K.I.S.S.ing Diabetes
Contents
Learning Objectives
Upon completion of this teaching lesson the learner will be able to
- Explain what Diabetes Mellitus is and provide three actions that reduce their chance of complications (i.e. check blood sugar level routinely, practice good foot care, manage diet, state exercise the enjoy, etc
- Explain what hypoglycemia is
- Identify two appropriate injection sites
- Perform self insulin injections and draw up the correct insulin dose after the educator has provided demonstration
- Explain how to perform good foot care and prevent skin complications
- Identify two major complications associated with Diabetes
- Discuss and rationalize need for adequate support system, compliance with medications and follow up appointments
Learning Theory
Jean Watson's Caring Theory – because diabetes is so complex, it is often difficult to treat the patient as a whole vs. a necrotic foot ulcer. The main idea in Watson's theory is seeing the patient from a wholistic perspective and addressing both their medical problems in addition to their emotional, spiritual and mental well being. Diabetes is more than just a disease that affects the heart, eyes, skin, etc. It can be extremely debilitating on all aspects of being human. By using Watson's theory to create this teaching plan, the patient is addressed as a human being. Their entire needs are met and overall health is improved. Watson's theory further asks the educator/RN/health care provider to reflect on their ability to perform their task and assess their competence. In order to be as effective as possible in teaching diabetes, it is important for one to look intuitively into their own ability to teach. Since Watson's theory fosters a great learning experience for both the patient and the health care provider, it is the best theoretical framework for teaching diabetes.
What is Diabetes Mellitus
Diabetes Mellitus is a chronic medical condition involving abnormally high blood sugar (also known as glucose) levels. In our bodies, we have a hormone called insulin that is responsible for controlling the amount of blood sugar that circulates throughout our bodies. When we eat and drink our bodies simply break down the materials it needs to function. Included in this is sugar which is absorbed into our bloodstream and triggers our pancreas to make insulin. The pancreas is a gland part of the digestive and endocrine system and produces hormones such as insulin and glucagon that assist our bodies in breaking down food we take in. Once insulin is created, sugar is able to move in and out of our cells. In the cells, the sugar is changed to energy which our bodies use right away or store for future use.
As we go about our day, our blood sugar level changes. Often times it becomes higher after a meal and usually return to normal or baseline within 2 hours and insulin production then slows down. Normal blood sugar ranges between 70 - 110 milligrams per deciliter. When our bodies does not produce enough insulin to move the sugar into the cells, the results include a high amount of sugar circulating in our bloodstream and inadequate amounts of sugar in our cells. This is then called Diabetes Mellitus.
Diabetes Mellitus can be a serious medical condition. There are currently 25.8 million children and adults in the United States with Diabetes. That is 8.3% of our population! The need for education regarding Diabetes is crucial as there are 18.8 million people who are currently diagnosed and 7.0 million people left undiagnosed. In addition, there are 79 million people who are prediabetic and at high risk for developing Diabetes later in life. source:http://www.diabetes.org/diabetes-basics/diabetes-statistics/
| Diabetes Overview. From AnswersTV
[[1]] |
Type I and Type II
Type I (aka insulin-dependent diabetes & juvenile onset diabetes)
- Occurs during the age of 30
- Makes up 10% of all Diabetics (rare)
- Pancreatic cells that produce insulin are 90% damaged
- Pancreas creates only little if no insulin
- Environmental factors (i.e. viral infections & nutritional factors in early childhood) could have effects
Type II (aka non-insulin-dependent diabetes & adult onset diabetes)
- May occur in childhood or adolescent but usually appears around the age of 30 and continues to progress over time
- 15% of diabetics older than 70 years old have this form
- African Americans and Hispanics are 2-3x greater at risk
- Pancreas still works and produces insulin but the body forms resistance to insulin and rejects it
Risk Factors
- Weight - Being overweight and obese or having a high BMI put you at greater risk for developing Type II. Remember that fatty cells are resistant to insulin
- Inactivity - sedentary lifestyle promotes risk factors for becoming overweight. When you dont move your body does not use glucose for energy
- Family history - Your risk increases when your parents or siblings had/have Diabetes
- Race - including African Americans, Hispanics, American Indians and Asian-Americans have higher risk of developing Diabetes
- Age - older age --> higher risk due to decrease in exercise, weight gain, inactivity, and poor diet
Hypoglycemia
Hypoglycemia is a term used to describe low blood sugar levels. Hypoglycemia occurs with people who take insulin and oral antiglycemic medications. It can occur when people take too much insulin, do not eat enough food, exercise without snacking before activity, skip or wait too long before meals and take in excessive amounts of alcohol. When your blood sugar gets too low, you may experience perspiration, anxiety, begin to shake or tremble, and feel hungry. If left untreated, you may experience difficulty walking, extreme weakness, vision and personality changes, disorientation and may loose consciousness or have seizures. This is a serious condition and it is important to check your blood sugar level for accuracy, check it routinely, treat with appropriate amounts of insulin and call for medical help. It is recommended to have glucose tablets or hard candy available nearby in case you experience hypoglycemia.
