Lab: Cardio fitness
Contents
- 1 Harvard Step Test - a measure of cardio fitness
- 2 Blood pressure
- 3 Cardio fitness lab
- 4 Materials needed
- 5 Procedure
- 5.1 Part 1. Fitness Evaluation
- 5.2 Part 2. Harvard Step Test
- 6 Questions for Analysis/Discussion
- 7 References
Harvard Step Test - a measure of cardio fitness
The Harvard Step Test is a type of cardiac stress test for detecting and/or diagnosing cardiovascular disease. It also is a good measurement of fitness, and your ability to recover after a strenuous exercise. The more quickly your heart rate returns to resting, the better shape you are in.[1] The Harvard Step Test was developed by researchers at Harvard University during World War II in order to test the cardiovascular fitness of military recruits, and today is used to gauge an individual’s relative cardiac fitness.[2] The test computes the capability to exercise continuously for extended intervals of time without tiring, so it is a test of endurance. The test is conducted by having a person step up and down on a platform at a height of about 45 cm. at a rate of 30 steps per minute for 5 minutes or until they reach a state of exhaustion. Exhaustion is the point at which the subject cannot maintain the stepping rate for 15 seconds. The subject immediately sits down on completion of the test, and the heartbeats are counted for 1 to 1.5, 2 to 2.5, and 3 to 3.5 minutes. Then the recovery index (RI) is calculated as follows:
[math]Recovery \ Index\ (RI)\ = \frac{Duration\ of\ exercise\ (seconds) * 100}{(\sum of\ 3\ pulse\ counts)*2}[/math]
Using the RI value and the chart below the overall cardiac fitness rating may be determined:
| Gender | Excellent | Above Average | Average | Below Average | Poor |
|---|---|---|---|---|---|
| Male | >90 | 80-90 | 65-79 | 55-64 | <55 |
| Female | >86 | 76-86 | 61-75 | 50-60 | <50 |
There are several factors that can influence the results of the Harvard Step Test, such as height of the bench stepped on as well as weight and height of the subject, so the relative cardiac fitness of an individual is not measured solely based on this test.
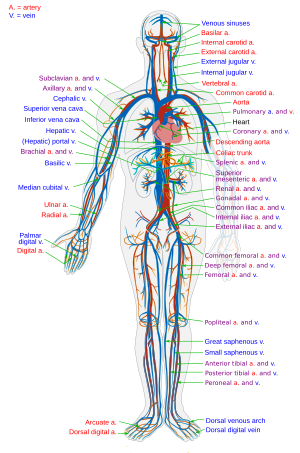
Blood pressure
An important measurable aspect of the circulatory system is blood pressure. When the ventricles of the heart contract, pressure is increased throughout the arteries. Arterial blood pressure is directly dependent on the amount of blood pumped by the heart per minute and the resistance to blood flow through the arterioles. The arterial blood pressure is determined using a device known as a sphygmomanometer. This device consists of an inflatable cuff connected by rubber hoses to a hand pump and to a pressure gauge graduated in millimeters of mercury (mm Hg). The cuff is wrapped around the upper arm and inflated to a pressure that will shut off the brachial artery. The examiner listens for the sounds of blood flow in the brachial artery by placing the bell of a stethoscope in the inside of the elbow below the biceps. At rest, the blood normally goes through the arteries so that the blood in the central part of the artery moves faster than the blood in the peripheral part. Under these conditions, the artery is silent when one listens. When the sphygmomanometer cuff is inflated to a pressure above the systolic pressure, the flow of blood is stopped and the artery is silent again. As the pressure in the cuff gradually drops to levels between the systolic and diastolic pressures of the artery, the blood is pushed through the compressed walls of the artery in a turbulent flow. Under these conditions, the blood is mixed, and the turbulence sets up vibrations in the artery that are heard as sounds in the stethoscope. These sounds are known as the heart sounds or sounds of Korotkoff. The sounds are divided into five phases based on the loudness and quality of the sounds.
- Phase 1. A loud, clear tapping sound is evident that increases in intensity as the cuff is deflated.
- Phase 2. A succession of murmurs can be heard. Sometimes the sounds seem to disappear during this time that may be a result of inflating or deflating the cuff too slowly.
