intestinal Helminths
Contents
UNIT 15: HELMINTHIASIS
INTRODUCTION
Welcome to this unit on Helminthiasis. These are parasitic worms of various types which live in a child’s body where they cause ill health.
They are of two types:
- Those that infest the child’s intestines and are called intestinal helminths
- Those that infest the child’s tissues and organs and can be referred to as tissue or visceral helminths
Young children are particularly affected by Intestinal helminths. Poor sanitation and failure to use a latrine increases the spread of these worms. It is therefore important for you to know how the worms are spread and their effects on child health so that you can manage and prevent them effectively.
|
By the end of this unit, you should be able to:
|
15.1: COMMON HELMINTHIC WORMS
The common helminthic worms in Kenya can be divided into two categories:
- Intestinal worms;
- Tissue/visceral helminths.
Intestinal helminths include the following:
- Ascaris lumbricoides
- Strongyloids stercolaris
- Enterobias vermicularis
- Trichuris trichura
- Ankylostoma duodenale
- Necator americanus
- Taenia saginata
- Taenia solium
The tissue or visceral helminths include:
- Filaria
- Hydatid
- Schistosome
- Kala-azar
Life Cycle of Helminths
A life cycle is a description of the various stages a given worm goes through from the time of infection to the time of maturation. Each type of worm has a different life cycle. Knowledge of this life cycle is important as it will enable you to identify the appropriate treatment and preventive measures for each worm.
In this unit we shall start our discussion of helminthiasis with intestinal helminths and then move on to tissue or visceral helminths.
15.2: INTESTINAL HELMINTHS
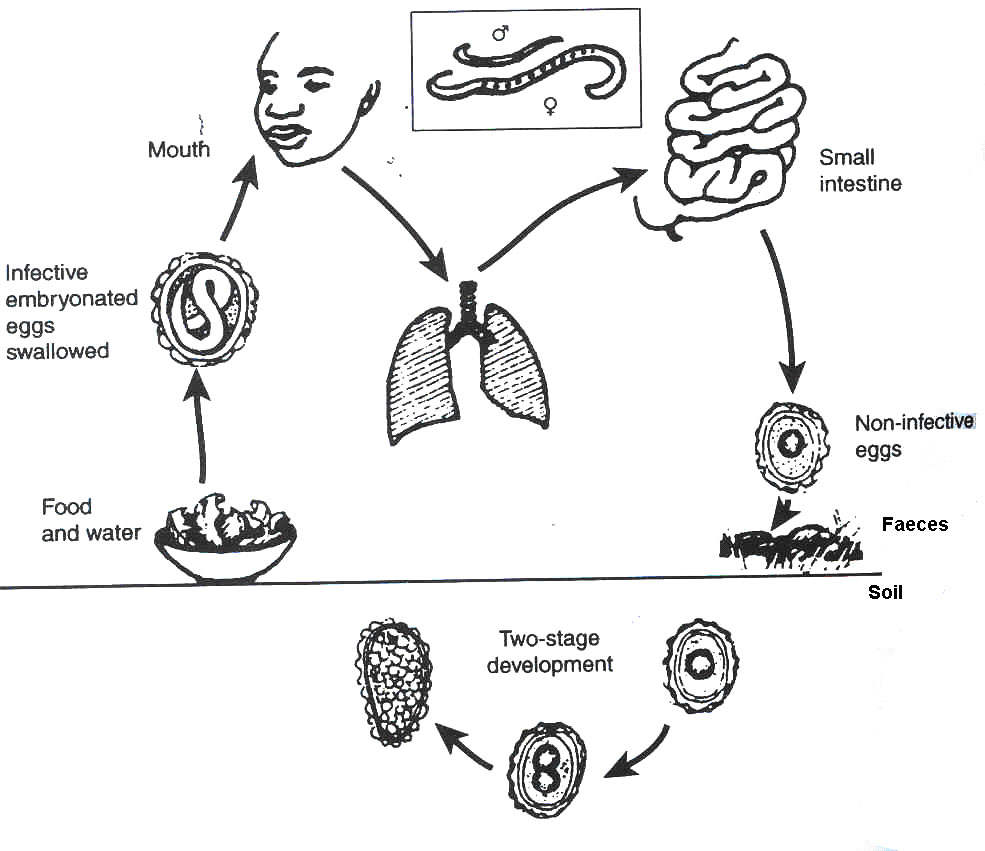
a) ROUNDWORM (Ascaris lumbricoides)
Ascaris lumbricoides is one of the most common of the intestinal worms. It is a roundworm and infection with it is called Ascariasis. Children are more frequently and more heavily infected than adults because of their habit of putting all kinds of things into their mouths. If these objects are contaminated with ascaris eggs from human faeces the children swallow the eggs and thus become infected.
The round worm lives in the small intestines. The female lays as many as 200,000 eggs a day. These are passed in stool and develop in the soil. They are then transmitted as follows:
- Eggs passed out in stool are embryonated in stool before they are infective.
- The embryonated eggs are carried away from the contaminated place into houses by feet, foot wear or in dust by wind. They also can reach vegetables and fruits
- A child then eats and swallows food or fruits contaminated with eggs.
- The eggs hatch into larva in the intestinal canal.
- The larva penetrates the intestinal wall and reach the liver via the portal system.
- The larva is then carried to the lungs.
- In the lungs, they penetrate into the airway and pass via the bronchioli, bronchi, and trachea to the pharynx.
- They are coughed up and are swallowed a second time, thus returning to the intestinal tract.
- They then settle into the jejunum where they develop.
- In two months, they mature as adult worms and can live for about a year.
Fig. 15.1: Life Cycle of Ascaris lumbricoides
Before you read on, do the following activity. It should take you 5 minutes to complete.
| 2
Some children with roundworms have been brought to you in your health facility. What are their symptoms? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… …………………………………………………………………………………………………………
|
Signs and Symptoms Usually, children with mild infestation are symptomless. They may, however, present with symptoms indicative of larval migration like pneumonitis or urticarial rash. There may be some vague abdominal discomfort. Sometimes a worm may leave the body through vomitus or stool.
