Lesson 1: Introduction to Communicable Diseases (include epidemiology)
| At the end of this unit the student should be able to describe the principles of communicable disease control and prevention.
Specific objectives
|
Contents
Introduction
Communicable diseases
Communicable diseases are diseases that are as a result of the causative organism spreading from one person to another or from animals to people. They are among the major causes of illnesses in Kenya and the entire Africa. These diseases affect people of all ages but more so children due to their exposure to environmental conditions that support the spread. Communicable diseases are preventable base on interventions placed on various levels of transmission of the disease.
This region is also faced with new and emerging diseases which are challenging public health as never before. Unfortunately, many of these diseases affect the poor and marginalized sections of society, and contribute not only to ill health and poverty at micro-level but also have serious socio-economic implications at the macro-level. Health workers have an important role to play in the control of these diseases by applying effective and efficient management, prevention and control measures. Health workers need to be equipped with capacity to target communicable diseases for eradication.
lesson
Communicable diseases common characteristics of importance
1.They are very common 2.Some of the cause death and disability 3.Some of the cause epidemics 4.Most of them are preventable fairly simple interventions 5.Many of the affect infants and children
Classification of communicable disease
There are various ways of classifying communicable diseases, the classification below is the one that is considered to be best for ease of understanding. The detailed description of these classes of diseases will be discussed in the respective chapters in this course.content.
Contact diseases e.g. scabies, pediculosis, bedbugs, fleas, flies, fungal skin infections, trachoma, acute bacterial conjuctivities. Sexually transmitted diseases and HIV/AIDS Vector borne diseases e.g. relapsing fever, bancroftian filariasisn onchocerciasis, yellow fever, trypanosomiasis, plague, schistosomiasis, dracunculosis, leishmaniasis) and Malaria. Diseses caused by Faecal – oral contamination e.g acute gastro-enteritis, bacillary dysentery, campylobacter jejuni, giadiasis, amoebiasis, cholera, enteric fevers, food poisoning, poliomyelitis, viral hepatitis.
Helmonthic diseases e.g. Ascariaris, enterobiasis, trichuriasis, hookworm, strongyloidiasis, taeniasis, hydatidosis
Airborne diseases ;Acute respiratory infections, Meningitis (bacterial and fungal) Tuberculosis and leprosy. Zoonotic diseases (diseases of contact with animals or animal products) e.g. anthax, brucellosis, rabies, hydatidosis, tetanus.
BASIC EPIDEMIOLOGY
|
Epidemiology Epidemiology is the study of distribution and determinants of disease and conditions among populations. Disease distribution is considered in terms of Persons, time and place (Who, when and where). Persons who are affected by disease in terms of age, sex, race, occupation etc. The common characteristics relating to those persons affected by disease. Time relates to when the diseases is most likely to strike e.g. an epidemic, endemic, seasonal, cyclic etc Place refer to the geographical distribution of a diseases and the common characteristics that are favourable for that diseases in the given locality. Some diseases are localized, regional, pandemic etc. |
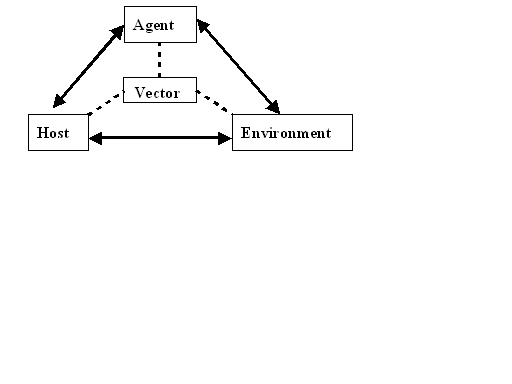
Disease determinant factors include the Agent, host and environment.
|
Agent refers to the disease causing organism characteristics e.g. habitation, breeding migration, infectivity, climatic and environmental factors favouring its existence. Host refers to the biological makeup of the individuals that make the vulnerable to the specified illness e.g. physical condition, genetic make up, habits etc. Environment refers to the ecological conditions that favour the interaction of host and agent e.g. swampy areas, bushes within house holds, sanitation etc. |
The epidemiologic cycle
The epidemiologic cycle is a diagrammatic illustration of the interaction between disease determinant factors (figure 1)
Fig.1. Disease causation cycle
From WikiEducator Jump to: navigation, search
The host, agent and environmental factors have to be conducive for the disease to occur. All communicable disease requires that the three factors are present for individuals to be affected.