- Phase 3. A loud, thumping sound, similar to that in Phase 1 but less clear, replaces the murmurs.
- Phase 4. A muffled sound abruptly replaces the thumping sounds of Phase 3.
- Phase 5. All sounds disappear.
The cuff pressure at which the first sound is heard (that is, the beginning of Phase 1) is taken as the systolic pressure. The cuff pressure with the muffled sound (Phase 4) disappears (the beginning of Phase 5). is taken as the measurement of the diastolic pressure. A normal blood pressure measurement for a given individual depends on a person's age, sex, heredity, and environment. When these factors are taken into account, blood pressure measurements that are chronically elevated may indicate a state deleterious to the health of the person. This condition is called hypertension and is a major contributing factor in heart disease, kidney disease and stroke. A healthy blood pressure is defined as one whose systolic value is less than 120 mm Hg and whose diastolic value is less than 80 mm Hg.
The table below shows the classification of blood pressure adopted by the American Heart Association for adults who are 18 years and older:
Table 1: Classification of blood pressure for adults according to the American Heart Association[4]
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
While average values for arterial pressure could be computed for any given population, there is often a large variation from person to person; arterial pressure also varies in individuals from moment to moment.
Table 2: Normal Blood Pressure for Men and Women at Different Ages
| |
| |||
| Age in Years | Men | Women | Men | Women |
| 10 | 103 | 103 | 69 | 70 |
| 11 | 104 | 204 | 70 | 71 |
| 12 | 106 | 206 | 71 | 72 |
| 13 | 108 | 108 | 72 | 73 |
| 14 | 110 | 110 | 73 | 74 |
| 15 | 112 | 112 | 75 | 76 |
| 16 | 118 | 116 | 73 | 72 |
| 17 | 121 | 116 | 74 | 72 |
| 18 | 120 | 116 | 74 | 72 |
| 19 | 122 | 115 | 75 | 71 |
| 20-24 | 123 | 116 | 76 | 72 |
| 25-29 | 125 | 117 | 78 | 74 |
| 30-34 | 126 | 120 | 79 | 75 |
| 35-39 | 127 | 124 | 80 | 78 |
| 40-44 | 129 | 127 | 81 | 80 |
| 45-49 | 130 | 131 | 82 | 82 |
| 50-54 | 135 | 137 | 83 | 84 |
| 55-59 | 138 | 139 | 84 | 84 |
| 60-64 | 142 | 144 | 85 | 85 |
| 65-69 | 143 | 154 | 83 | 85 |
| 70-74 | 145 | 159 | 82 | 85 |
Cardio fitness lab
This lab offers an opportunity for students to evaluate data related to cardiovascular fitness:
- Harvard Step Test: a cardiovascular endurance test used to measure cardiac fitness
- Effect of Position on Blood Pressure: to measure relative cardiac fitness based on blood pressure changes upon change in body position
Students will measure pulse and blood pressure in varying conditions, and use the data to determine overall fitness.
|
When you have completed this lab, you should be able to do the following:
|
Materials needed
- sphygmomanometer
- timer/stopwatch (in seconds)
- bench or other area for reclining
- calculator
- 45 cm step/bench
- yardstick
- metronome
- data sheet (1 for each subject being tested)
Procedure
Before beginning be sure to read over the complete procedure and print out a copy of the specific procedures and cardio fitness data sheet for use in recording your data.
Part 1. Fitness Evaluation
I: Standing Pulse Rate
For each subject being tested:
- Have the subject stand at ease for 2 minutes.
- After the two minutes, determine the subject's pulse.
- Count the number of beats for 30 seconds and multiply by 2. The pulse rate is the number of beats per minute.
- Record the beats per minute on the data sheet.
- Repeat steps 1-4 two more times.
- Calculate and record the average pulse rate.
- Assign fitness points based on Table 3 and record on the data sheet.
| Average Pulse Rate (beats/min) |
Fitness Points |
|---|---|
| 60-70 | 3 |
| 71-80 | 3 |
| 81-90 | 2 |
| 91-100 | 1 |
| 101-110 | 1 |
| 111-120 | 0 |
| 121-130 | 0 |
| 131-140 | -1 |
II: Reclining Pulse Rate
For each subject being tested:
- Have the subject recline for 5 minutes on a bench or other flat surface.