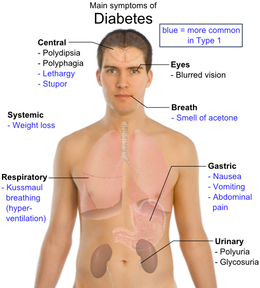
Signs/Symptoms
Type I and Type II have similar signs and symptom but mostly reflect on high blood sugar levels. There are the cardinal 3 Ps (polyuria - frequent urination, polydipsia - excessive thirst, polyphagia - excessive hunger) that explain the majority of the symptoms individuals experience.
When the blood sugar is high (i.e. 160 - 180 mg/dl, sugar spills into our urine causing high sugar levels. Our kidneys then produce additional water to dilute our urine. Since the kidneys produces an excessive amount of urine, the individual then has frequent urination. The constant urination makes the individual abnormally thirsty. As calories are lost with frequent urination, the individual may begin to lose weight. They attempt to compensate by eating more.
| Type I | Type II |
|---|---|
| frequent urination | any or all of the Type I symptoms |
| unusual thirst | frequent infections |
| extreme hunger | blurred vision |
| unusual weight loss | cuts/bruises that are slow to heal |
| extreme fatigue/irritability | tingling/numbness in hands and feet (Neuropathy) |
| source: http://www.diabetes.org/diabetes-basics/symptoms/ | recurring skin, gum, or bladder infections |
Complications
Diabetes can be a long term and serious medical condition. It is progressive and the more an individual is able to control their sugar levels, the less they are likely to develop complications. When our blood sugar levels are high, blood vessels begin to narrow. Sugar substances begin to build up along the walls of our blood vessels, making them thick and leaky. Blood supply to our body decreases as vessels become less elastic and plaque begins to build up (Atherosclerosis). In time, the poor circulation and continued high blood sugar affect our heart, brain, eyes, kidneys, nerves, skin. Chest pain, heart failure, strokes, leg pain (claudication), poor vision, renal failure, and skin break down occurs.
Poor circulation to the skin leads to infections and ulcers that are slow to heal. They are commonly found on the feet and legs. Extreme complication can lead to amputation when the ulcers/infections do not continue to heal.
Diabetic retinopathy is seen when damage to the blood vessels in the eyes occur. This often leads to loss of vision. This can be fixed with laser sugery that closes off leaky blood vessels. Prevention by having routine eye exams is recommended.
As kidneys have decreased function or fail, dialysis or kidney transplants may be necessary. Having high levels of albumin in our urine can be an indicator for kidney damage.
Nerve damage (aka diabetic polyneuropathy) may occur in the hands, legs and feet in which the individual experiences tingling and numbness in these areas. It is also associated with burning pain and weakness at times, putting the individual at risk for injuries.
| Diabetes and associated complications. From boehringeringelheim |
Managing Diabetes with Insulin
Insulin is measured in units and can come in several forms (vial or pens)
Types of Insulin
| A detailed overview of the different insulins available. From DiabetesCenter |
How to Inject Insulin
1. Roll your insulin - needed when using intermediate or long acting insulin (cloudy). This is done by rolling your vial in between your palms to mix the insulin.
2. Measure air - using a syringe, measure the amount of insulin you will be administering. This will be the same amount of air you will measure. Be sure to match the black plunger of the syringe to the correct number
3. Equalize the pressure - remove cap of your insulin vial, wipe with alcohol. Remove cap of your insulin syringe and plunge the syringe into the rubber stopper of the vial. Remember to keep the vial facing upward on a hard surface. Push all the air into the vial. This is equalize the pressure in the bottle and make it easier to draw the insulin.
4. Turn the bottle - keeping the needle in place, turn the bottle upside down and make sure that the entire needle is covered with insulin.
5. Measure your dose - keeping the bottle upside down, draw the correct amount of insulin you need. Remember to continue using the black plunger to mark your dose.