Complications In heavy infections, complications may occur. I will briefly describe them here:
- Intestinal obstruction: This is a serious complication of heavy roundworm infestation. A ball of worms forms, usually at the narrowest part of the intestine (the ileocaccal junction) where the small intestine enters into the large intestine. The child is ill with abdominal pains, constipation, vomiting, abdominal distension and an abdominal mass. If the obstruction is complete the child is not passing gas or stool at all, urgent surgery is needed and you should refer the child to hospital urgently.
- Wandering of the worms: Wandering ascaris may reach abnormal foci and cause acute symptoms. Vomiting of the worm may course swelling of the glottis and larynx. This results in difficulty in breathing. Blockage of the bile ducts may cause obstructive jaundice and migration into the liver may result in liver abscess.
- Malnutrition: Ascariasis contributes to serious malnutritional states such as stunting, kwashiorkor and Vitamin A deficiency. The adult worms absorb the child’s digested food in small intestines. The worms also interfere with the absorption of nutrients in the small intestine thus causing malnutrition.
Diagnosis If you work in a unit with laboratory facilities then you should request a microscopic examination of the stool. A characteristic ovum is seen under microscope on stool preparation.
You can also make a diagnosis of ascariasis when:
- The caretaker tells you the child has passed the worm in stool or vomited it.
- You are able to see the worm in a child's stool or vomitus.
Treatment
A child with ascariasis should be treated as follows:
- A child who is aged 2 years or more can be given albendazole 400 mg of mebendazole 500 mg single dose.
- A child aged less than 2 years should receive half that dose.
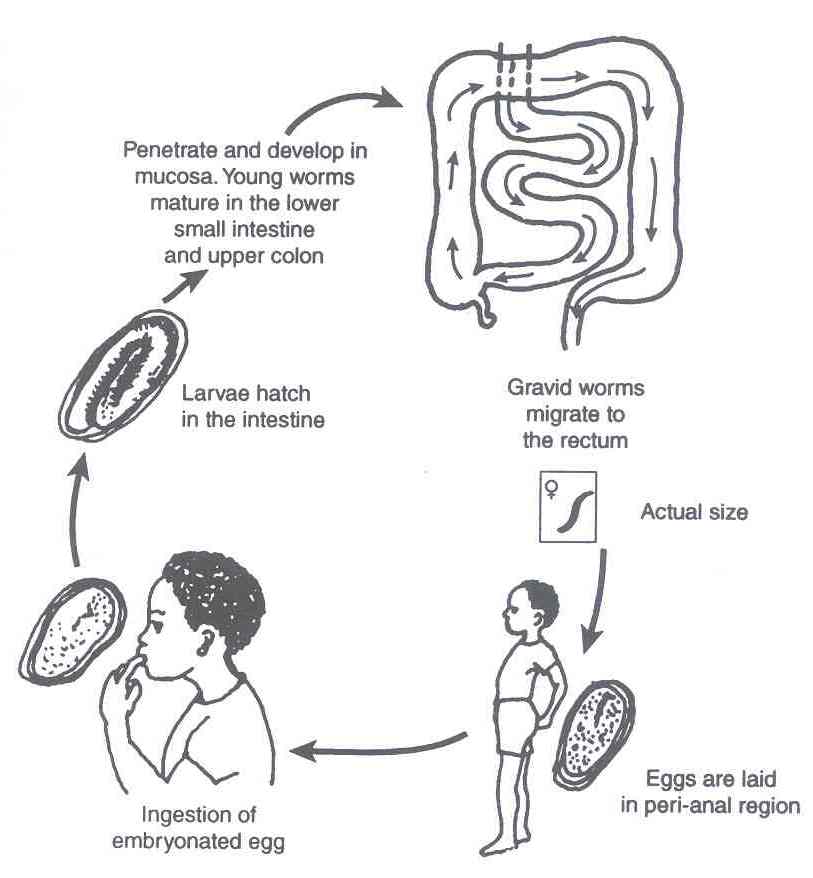
b). PINWORM OR THREADWORMS (Enterobius vermicularis)
Infestation with Enterobius vermicularis is called enterobiasis. The worm is commonly known as threadworm or pinworm.
Infection with Enterobius vermicularis occurs by the faecal oral route. It is transmitted as follows:
- An infected child passes out stool containing embryonated eggs.
- A child ingests (eats) food contaminated with the embryonated eggs.
- The larvae hatch in the intestines.
- The larvae penetrate and develop in the mucosa. Young worms mature in the lower small intestines and upper colon.
- The grown worms migrate to the rectum, especially at night, to discharge eggs on the perianal skin.
You should now study the illustration provided in Fig. 15.2 to appreciate the lifecycle of the pinworm.
Fig. 15.2: The Life Cycle and Transmission of Pinworm
Signs and Symptoms
A child with Enterobiasis will present with a history of severe pruritus ani. In the child's perianal region you will see excoriation and secondary bacterial infection. This is as a result of intense scratching of the area. You will be told of other symptoms like sleep disturbances, restlessness, loss of appetite and weight loss. In female children, vulvitis may also occur.
Diagnosis You can diagnosis Enterobiasis by seeing the worms in the stool. Pick up the eggs by sticky tape (cellotape) placed on the perianal skin in the early morning. You can also diagnose on the basis of a history of itching and scratching of the perianal region.
Treatment The treatment of Enterobius is similar to that of Ascariasis. You should treat with Albendazole or Mebendazole in the doses stated earlier. You should give the same dose to each child of the family. An alternative treatment that can be given is Piperazine (antepar) 75 mg kg/day for a week.