Vector is a vehicle that some of the agents or disease causing organism require to be move from one point to the other, some require it to complete their developmental cycle e.g. a mosquito in transmission of malaria. Not all communicable diseases require a vector for transmission.
Control and prevention measures can be implemented at the various levels of the chains shown above e.g. to break the chain between host and environment for malaria disease you need to clear swampy areas, bushes and proper disposal of waste. To break the chain between host and agent in malaria disease one can take prophylactic anti-malaria drugs. To break the chain between the environment and the agent one can spray the breeding sites for mosquitoes and for the vector and host chain one can sleep under mosquito net.
Disease transmission
Disease transmission process has three components i.e source, transmission route and susceptible host. Source is the origin of the disease causing organism. This could be infected person, animal, place or object. Transmission route the main routes of transmission are;
- Direct contact for example sexual contact
- Vectors like mosquitoes
- Faecal oral (ingesting contaminated food and water)
- Airbone
- Transplacental (mother to foetus)
- Blood contact (transfusion, surgery, injection)
- Contact with animals or their products that are infected.
- Susceptible host is an individual who has low resistance to particular disease. This may be due to various factors such as;
- Lack of previous contact with the disease hence no immune cells
- Immuno suppressive illnesses such as AIDS
- Malnutrition
- Drugs that a person may be consuming.
Control and prevention measures
Each and every communicable disease has its own unique source, route of transmission and susceptible hosts. The principles of control and prevention should be geared to wards Attacking the source of the disease causing organism Interrupting the transmission cycle Protecting the susceptible host.
- Example
In the case of malaria we can attack the source by clearing and praying mosquito breeding sites, we interrupt the transmission route by spraying and killing the mosquitoe hence the causative organism and lastly we can protect the susceptible host by giving prophylactic medications, sleeping under mosquito nets etc.
To understand the transmission process of communicable diseases it is paramount to understand the Natural history of a disease.
Natural history of disease
|
The natural history of disease refer to the process of disease/condition progression from the time it affect an individual to the time the individual recovers or dies if appropriate measures are not instituted. The process has two distinct periods;
Sub clinical horizon; the host cells have started dying but to major effects are felt yet and the host has no signs or symptoms of the disease. At this level only laboratory tests would reveal the extent of damage. Clinical horizon; at this time the damage on the cells is so much that some of the hosts body functions are starting to fail. This manifests in signs and symptoms of a disease that the host is feeling uncomfortable or sick. If the host does not receive appropriate medical intervention then thy get in to the next stage. Early disease stage; at this time the disease effects are real as a result of massive cell damages that are affecting tissues functions. The host need appropriate intervention to correct the damage. If they fail to receive correct interventions then the disease gets in to the next level. Advanced disease; at this level the damage to the host systems is massive and may be irreversible leading to disability, or permanent damage. The host has three outcomes at this stage i.e. recover, permanent disability, convalescence or in worst cases death. Figure2 illustrates the natural history of disease/conditions process. |
Fig.2 The natural history of disease/condition.