- Determine the subject's resting pulse, as the subject continues to recline; count the number of beats for 30 seconds and multiply by 2. The subject should continue to recline until step III.
- Record the resting pulse on the data sheet.
- Assign fitness points based on Table 4 and record on the data sheet.
| Pulse Rate (beats/min) | Fitness Points |
|---|---|
| 50-60 | 3 |
| 61-70 | 3 |
| 71-80 | 2 |
| 81-90 | 1 |
| 91-100 | 0 |
| 101-110 | -1 |
III: Baroreceptor Reflex (Pulse Rate Increase from Reclining to Standing)
For each subject being tested:
- Have the reclining subject stand up.
- Immediately take the subject's pulse. Record this value on the data sheet. (
 : The observed increase in pulse rate is initiated by baroreceptors (pressure receptors) in the carotid artery and in the aortic arch. When the baroreceptors detect a drop in blood pressure they signal the medulla of the brain to increase the heartbeat, and consequently the pulse rate.)
: The observed increase in pulse rate is initiated by baroreceptors (pressure receptors) in the carotid artery and in the aortic arch. When the baroreceptors detect a drop in blood pressure they signal the medulla of the brain to increase the heartbeat, and consequently the pulse rate.)
- Subtract the reclining pulse rate (recorded in step II.) from the pulse rate immediately upon standing (recorded in step III.) to determine the pulse rate increase upon standing.
- Assign fitness points based on Table 5 and record on the data sheet.
| Pulse Rate Increase on Standing (# beats) | |||||
|---|---|---|---|---|---|
| 0-10 | 11-18 | 19-26 | 27-34 | 35-43 | |
| Reclining Pulse (beats/min) | Fitness Points | ||||
| 50-60 | 3 | 3 | 2 | 1 | 0 |
| 61-70 | 3 | 2 | 1 | 0 | -1 |
| 71-80 | 3 | 2 | 0 | -1 | -2 |
| 81-90 | 2 | 1 | -1 | -2 | -3 |
| 91-100 | 1 | 0 | -2 | -3 | -3 |
| 101-110 | 0 | -1 | -3 | -3 | -3 |
IV: Heart Rate and Physical Fitness—Running in Place (Endurance)
During physical exertion, the heart rate (beats per minute) increases. This increase can be measured as an increase in pulse rate. Although the maximum heart rate is usually the same in people of the same age group, those who are physically fit have a higher stroke volume (milliliters per beat) than more sedentary individuals. A person who is in poor physical condition, therefore, reaches their maximum heart rate at a lower work level than a person of comparable age who is in better shape. Maximum heart rates are listed in Table 6. Individuals who are in good physical condition can deliver more oxygen to their muscles before reaching maximum heart rate than can those in poor condition.
| Age (years) | Maximum Heart Rate (beats/min) |
|---|---|
| 20-29 | 190 |
| 30-39 | 160 |
| 40-49 | 150 |
| 50-59 | 140 |
| 60 and above | 130 |
For each subject being tested:
- Recruit a partner to record the data.
- Jog in place vigorously for 2 minutes, being sure to lift each foot off the ground at least 8-10 inches with each step.
- Immediately after the completion of the exercise, count the pulse beats for 15 seconds (0-15 sec) and record on the data sheet.
- Count the pulse beats again for 15 seconds (16-30 sec) and record.
- Count the pulse beats, this time for 30 seconds (31-60 sec), and record on the data sheet.
- Repeat step 5, for two more 30 second intervals, 61-90 sec and 91-120 sec.
Return of pulse rate to standing after exercise
- Determine the time that it takes for the pulse rate to return to approximately the level as recorded in Test I (standing pulse rate).
- Assign fitness points based on Table 7 and record them on the data sheet.
| Time (seconds) | Fitness Points |
|---|---|
| 0-30 | 4 |
| 31-60 | 3 |
| 61-90 | 2 |
| 91-120 | 1 |
| 121+ | 1 |
| 1-10 beats above standing pulse rate | 0 |
| 11-30 beats above standing pulse rate | -1 |
Pulse rate increase immediately after exercise
- Subtract the normal standing pulse rate (recorded in step I.) from the pulse rate immediately after exercise (the 0-to 15-second interval in step V.) to obtain the pulse rate increase.