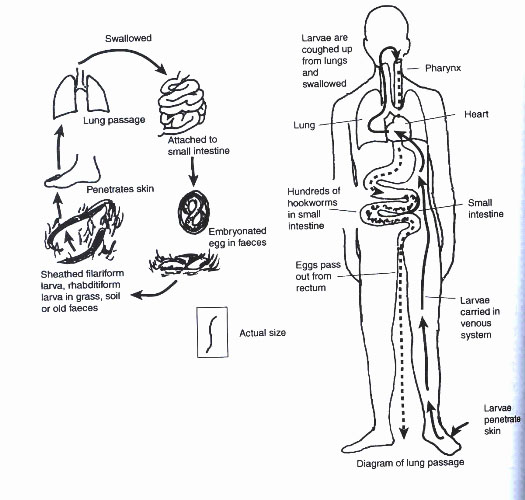
c) HOOKWORM (Ankylostoma duodenale/Necator americanus)
Infection with hookworm varies from symptomless to a chronic debilitating disease with a variety of symptoms. This depends on a number of factors:
- The extent of the infection i.e. worm load.
- The nutritional state of the child and
- The degree of anaemia
Hookworm anaemia is one of the most important causes of anaemia in children.
Epidemiology
There are two types of hookworms:
- Necator americanus;
- Ankylostoma duodenale.
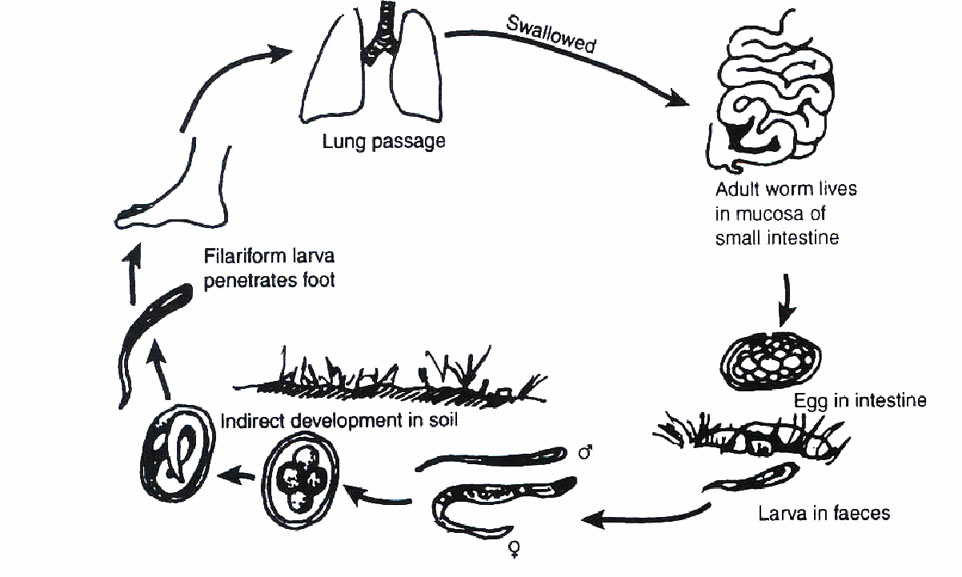
The adult worms live in the upper part of the small intestine. Their heads are attached to the wall of the intestine by hooks. The transmission of hookworms is as follows
- The hookworm eggs are passed in the faeces already embroyonated;
- If the faeces are left in warm moist surroundings they develop into larvae.
- The larvae leave the faeces and bury themselves in moist damp soil;
- When the larvae comes into contact with human skin it attaches itself and penetrates actively through the skin;
- The larvae pass via the lymphatic system and blood stream to the lungs.
- The larvae then migrate up the trachea and are swallowed a second time. They reach the small intestines where they grow to be adults.
Fig. 15.3: The Life Cycle and Transmission the Hookworm
Signs and Symptoms
A few hookworms in a well nourished child do not cause any sickness as the small amount of blood loss can be replaced. However the child may have:
- Temporary cough and wheezing as a result of the larvae passing through the lungs.
- Chronic anaemia caused by a heavy infestation which suck blood from the intestine where adult worms live hooked onto the intestinal wall.
The degree of anaemia depends on the child’s nutrition and the number of worms present. A child with severe anaemia will have tiredness, pallor, and swelling (oedema). Breathlessness and heart failure may develop.
Diagnosis
If you work in a health unit with laboratory facilities you should request a microscopic examination of stool. Characteristic hookworm eggs will be identified in stool prerparation. You can also suspect hookworm if a blood specimen is taken for examination and a child is found to have chronic anaemia (Hb less than 10g/dl). Also, microcytic (small red cell) and hypochronic red cells with low pigmentation are peripheral blood picture of iron deficiency caused by hookworms,
Treatment
As you have discovered in your clinical practice, a child with hookworm infestation may have iron deficiency anaemia and the worms themselves. You therefore need to de-worm the child and then treat for anaemia.
- Deworming: Use Albendazole or Mebendazole in the doses described for ascaris. Can you remember the dosage? Check if you have forgotten. Remember that children who are below 2 years should receive half the dose.
- Levamisole Tablets 3mg/kg as a single dose may also be used.
You must also treat the iron deficiency anaemia. Give iron orally:
- For 1 to 5 years of age: Ferrous Sulphate Tablets 100 mg (1/2 tablet) every 12 hours for 2 months.
- For children older than 5 years of age: Ferrous Sulphate Tablets 200 mg every 12 hours for 2 months.
Treating Malnutrition:
The associated malnutrition should be treated by advising the caretaker to feed the baby on locally available high protein energy foods. You will learn more about these foods in the nutrition unit.