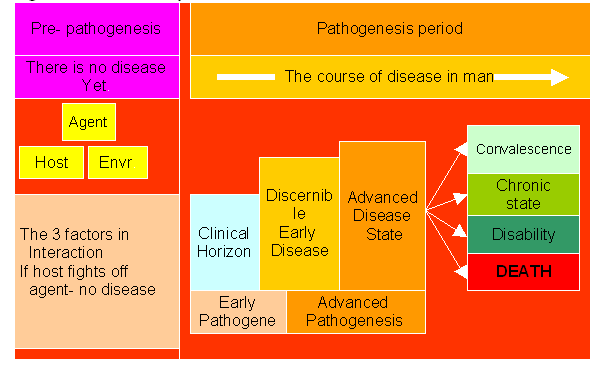
Disease prevention
|
Disease prevention refers to deliberate actions to halt or delay disease progression from one stage to the next. There are three levels of disease prevention; |
- Primary prevention
This is the most common especially for communicable disease. This level is targeted at the pre-pathogenesis period or the period before the disease infects the individual. The interventions include General measures such as health education, safety measures and healthy behaviour.
Specific measures such as vaccination, prophylaxis medication etc.
- S'econdary prevention
This mainly happen during the early stages of disease process. The purpose is to prevent further damage to host cells and tissues and thus avoid disease complications. Measures would include early diagnosis, screening and prompt treatment.
- Tertiary prevention
This takes place during the advanced stages of the disease progression to minimise the complications or reverse the effects. Main interventions are rehabilitative in nature and include physical therapy, occupational therapy, psychotherapy, corrective/rehabilitative surgery etc.
Measures of disease in populations
Epidemiologists use various methods and approaches in quantifying disease cases in a population such as; *counts, *ratio, *proportion, *percentage, and *rates.
- Count- : number of individuals with a specified quality in a defined population.
- A ratio- expresses the relationship between two numbers in the form of
X: Y E.g. Ratio of males to female is1:3
- Proportion-is a specific type of ratio in which the numerator is included in the denominator and the resultant value is expressed as a part of the whole.
X/X+Y or X per X+Y E.g. proportion of males in the class is 4 per 10 students, or 40 per 100 students or 400 per 1000 etc.
- Percentage- is a proportion that is expressed per 100.
X per 100 E.g. 40 percent of the community members are males
It is a very common measure of disease in various epidemiological descriptive studies.
- Rate
It is a special form of proportion that includes specification of time and population. It is the basic measure that most clearly expresses probability or risk of disease in a defined population over a specific period of time. The rate is defined as follows;
Rate = no of events in a specified period x K
Population at risk of the specific event in a specified period
Where k is a constant that may be set (fixed) for certain rates or set by the investigator for convenience.
Application of the measures in populations
Incidence The incidence of a disease or health condition refers to the number of persons in a population who develop the disease/condition during a specified period of time. The determination of incidence requires that a population is followed up over a period of time through a prospective study.
Incidence rate = Number of new cases in a population over a Specified duration of time in a given population x K
The population at risk of developing the disease/condition at the beginning of the duration of interest.
Example Kilanga village has a population of 1500 males and 2000 females. A prospective study is conducted over two years to establish the incidence of cancer of prostate within the population during which 30 males were developed the disease. Calculate the incidence of the disease in the population.
Incidence rate= 30 (individuals who developed the disease) 1500 (males)
= 0.02 cases for ease of interpretation we multiply by K which we may take to be 100 for this case and it will be;
incidence= 2 cases per hundred males in the population of Kilaga village within the two years of study.
Prevalence The prevalence of a disease or condition refers to the total number of persons who have the disease/condition of interest at a particular time. Prevalence rates are calculated at a point in time (point prevalence) or over duration of time (period prevalence).The information required for point prevalence is obtained from cross sectional studies and in period prevalence is obtained from retrogressive studies.
Point prevalence = number of existing cases of Disease/condition at a specified point in time. x K
Total population at that point in time.
Example
Data collected in match at kilanga village revealed that there were 140 cases of malaria at the time of data collection. If kilanga village had a total population of 3500 persons, calculate the point prevalence of malaria at that time.