6. Pull out the needle - once you have your correct dose pull the needle out of the bottle
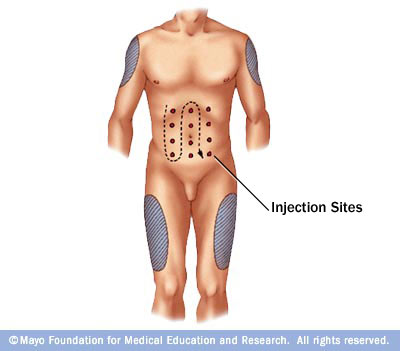
7. Choose injection site - The appropriate injection sites include abdomen, top of thighs and back of upper arms. *** Avoid broken or scarred skin*** When using your abdomen, divide your abdomen into four equal squares resulting in the Right Upper Quadrant (RUQ), Left Upper Quadrant (LUQ), Right Lower Quadrant (RLQ) and Left Lower Quadrant (LLQ). You will most likely be injecting yourself more than once a day. It is best to choose a different site each time you inject.
8. Inject yourself - clean the injection site with alcohol and hold the syringe the way you hold a pen or pencil. Using your free hand, pinch the skin and inject at a 45 degree angle with the bevel part of the needle facing up. (the bevel is the hole of the needle and is slightly slanted).
| Diabetes Center: Injecting Insulin. From postcarecom |
Caring for yourself and making lifestyle changes
Diabetes is a complex medical condition and it requires committment, effort and hard work to prevent complications. When you are able to control your blood sugar the need for medication may decrease. There are several lifestyle changes that both prolong life, reduce risk factors, decrease complications and improve total well being.
- Exercise - assists in lowering high blood pressure and cholesterol, improves blood sugar control, promotes weight loss and an overall outlook on life and improved health. All individuals with or without diabetes can benefit from the effects of exercise. There are several forms of exercise that are available to diabetics including aerobics, walking, swimming, dancing, yoga, etc. 30 minutes a day is adequate. It is important to choose an exercise regimen that fits your lifestyle, abilities and one that you enjoy.
- Smoking - increases an individuals risk for heart attacks and strokes (two complications highly associated with diabetes). Diabetics who smoke have higher risk for developing abnormal cholesterol levels, poor blood sugar control, increased nerve and kidney damage and foot ulcers.
- Alcohol - moderation is always key. Be aware of slight increases followed by a decrease in blood sugar level when taking alcohol. Alcohol has no nutritional value and may be a contributor to weight gain or weight loss control.
- Diet - having diabetes should not completely stop you from eating what you want. Like alcohol, moderation and self control is key. It is important to continue including carbohydrates into your meals. Eating three meals a day without skipping meals is also necessary. It is advisable to have a variety of foods in your diet to ensure that your body receives all the necessary requirements. Remember to time your meals with your insulin regimen. Knowing the action mechanism of the type of insulin you take can help you determine when it is best to eat and take insulin. As a diabetic, it is important to you also keep in touch with your nutritionist/dietitian. They are experts in this field and can certainly assist you in creating a meal plan that works for your pallate and helps you control your blood sugar.
- Skin and foot care - foot complications are common among diabetics due to poor circulation, poor wound healing and nerve damage. Long standing high blood sugar affect blood vessels, causing less blood flow that weakens our skin. When nerve damage occurs, your ability to notice pain and pressure is impaired making you prone to developing foot ulcers, athlete's foot and gangrene. It is important to wash and check your feet daily for skin changes, deformities and circulation, wear shoes that accommodate the shape of your feet, choose cotton socks that breath and fit comfortably and practice good hygiene.
- Medications and Appointments - managing your medications can be a difficult task. Often times it involves numerous medications and a full understanding of administration times. Organization is key as your daily medication regimen can include both oral and injectable forms of antigylcemic drugs.
As always, it is best to consult with your physician regularly and keep yourself involved with managing your condition. By following the suggestions outlined below you are making yourself an active participant in your care and taking better control. Remember that there is life with diabetes.
Are you at risk?
Diabetes Risk Test
http://www.diabetes.org/assets/pdfs/alert-day-2011/diabetes-risk-test-english.pdf
Support Groups and Community Involvement
Diabetes can be complicated to control but with proper understanding of your condition and a good support system you can live normally. Having family and friends there to support and assist you in managing your medications, keeping you up to date with your follow up exams, assisting you in administering your insulin and supporting your lifestyle changes can make dealing with your medical condition easier.
There are several support groups available near your household. You may find some online and your physician can provide you with support programs and educational classes. The following websites offer peer to peer support groups:
http://www.defeatdiabetes.org/support_groups.htm
http://www.diabetessociety.org/services/support-groups
http://www.dailystrength.org/c/Diabetes-Type-2/support-group
World Diabetes Day is November 14
| World Diabetes Day. From DiabetesHand |