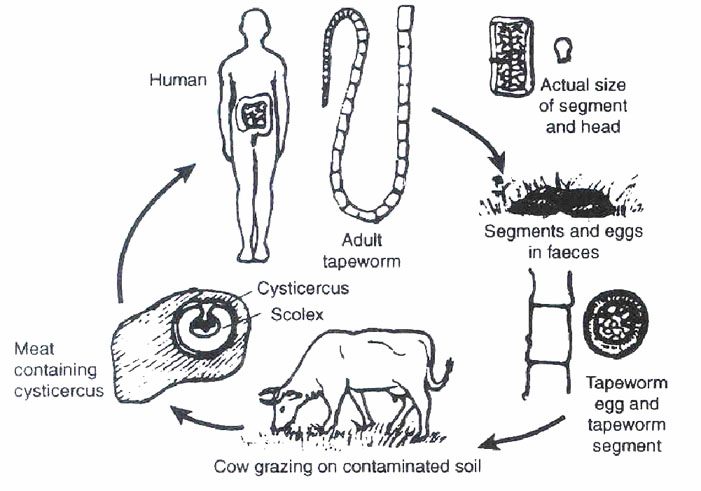
d) TAPEWORM (Taenia saginata and Taenia solium)
Tapeworm infestation is caused by two worms called Taenia saginata and Taenia solium. The infestation is referred to as Taenasis. Tapeworm infestation is common in areas where beef and pork is eaten raw or undercooked.
Life Cycle
Let us now learn about how one can get infested with tape worm. Study the illustration in Fig. 15.4 and the descriptive notes below. The life cycle of the tapeworm begins with an infected person and is transmitted as follows:
- Stool containing grand segment of the worm or eggs is passed;
- Cattle or pigs ingest the eggs or segments;
- In the gastrointestinal tract of the animals, the embryos hatch and penetrate the bowel wall;
- The larvae are then carried via the blood stream to striated muscles;
- In the muscle, the larvae grow and form the infective cysts called cysticerci. Pork or beef containing these cysts is called "mealy" pork or beef;
- When a child ingests lightly cooked meat containing cysticerca, the cysts are dissolved by the gastric acid in the stomach and the embryo is release;
- Taenia saginata embryo attaches itself to the wall of the small bowel by its head and grows into an adult worm;
- Taenia solium behaves differently by penetrating the intestinal wall. It is then carried by the blood stream to striated muscles or the brain.
Fig. 15.4: The Life Cycle and Transmission of Taenia saginata
Signs and Symptoms
Most infections with Taenia saginata cause no signs or symptoms. In some children there is a loss of weight, abdominal discomfort and pruritus ani.
A child with Taenia solum infection may present with neurological signs like epilepsy, or muscular pains. This is because the cysticerca invade the brain or muscle respectively.
Diagnosis
You can diagnose tapeworm infestation when you are given a history of the presence of segments in the stool. The segments can migrate out through the anus and be found on the buttocks or they are passed with the faeces.
Treatment
The drug of choice in the treatment of tapeworm infestation is Niclosamide. You should give it according to the schedule in Table 15.1.
Table 15.1: Niclosamide Treatment for Tapeworm
| Age | Dose | Duration |
|---|---|---|
| < 2 years | 500 mg as a single dose | 1 day |
| 2-6 years | 1 gm as a single dose | 1 day |
| > 6 years | 2 gm as a single dose | 1 day |
When administering the drug Niclosamide, you should take note of the following:
- It is better to give Niclosamide at breakfast and the tablets should be chewed.
- Two hours after administering Niclosamide, give a purgative like Bisacodyl (5mg/tablet) to the child.
An alternative treatment is mebendazole tablets as described in the treatment for Ascaris.
e) STRONGYLOIDIASIS (Strongyloides stercoralis)
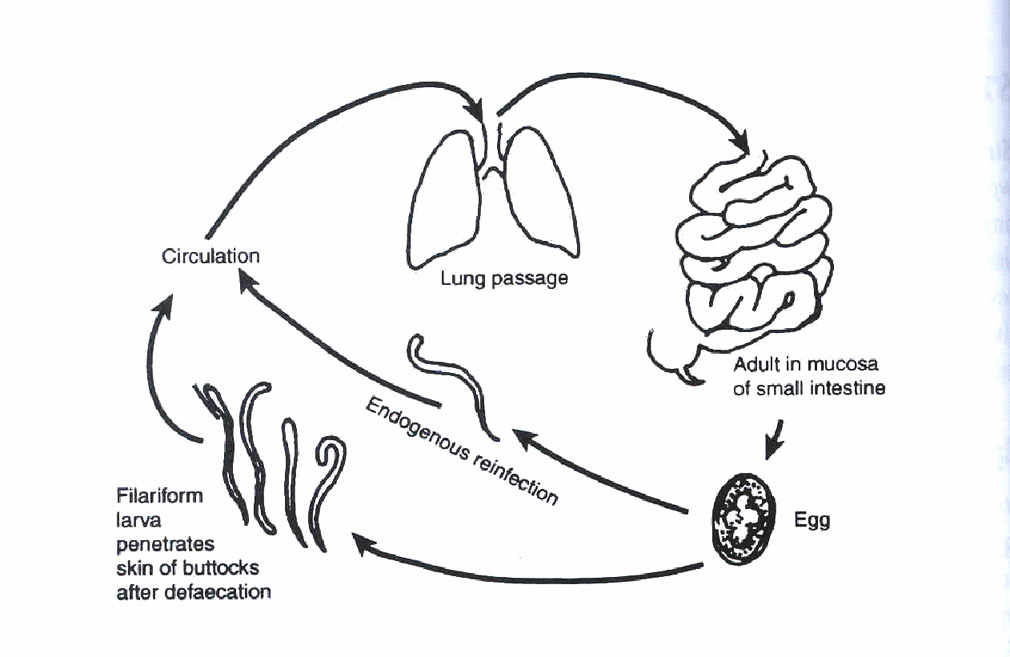
Strongyloides stercoralis is an intestinal worm. The adult worm lives in the mucosa of the duodenum and jejunum. Infection with Strongyloides stercoralis is called strongyloidiasis. Most infections are without symptoms an signs and are usually not very severe. However, extremely heavy infections may result in death, especially among patients with AIDS or after immunosuppressive drugs.