Point prevalence = 140 (cases)
3500 (population)
= 0.04 cases
for ease of interpretation we multiply by K in this case we take it to be 100.Hence the report will read
Point prevalence of malaria for kilanga village in March was 4 cases per 100 people.
Period prevalence = number of existing cases of
disease/condition over a specified duration of time. x K
average population over the specified duration of time.
Example
Records obtained from kilanga village indicate that for the previous six months inclusive of March the number of malaria cases was 700. Calculate the period prevalence of the disease assuming that the population remained constant at 3500 over that duration.
Period prevalence= 700 (cases) 3500 people = 0.2 cases Hence for ease of interpretation we multiply by K which we may take to be 100. The period prevalence will be 20 cases of malaria per 100 persons in kilanga village over the last six months.
Importance of incidence and prevalence rates
Incidence rates help us to know how fast the disease is spreading, infecting or affecting people Prevalence rates help us to know how many people are having a disease in the population Prevalence can also give an indication of how fast people are recovering, dying from the disease and how many are in chronic stage of the disease. With this knowledge you can be able to interpreter and predict disease epidemiologic patterns and hence plan for interventions. You can determine if a disease is an epidemic or endemic.
How to determine endemic and epidemic diseases
- Epidemic;
This is the occurrence of disease cases at a frequency that is higher than the normal for the population in a give period of time.
- Endemic;
This is the occurrence of disease/condition in a given population at frequencies that are constant over a duration of time. However these frequencies are higher that would be expected for that population. Figure 3 illustrates.
Figure 3. The epidemic and endemic patterns of communicable diseases.
Note; some communicable diseases are endemic in some regions of our country while others appear as epidemics.
Assignment
List the communicable diseases that are endemic in specific regions of this country List the communicable diseases that are epidemic in specified regions of this country.
Commonly used rates
Measures of natality Crude birth rate = Number of live births during time interval x 1000 Estimated mid-interval population
Fertility rate = Number of live births during time interval x 1000 Number of women aged 15 – 44 at mid-interval
Measures of morbidity and mortality
Crude death rate = Number of deaths during time interval x 1000 Estimated mid-interval population
Specific death rate = Number of deaths in sub group during time interval x 1000 Estimated mid-interval population of subgroup
Cause specific death rate= Number of deaths from specified cause during time interval x 1000 Estimated mid-interval population
Infant mortality rate= Number of deaths of infants age < 1year during time interval x 1000 Total live births during time interval
Neonatal mortality rate = Number of deaths of infants age < 28days during time interval x 1000 Total live births during time interval
Post neonatal mortality rate = Number of deaths of infants age ≥ 28days but
< 1year during time interval x 1000
Total live births during time interval
Epidemiological methods
Epidemiologic methods are the various approaches in which data is gathered analyzed and reports written with regard to various diseases distribution and determinants. They enable us to plan and evaluate disease management in communities.
They are several classified as; Descriptive methods e.g. Individual based (case study and case series) and population based (correlation studies, cross sectionals studies and surveys)
Analytical studies e.g. prospective (cohort studies) and retrospective (case control)
Experimental studies
Community based studies e.g. community trials
Descriptive studies These are basic studies that seek to describe the situation as it is. These methods utilize simple descriptive statistics such as percentages tables and graphs to describe the disease situation. These studies generate hypothesis.
Individual based studies; they reflect on single individuals as the unit of study Case report – a single unique case is reported as it is identified by the health worker. Case series- several case reports that have similar characteristics are analyzed so as to draw conclusions in relation to the particular disease of interest.
Population based studies
Surveys – are conducted over a short duration of time with specific objectives to meet. They are more of fact finding studies in a bid to rapidly draw conclusion with regard to illnesses or conditions affecting entire population. Cross sectional studies- these are studies carried out across a huge population sample over a very short duration of time. Their methodology and analysis is more advanced than that of surveys. Correlation studies- these studies seek to compare one variable or characteristic of population to one or more others. E.g. smoking and lung disease, immunization coverage and measles outbreaks. One may also compare worm infestation against use of latrines, amount of house hold water, maternal literacy etc.