Life Cycle
Study the illustration given in Fig. 15.5 and the notes that follow to learn about the life cycle and transmission of Strongyloides stercolaris. The life cycle begins with an infected person:
- An infected person passes out faeces containing larva;
- The larvae may either develop into free living adults which continue to reproduce outside the body, or they may develop into infective filariform larvae which penetrate the skin.
- The rest of the cycle is similar to hookworm infection.
Fig. 15.5: The Life Cycle and Transmission of Strongyloides stercoralis
From the above description you must have noted that there is a chance of the larva developing directly into the infective stage. Because of this, re-infection is common. Even within the bowel, the larvae may become infective and penetrate the bowel wall. This is called endogenous re-infection. This is illustrated in Fig. 15.6. You should take a look at it now (next page).
Fig. 15.6: Auto-re-infection Cycle for Strongyloides stercoralis
Signs and Symptoms:
A child with mild infection of stronglyloides stercoralis is symptomless. If the infection is heavy, the child presents with the following:
- Diarrhoea and malabsorption. This is because the worms interfere with the normal functioning of the bowel;
- Urticaria and other hypersenstivity reactions. This is as a result of the continuous re-infection.
Diagnosis
If you have a laboratory facility in your health unit, then you can make a diagnosis by identifying the characteristic larvae in a fresh stool specimen. If you do not have a laboratory facility, then suspect strongyloidiasis from the history given and the clinical presentation.
Treatment
The drugs for the treatment of a child with strongyloidiasis are Albendazole and mebendazole. You should give it in the same doses as we outlined for the treatment of Ascariasis. To remind yourself do the following activity.
| 6
Indicate how you would prescribe mebendazole for children with strongyloidiasis in the table below:
…………………………………………………………………………………………………………………………………………………………………………………………………………………… >2 years Age Dose Duration ……………………………………………………………………………………………………………………………………………………………………………………………………………………
|
Compare your answer with the treatment we discussed earlier for Ascariasis.
f) WHIPWORM (Trichuris trichura)
Infection with Trichuris trichura is called Trichuriasis. The adult worm is commonly known as the whipworm, as it looks like a whip. It lives in the large intestines and is common in hot and humid climates.
Infection with whipworms occurs in a very similar war to those of ascariasis. The embryonated eggs are ingested and then hatch. The mature worms attach themselves to the mucosa of the caecum and colon. This worm does not have a lung passage phase.
| 7
We have briefly described the life cycle of the whipworm. Now draw an illustration of its life cycle on a separate piece of paper. When you finish compare your illustration with that of the life cycle of Ascaris lumbricoides worm. Yours should be similar, the only difference being the absence of the stage of lung passage.
|
Signs and Symptoms
Mild infections with Trichuris trichura are symptomless. A child with heavy infection will have the following:
- Abdominal discomfort
- Bloody diarrhoea
- Loss of weight
- Anaemia
- Prolapse of the rectum especially in malnourished children (A reddish mass protruding from the anus).
Diagnosis
If you work in a unit with a laboratory facility then request a stool examination. Diagnose trichuriasis when barrel-shaped eggs are found in stool. You should also suspect trichuriasis in children who present with rectal prolapse ( a mass protruding from the anus).
Treatment
The treatment of trichuriasis is similar to that of Ascariasis.
The prolapse of rectum needs to be treated when it occurs. To reduce the prolapse you wear gloves and gently push the mass up the rectum using a moist cloth.
- Strap the buttocks together with plaster;
- Treat diarrhoea;
- Improve the child’s diet to improve nutrition
In mild infections, you may not need to give a child any treatment.
As we mentioned at the beginning of this unit, there are two types of helminths: intestinal and visceral helminths. So far we have discussed intestinal helminths. Next, let us look at visceral helminths.
15.3 VISCERAL (TISSUE) HELMINTHIASIS
Visceral helminths are human parasites which live in the body tissues and organs (viscera) where they cause ill health to children. They include the following:
- Filaria
- Hydatid
- Schistosomes
- Kala azar
Let us discuss each in turn.
1. FILARIASIS
Filariasis is a group of diseases caused by nematode worms of different species. In Africa three common types of filarial worms are Wuchereria brancrofti, Ochocerco volvulus and Loa Loa. These worms infect the lymphatic system and lymph nodes of humans where they cause inflammation or lymphangitis and swelling of lymph nodes also known as lymphatedenopathy with its characteristic lesions. Filariasis is transmitted by mosquitoes.
Life Cycle
Generally the life cycle of these filarial nematode worms is similar. When a mosquito or fly carrying microfilarial larvae bites a new host, it deposits larvae into the subcutaneious tissue of the host. The larvae find their way into the lymph vessels where they take about a year to mature. The mature adult female produces larvae called microfilariae. These escape from the lymphatics to reach blood circulation. It is from here where mosquitoes biting the infected person ingest them. The ingested microfilaria develop in the mosquitoes to reach infective stage of microfilariae transmit them to the next human victim when they bite him. This is similar to the transmission of malaria parasites. The injected larvae migrate from blood stream into the lympatics thus completing the life cycle; when they mature into adult filarial worms
Microfilariae appear in plenty in blood circulation at distinct times of the day, usually in the evenings and at night. This characteristic phenomenon is referred to as periodicity and appears to be related to the biting habits of the transmitting mosquitoes.
Children infected with filarial worms develop light intensity of worms and usually have no clinical symptoms, Repeated infections increase filarial worm intensity and a child may display mild symptoms consisting of malaise, fever of varying grades and vomiting.
Diagnosis involves laboratory examination of blood smears for microfilariae . In endemic areas this is enough proof of infection. The main typical lesions of filariasis are seen in adults whose features vary by the infecting nematode as you will see in the following section. However, in all of the filarial infection there is marked eosinophilia, fleeting skin rashes, urticarial rashes and pneumonitis.
Let us briefly look at the diseases caused by the three worms which we discussed earlier.
Bancroftian Filariasis (Wuchereria brancrofti) This worm causes bancroftian filariasis which mainly affects the lymphatic system. The worms live in lymphatic system where the female worms produce microfilariae and make their way to the blood stream. The presence of the worms in the lymph vessels gives rise to a foreign-body reaction. When the worms die, more foreign proteins are released causing an even more severe reaction. This infection has three phases, an acute, subacute and chronic phase. In the acute stage is characterised by fever and lymphadenopathy and eosinphilia. The subacute phase sets in after about a year. Reactions to the adult worms cause attacks of fever with lymphangitis, funiculitis and or epididymitis. . In the chronic phase, the lymph glands and lymph vessels become obstructed thereby causing swelling of the legs or scrotum (referred to as elephantiasis). Two types of mosquitoes are involved: the Culex in urban areas and the Anopheles in the rural areas.
Fig 15.7: Filariasis of the legs
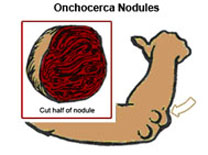
Onchocerciasis (Onchocerca Volvulus) This filarial worm causes a disease called Onchocerciasis which is endemic in West Africa, Central Africa, East Africa and Sudan. The disease is also known as river blindness. The worms cause severe lymphangitis, skin modularity and eye lesions which can cause blindness. It is transmitted by a small black fly called Simulium damnosum, which lays eggs in fast-running rivers or turbulent areas of a river.
Fig 15.8: Onchocerca nodules
Loiasis (Loa Loa)
This filarial worm cause a disease referred to as loiasis which is characterized by transient subcutaneous swelling.
Diagnosis of Filariasis
If a child from an endemic area comes with the skin lesions and eye changes we have discussed, you should suspect filariasis and order a laboratory test. Laboratory confirmation is based on peripheral blood smears as well as complement fixation test. In the chronic phase of bancroftian filariasis, a blood slide should be taken between 10.00pm and 2.00 am or 45 minutes after a provocative dose of diethylcarbamazine 100mg. The microfilariae of Onchocerca volvulus is not found in the blood. The diagnosis is made by demonstrating microfilariae in skin snips obtained from the thighs, buttocks and iliac crests. The snip is placed in normal saline, shredded and examined under a microscope for microfilariae.
Treatment
Treatment should be done early before the sclerotic skin changes and lymphatic blockage has occurred. The drug of choice is diethylcarbamazine 2 Mg/Kg body weight is given orally three times a day for a week. This drug kills the microfilariae and has also some effect on the adult worm.
Prevention and Control Prevention or control of filariasis focuses on reducing human reservoir and vector population. Treatment with diethylcarbamazine abolishes or greatly reduces circulating microfilariae and also kills adult worms in the lymphatics. Culex mosquitoes often breed in septic tanks and pit latrines in urban areas. Therefore septic tanks and latrines should be treated regularly with larvicides. In the case of onchocerciasis, recent trials have confirmed that treatment with Ivermectin given with health education on safe water use reduces the disease burden in communities. Also the continuous addition of insecticide to the water of rivers known to be breeding places for Simulium fly can help to control the disease.
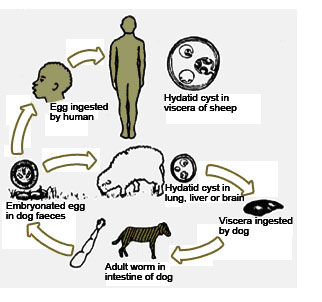
2. HYDATID DISEASE (HYDATIDOSIS)
Hydatidosis is a disease caused by the cysts of the dog tapeworm called Echinococcus granulosus. It is known as echinococcosis or hydatid disease. The adult Echinococcus is a small tape worm measuring 5mm in length and lives in small intestines of dogs. Man acquires hydatidosis when he swallows infected ova as a result of his close association with dogs. In Kenya the disease is common in Turkana where a large number of camel and goats are heavily infected with Hydatid cysts. The disease also occurs in Masailand but to a small extent as dogs there are not in close contact with children. In Masailand the domestic animals which infected are cattle and sheep. When dogs eats cow or goat meat that is infected with cysts, they get infected. The cysts develop and mature into adult tape worms in their intestine thus completing the life cycle. The dogs then pass the eggs in their faeces which are ingested by sheep, goats, and cattle. Thus the main cycle of transmission is between dogs and domestic livestock.
The Turkana tribesmen are the most heavily infected people in Kenya because of the intimate contact between children and the large number of dogs in the area. In Turkana dogs are used to clean the face and anal regions of babies due to lack of water. Because of this closeness with dogs, the infected dog faeces easily get in contact with the children’s hands. If they do not wash their hands before eating, they swallow the ova while eating their food. The swallowed ova hatch out in the intestines and the larvae invade body tissues where they develop into cysts. The cyst continues to grow in various organs of the body, most commonly the liver and the lungs. The brain is occasionally infected.
Fig 15.9: Life cycle of Echinococcus granulosus
Clinical Picture
The main clinical features are abdominal swelling due to cysts in the liver. This can lead to extreme abdominal distension. Cysts in the brain present with increasing intracranial pressure similar to intracranial neoplasm. There is evidence of chronic ill health as shoen by gross emaciation. If a child from Turkana presents with these features, you should immediately suspect hydatidosis. A chest X-ray or abdominal ultrasound investigation may be done in hospital. Other diagnostic tests include the Casoni’s test which is positive in 75% of the cases.
Treatment
The treatment of hydatidosis is both medical and surgical. Medical treatment with Albendazole is very effective. The treatment is given as 20mg/kg in divided doses (twice a day) for 30 days. This treatment gives a 20% cure rate for single cysts and less in multiple cysts. However, it can arrest the growth of the cyst and reduce its size. Surgical treatment involves the removal of easily accessible cysts from the liver, lungs and brain.