Analytical studies These studies are more advanced in methodology and analysis and their findings are more generalisable as compared to descriptive studies. While descriptive studies generate hypothesis these ones test hypothesis.
Prospective studies (Cohort studies) These studies start with individuals with an exposure of interest (cohorts) and are followed up over time as they are compared with individuals who do not have the exposure of interest. Analysis is then done to find out if those who had exposure will develop the outcome of interest more that those without exposure.
Example People working in farms (exposed to zoonotic disease) are followed up over time to establish if they will manifest the zonnotic diseases. Simultaneously a similar group of individuals who do not work in the farms are followed up to establish if they develop zoonotic disease.
Retrospective (case control studies) These studies are easier to conduct consume less time and are cheaper than the cohort studies. Two groups are selected from a population one group with the disease of interest (case) and another without (control). Then they are asked about their past in order to establish if they had a common exposure that might have caused the disease. These studies are however prone to recall biases.
Example In a community people who have amoebiasis may be asked about their food (sources, preparation, storage and consumption) they have been consuming. Another group from same community who do not suffer from amebiasis is also asked the same questions then the data is analyzed.
Experimental studies
These are studies conducted in a controlled environment where the researcher has control over all variables. It is a laboratory set up kind of study. They are very useful in isolation of the actual disease causative agent. They are very strict and also very expensive. They require highly specialized personnel and equipment.
Community trials
These are studies involving and entire community.
Example
In one community water may be fluoridate while in the other it may not. The two are followed up and with time if those taking water that is not fluoridated start complaining of teeth problem then the effects of fluoride are confirmed.
Importance of epidemiology in communicable diseases control
Enables us to know the disease distribution patterns Enables us to know the disease causation factors It equips us with data that we can apply for effective prevention and control of diseases It enable us to understand the disease progression and what measures need to be take to halt or reduces disease effects It enables us to evaluate intervention programs It enables us to conduct research with regard to communicable diseases and how they affect populations.
Disease surveillance
Health Surveillance may be defined as the tracking and forecasting of any health event or health determinant through the; Continuous collection of high-quality data, Integration, analysis and interpretation of those data into surveillance products (for example reports, advisories, alerts, and warnings), Dissemination of those surveillance products to those who need to know. Surveillance products are produced for a specific public health purpose or policy objective. Surveillance should be purposeful, economical, and action oriented. It should not only detect emerging health risks, but include systems that allow public health officials to monitor and evaluate progress in health protection and disease prevention. New health risks such as bioterrorism and zoonoses, re-emergence of some diseases (e.g., multiresistant bacteria), and globalization have fundamentally altered the scope and response time expected of surveillance programs at every level. Surveillance uses whatever data sources will provide the necessary information. Surveillance systems may share data with personal health services information systems, but the end-products are different. Most of the data currently available from health facilities are originally generated for administrative purposes. They can serve as raw material for health services management and research, as well as for disease and health surveillance if procedures for capturing and handling administrative data are appropriately adapted. In general, surveillance data can originate from any of four classes of source: Special purpose, i.e., data collected specifically for a particular surveillance need. Special purpose data sources select the most relevant data and facilitate detection and response, but are costly to operate and may be difficult to maintain over the long term. Surveys. Usually collected for more general health surveillance purposes, survey data differ from other special purpose data sets in that they are usually cross-sectional or 'one-off' and may be useful for multiple surveillance functions, notwithstanding their lack of specificity. Administrative. As noted, data collected for administrative purposes often find a secondary purpose in disease surveillance, e.g., analysis of the diagnostic fields on hospital discharge abstracts looking for geographic clusters of a particular disease. Administrative data are generally lower quality, and may not always be available on a timely basis, but are convenient to acquire and inexpensive. Clinical. For many surveillance purposes, this is the ideal source. Indeed, new diseases and emerging clusters of known diseases are often first suspected by astute clinicians who observe unusual patterns of illness, and work with others to initiate more systematic surveillance. Optimum efficiency in clinical surveillance can only be achieved if the clinical data are accessible electronically. This is rarely the case at present. The Electronic Health Record has the potential to be a rich source of surveillance data in future. Moreover, as submissions to the Committee have pointed out, clinical data for surveillance need to be assembled from a range of providers and facilities, including family physicians and other primary care providers, emergency departments, pharmacists, and veterinarians.