Prevention and Control The disease is prevented by:
- Hand washing, especially before feeding;
- Deworming dogs and dog control;
- Avoiding close contact with dogs;
- Disposal of all meat containing Hydatid cysts by burning or burying.
3. SCHISTOSOMIASIS (BILHARZIA)
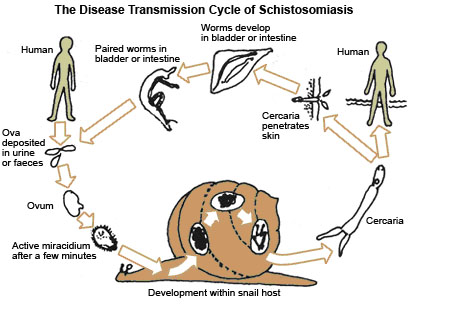
This is a chronic disease related to water use. It is known as Bilharzia after Theodor Bilharz who discovered it in Cairo in 1861. Two forms of of schistosomiasis occur in Africa. These are urinary schistosomiasis and intestinal schistosomiasis. In Kenya, intestinal schistosomiasis is the most important. It is found a long the coast and Lake Victoria regions, although there may be some other pockets of the disease in the country. In this section we shall therefore discuss intestinal schistosomiasis which is caused by schistosoma mansoni (s. mansoni).
Let’s start by reviewing its life cycle.
Life Cycle
The adult worm of S.Mansoni inhabits the veins around the colon, rectum and anus of the infected persons. Here the adult female worm lays eggs which are carried to distant parts of the body, such as, the liver, the lungs, the brain and spinal cord. The eggs penetrate the mucosa of intestines to reach the stool and are passed in stool of the infected persons.
On reaching water particularly stagnant water of swamps the eggs hatch into larval stage called miracidia. The miracidia infect snails in the water and undergo developmental stages to become cercariae. The cercariae leave the snails and swim freely in the water awaiting contact with human skin. Children playing in such water come in contact with cercariae which penetrate their skin and infect them.
After entering the host, cercariae travel in the blood stream or lymphatic system to reach the right side of the heart from where they are carried to the lungs and eventually reach the liver. In the liver, the larvae mature into adult worms. Here they mate and migrate against portal stream to reach the veins in the colon, rectum and anus and the cycle is repeated.
Fig. 15.10. Transmission of Schistosomiasis
Clinical Features The clinical features of schistosomiasis occur in relationship to the following::
- Site of entry of the parasite;
- Local site where the worms stay;
- Systematic reactions caused by the worms;
- Complications caused by either the adult worm or where the ova or eggs get deposited.
The disease progresses in three stages: invasion, maturation and established infection and late stage. Let us briefly look at each stage.
Invasion stage:
The earliest clinical feature is the itchy skin lesion at the entry of the cercariae. When the cercariae penetrates the skin, it causes dermatitis and itching reddish papules and local oedema. However, this stage is not always noticed and so it goes unreported. The stage disappears spontaneously within three days.
Maturation stage
During this stage the schistosomes mature in the liver. The clinical features include fever, eosinophilia, abdominal pain and transient generalised urticaria. When the adult worm matures it descends to the mesenteric veins in the intestinal wall. However, this stage also passes largely unnoticed.
Established infection
This is the stage of egg production. Some eggs do not penetrate the tissue and are carried with the blood stream to the liver and lungs. Other eggs penetrate tissue with the help of their spines but fail to reach the lumen of the bowel. These eggs which do not reach the lumen of the bowel provoke an inflammatory reaction and the formation of granulomas. Constitutional systemic features follow which include: debility, indigestion, poor appetite, and tiredness, headache and weight loss. An irritating dry cough also occurs in some patients. Whose chest x-ray show miliary mottling or patchy lesions in both lungs which may be mistaken for tuberculosis, or pneumonia. Blood counts or this stage showing marked oesinophilia. Fever is common at this stage of the illness. The fever is usually mild to moderate but continuous and may be irregular lasting several weeks.
Other local clinical features consist of abdominal pain of various severity and distribution and dyspepsia resembling peptic ulcers. The patient may also present with loose bowel motions which are followed by obvious diarrhoea with mucus or blood. At least a half of the affected children do not suffer from these bowel symptoms but when they occur, they constitute very significant features which are important clinical aids to the recognition of intestinal bilharzias. Bilharzia worms can also cause acute appendicitis where worms or ova are found in the inflamed organ.
The Late Stage
The late stage is fibrosis and calcification which occur where there are many eggs in the tissues. Bilharzia fibrosis causes disease in the liver, lungs and heart resulting in enlarged liver, pulmonary fibrosis and heart failure. Anaemia also occurs. Spinal cord damage leads to paralysis.
Diagnosis
The diagnosis of schistosomiasis is confirmed by finding eggs in stools or urine during a microscopic examination. If this test is found to be negative, a rectal snip or biopsy can be done. Also eosinophil counts can aid in the diagnosis as well as serological tests which are also highly sensitive and yield specific results.
Management These are various drugs on the market used for treatment of Bilharzia. They include:
- Lucanthone (Miraal D) at the dosage of 100mg/kg divided in six doses given for 6-8 days.
- Oxamniquine which is also a derivative of Lucanthone at the dosage of 50-60mg/kg given in four divided doses on successive days.
- Niridazole (ambilhar) at the dosage of 20-40mg/kg in two divided doses for six days
- Metriphonate given orally the dosage 28 mg/kg per dose, administered in three doses at an interval of 14 days.
To assess if the patient has been cured by these drugs, it is necessary to carry out a stool egg count. If after 6-12 weeks there are no eggs in the stool then the patient is cured.
Prevention
Prevention of bilharzia centres on controlling the breeding of snails using copper sulphate in ponds and dams as well as draining or filling water bodies and clearing vegetation in water bodies to deprive snails of food and resting places. Infection of snails may also be decreased by using pit latrines although it has been found that only a small amount of contamination is needed to keep the infection going. Children should be discouraged from swimming in ponds. All said and done, the most effective way to protect children and adults from schistosomiasis is to educate them about the disease and to give them ample supply of safe water. Water can be made safe by keeping it in a container for 48 hours using the three-pot system. Within this period of time the cercariae will die.
Lastly, let us now look at Kala azar.
4. KALA AZAR (Visceral Leishmaniasis)
Kala azar or visceral leishmaniasis is a parasitic disease which infests viscera or tissues of the infected persons. The commonly affected viscera are the spleen and the liver. While the bone marrow is the most involved body tissue. In Kenya the disease is commonly seen in eastern Kenya Kenya along the Tana and Athi rivers.
Life Cycle
The disease is caused by flagellated protozoa called Leishmania donovani. Man is the usual reservoir of the disease, although dogs and jackals are also considered reservoirs.
The protozoa are transmitted from man to man by the sand fly. This fly lives on anthills where it bites the children and young adults while they are out in the field. The parasites develop in the fly till they are injected in the next human victim and the cycle is completed. The parasites multiply in these viscera; spleen and liver as well as in the bone marrow, causing enlargement of the affected organs. Bone marrow involvement results in anaemia. There is depressed body immunity leading into susceptibility to infections such as pneumonia and tuberculosis.
Clinical Features
The incubation period of visceral leishmaniasis varies from 4 weeks to 2-6 months or even longer (up to 2 years) The clinical features may set in gradually or suddenly. The onset is heralded by fever which is irregular but continuous. There are however no associated systematic symptoms and the affected individuals’ appetite remains good. Emaciation occurs later and there may be lymphadenopathy.
The main features of the disease are progressive enlargement of the spleen and liver. The spleen assumes enormous size. In addition, there is epistaxis, bleeding from the gums, and falling out of teeth. Concrum oris occurs in severe cases. Anaemia also occurs due to bone marrow infiltration by the parasite as well as from the bleeding tendencies described above. In advanced cases, severe malnutrition develops with hair and skin changes, oedema and marked wasting.
Diagnosis
The diagnosis is suspected from clinical features and confirmed by finding of leishmania donovani bodies on liver aspirate or bone marrow biopsy. The disease can be confused with chronic malaria especially the Tropical splenomegaly syndrome.
Treatment
Kala azar is treated by sodium stibogluconate at the dose of 20mg/kg body weight , given intravenously for 30 days. The cure rate stands only at 80%. Relapses are common after cure. General management includes correction of anaemia and malnutrition. Prevention
Prevention includes elimination of the vectors and early treatment of the affected children to reduce the spread of the disease in the community.
We have described common helminths that infecting children. We have spelt out their life cycles and mode of transmission. We have also described the presentation and treatment of children with these worms. How can worms be prevented in our communities? Read on to find out.
| 8
What can you do to help prevent the spread of intestinal works in your community? ……………………………………………………………………………………… ……………………………………………………………………………………… ……………………………………………………………………………………… ……………………………………………………………………………………… ……………………………………………………………………………………… ……………………………………………………………………………………… ………………………………………………………………………………………
|
15.4 PREVENTION
As you will appreciate, it is not right to prevent the spread of one worm and leave the others. So we should aim at instituting preventive measures for all helminthic worms at the same time.
You should encourage and teach community members through health education sessions to prevent helminthiasis through the following simple measures:
- Washing of hands before and after meals;
- Washing of hands with soap and water after visiting a toilet;
- Washing fruits and vegetable before eating them;
- Thorough cooking of vegetables and meat;
- Proper faecal disposal;
- Wearing shoes or protective foot wear specially when children are playing or with parents in the gardens;
- Keeping of compounds and verandas clean and free of human excreta;
- Regular deworming preferably every two years of children above 2 years of age.
15.5: SUMMARY
Congratulations! You have now come to the end of this unit on helminithiasis. We divided helminthiasis into two broad categories. These were
- Intestinal Helminths:
- Ascaris lumbricoides (roundworms)
- Ankylostoma duodenale and Necator americanus (Hookworms)
- Taenia saginata and Taenia solium (Tapeworms)
- Trichuris trichura (Whip worms)
- Enterobias vermicularis (thread or pin worms)
- Strongyloides stercoralis.
- Visceral or tissue helminths, namely:
- Filaria
- Hydatid
- Schistosome
- Kala azar
If there is any section of this unit that you are not clear about, please write to your tutor for clarification or discuss it with your supervisor. Otherwise take a break and then complete the attached Tutor marked assignment and send it to us for marking.
|
DIRECTORATE OF LEARNING SYSTEMS DISTANCE EDUCATION COURSES
Name: ________________________________________ Address: _______________________________________ _______________________________________________
CHILD HEALTH COURSE Unit 15: Assignment INTESTINAL HELMINTHS (INTESTINAL WORMS)
1. Describe how you recognise a child who has hookworm infestation.
………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… 2. Explain how you would treat a child with Ascariasis: ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… …………………………………………………………………………………………………………
………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… …………………………………………………………………………………………………………
a. What would be your immediate suspicion of the child's problem? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… …………………………………………………………………………………………………………
b. What would be your plan of action in the management of this child? ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… …………………………………………………………………………………………………………
………………………………………………………………………………………………………… ………………………………………………………………………………………………………… ………………………………………………………………………………………………………… …………………………………………………………………………………………………………
a) What worm infestation may cause this condition? __________________________________________________________ b) How would you treat this condition? _________________________________________________________ _________________________________________________________ _________________________________________________________
a. What are you likely to find on abdominal examination? _________________________________________________________ _________________________________________________________ _________________________________________________________
_________________________________________________________ _________________________________________________________
_________________________________________________________ _________________________________________________________ _________________________________________________________ d. How would such a child be treated? _________________________________________________________ _________________________________________________________ _________________________________________________________ e. List important ways in which this condition can be prevented in that community? _________________________________________________________ _________________________________________________________ _________________________________________________________
|