Effective Communicable diseases control relies on an effective surveillance and response system that promote better coordination and integration of surveillance function. Recognizing this, the initiative to strengthen the disease surveillance system that promotes the integration of surveillance activities in Ethiopia was started in 1996. In 1998 WHO/AFRO, following the resolution of the 48th assembly started promoting Integrated Disease Surveillance and Response (IDSR) for all member state to adopt as the main strategy to strengthen national disease surveillance system.
Integrated disease surveillance and response (IDSR)
The specific goals of IDSR are to:
Strengthen district level surveillance and response for priority diseases,
Integrate laboratory with laboratory support,
Reduce duplication in reporting,
Share resources among disease control programs, and
Basic ingredients:
A good network of motivated people,
Clear case definition and reporting mechanism,
Efficient communication system,
Basic but sound epidemiology,
Laboratory support,
Good feedback and rapid response
Translate surveillance and laboratory data into specific and timely public health actions
Integrated disease surveillance envisages all surveillance activities in a country as a common public service that carry out many functions using similar structures, processes and personnel. The surveillance activities that are well developed in one area may act as driving forces for strengthening other surveillance activities, offering possible synergies and common resources.
Surveillance is based on collecting only the information that is required to achieve objectives for disease control. Data requested may differ from disease to disease and some diseases may have specific information needs, requiring specialized systems.
With the global momentum to scale up response to communicable diseases, public health practitioners need to review constantly their performance in detecting and responding to communicable diseases.
At the same time, they should remain accountable for their activities and policies to a variety of stakeholders. People at different levels of surveillance need to report accurate, timely and reliable data to national authorities, to ensure timely and effective responses to contain communicable disease outbreaks, and also to donors, to secure funding to strengthen surveillance and response activities to communicable diseases. Most importantly, all surveillance levels in countries should be able to utilize the surveillance information locally to address and resolve problems related to control of communicable diseases.
The International Health Regulations, currently under revision emphasize the commitment of Member States to the goal of global health security. This will require all Members States to maintain a functional and effective surveillance and response system that is able to detect, investigate and respond to public health emergencies of national and international concern.
Against this background and in response to requests from Member States, WHO, in consultation with technical partners and Member States, has developed a framework for monitoring and evaluating communicable disease surveillance and response systems. This framework aims to strengthen surveillance and response activities and builds on experiences gained by Member States in monitoring and evaluating their surveillance and response systems.
The framework contains a list of indicators that is proposed for purposes of monitoring and evaluating surveillance and response systems to communicable diseases.
Operational definitions of monitoring and evaluating The following definitions have been adopted for purposes of monitoring and evaluating communicable disease surveillance and response systems.
Monitoring is the routine (continuous) tracking of the performance of the surveillance and response systems.
Evaluating is the periodic assessment of changes in targeted results (objectives) that can be attributed to the surveillance and response system. Evaluation attempts to attribute changes in outputs, outcomes and impacts (negative or positive, targeted or non-targeted) of the surveillance and response system.
Figure3. The conceptual frame work of surveillance and response for communicable diseases
Notifiable diseases
In Kenya according to the public health act cap 254 ; 17(1) there are diseases that should be notified to the higher authorities above your office as a health worker once you come across them. They include;
The provisions of this Act, unless otherwise expressed, shall, so far as they concern notifiable infectious diseases, apply to smallpox, plague, cholera, scarlatina or scarlet fever, typhus fever, diphtheria or membranous croup measles, whooping Cough, erysipelas, puerperal fever (including septicaemia, pyasmia, septic pelvic cellulitis or other serious septic condition occurring during the puerperal state), enteric or typhoid fever (including para-typhoid fever), epidemic cerebro-spinal meningitis or cerebro-spinal fever, acute polio-myelitis, leprosy, anthrax, glanders, rabies, malta fever, sleeping sickness or human trypanosomiasis, beri-beri, yaws and all forms of tuberculosis which are clinically recognizable apart from reaction to the tuberculin test.
Epidemic response Outbreaks or epidemics are the occurrence of a disease in excess of its expected frequency. Outbreak investigations are a type of fast-paced epidemiologic research, undertaken to determine the cause of the outbreak and what remedial actions are required. These investigations are typically retrospective, occur in real time often under intense public and political pressure, begin without hypotheses, are iterative, and are closely tied to the implementation of public health measures to contain the outbreak. Outbreak investigations also involve considerable challenges in communication, including essential risk communication to the public. The investigation and management of infectious disease outbreaks is typically local and provincial, at least in the first instance. Other levels of government may assist, and the epidemic may even be managed by national or international bodies, but as a general rule, the first line of defense is local.
Recognition of a new threat has different permutations and challenges, depending upon whether the agent is known or unknown, whether the known agent is a notifiable or non-notifiable disease, and the extent of knowledge about how to contain the agent most effectively and efficiently Detection demands the timely upward reporting of data through the public health hierarchy - local, regional, provincial, national, global - and the collation and analysis of case data at the lowest level where a cluster of cases can be recognized On occasion, cases may be scattered widely so that an outbreak is not detectable at the local or even provincial level Steps involved Rapid epidemiologic assessment is essential at the beginning of an outbreak or epidemic to define the scope of the problem and start mobilization of containment strategies.
The next step is epidemic investigation to identify the etiology and the modes of transmission of an infectious agent, thereby guiding appropriate measures to prevent further transmission. An ongoing outbreak is generally a health emergency. Approaches to its investigation require different modes of operation, different command-andcontrol structures and unified leadership. Investigators should be insulated from the constant demands of data flow.
Establishing a case definition is central to disease surveillance and outbreak containment
Establishing aetiology is usually straightforward for known agents, provided the requisite logistical arrangements and laboratory capacity are in place. The ability to monitor data at the national and even provincial level may be undercut because of poor information systems and the lack of data sharing protocols. Epidemiologic and laboratory data became even more disintegrated, compromising epidemic investigation efforts.
Confirmation of cases presupposes the existence of a definitive test to ascertain true cases. When the agent is unknown, this takes some time.
Cases finding and defining the scope of the problem by the outbreak management and investigation team is paramount.
Generating descriptive epidemiologic information should be done immediately by the investigative team as data accumulate during the outbreak.
Generating and testing hypotheses should follow so as to have a working proposition of what may be going on.
Reporting of findings of epidemiologic investigations to national and international bodies is a critical part of an outbreak investigation for several reasons. Understanding a disease allows other jurisdictions to put in place appropriate measures for its control and to learn from the experience of others.
Outbreaks are often highly visible and are conducted under intense public, political and media scrutiny. Communications with the media, clinical personnel, governments, and the public are all extremely important.
The control of an epidemic through public health measures is the immediate purpose for epidemic investigations. With disease spreading, decisions on public health interventions need to be taken quickly and often with incomplete information. The actions that are taken in controlling any epidemic have very significant costs and may be controversial or highly unpopular.
The measures would include, case detection, isolation of cases, follow up and quarantine of contacts, strict infection control measures in hospitals, closure of hospitals, airline passenger screening and travel advisories.
End