- Record the difference on the data sheet.
- Assign fitness points based on Table 8 and record them on the data sheet.
| Pulse Rate Increase Immediately after Exercise (#beats) | |||||
|---|---|---|---|---|---|
| Fitness Points | |||||
| Standing Pulse (beats/min) | 0-10 | 11-20 | 21-30 | 31-40 | 41+ |
| 60-70 | 3 | 3 | 2 | 1 | 0 |
| 71-80 | 3 | 2 | 1 | 0 | -1 |
| 81-90 | 3 | 2 | 1 | -1 | -2 |
| 91-100 | 2 | 1 | 0 | -2 | -3 |
| 101-110 | 1 | 0 | -1 | -3 | -3 |
| 111-120 | 1 | -1 | -2 | -3 | -3 |
| 121-130 | 0 | -2 | -3 | -3 | -3 |
| 131-140 | 0 | -3 | -3 | -3 | -3 |
V.: Blood Pressure Upon Positional Change
A sphygmomanometer (blood pressure cuff) is used to measure blood pressure. The cuff, designed to fit around the upper arm, can be expanded by pumping a rubber bulb connected to the cuff. The pressure gauge, scaled in millimeters, indicates the pressure inside the cuff. A stethoscope is used to listen to the individual's pulse. The earpieces of the stethoscope should be cleaned with alcohol swabs before and after each use. We may also use automated blood pressure cuffs of either the brachial (upper arm) or radial (wrist) variety, neither of which require the use of a stethoscope.
Method for manual blood pressure measurement
Work in pairs. Those who are to have their blood pressure measured should be seated with both shirtsleeves rolled up. You need to be silent so that the pressures can be heard!
- Attach the cuff of the sphygmomanometer snugly around the upper arm.
- Place the stethoscope directly below the cuff in the bend of the elbow joint.
- Close the valve of the bulb by turning it clockwise.
- Pump air into the cuff until the pressure gauge goes past 180 mm Hg.
- Turn the valve of the bulb counterclockwise and slowly release the air from the cuff. Listen for sound of a pulse.
- When you first hear the heart sounds, record the pressure reading shown on the gauge. This is the systolic pressure.
- Continue to slowly release air and listen until the clear thumping sound of the pulse becomes strong and then fades away to silence.
- When you last hear the full heart beat, record the pressure reading shown on the gauge. This is the diastolic pressure.
- Repeat the measurements two more times. Record on the pressure readings on the data sheet.
- Calculate the average systolic and diastolic pressure, and record these values on the data sheet.
Method for automated blood pressure cuff measurement
For each subject being tested:
- Place the cuff in the appropriate location—upper arm for brachial measurement, wrist for radial measurement.
- Follow the directions provided by the machine, reminding your subject to remain quiet and still the entire time. Any movement will disrupt the measurement.
- After the allotted time has passed, collect the data from the machine and clear it for use on another test subject.
- Record the pressure readings on the data sheet.
Procedure for measuring blood pressure change from reclining to standing
The point scores on the following tests provide an evaluation of fitness based not only on cardiac muscular development but also on the ability of the cardiovascular system to respond to sudden changes in demand. Caution: Make sure that you do not attempt this exercise if strenuous activity will aggravate a health problem. Work in pairs. Determine the fitness level for one member of the pair and then repeat the process for the other member of the pair. For each subject being tested:
- Recline on a laboratory bench for 5 minutes.
- At the end of this time, measure the systolic and diastolic pressure and record these values on the data sheet.
- Remain reclining for two minutes, then stand and IMMEDIATELY repeat measurements on the same subject (arms down).
- Record these values on the data sheet.
- Calculate the change in systolic pressure from reclining to standing by subtracting the standing measurement from the reclining measurement.
- Assign fitness points based on Table 9 and record in the appropriate space on the data sheet.
| Change (mm Hg) | Fitness Points |
|---|---|
| rise of 8 or more | 3 |
| rise of 2-7 | 2 |
| no rise | 1 |
| fall of 2-5 | 0 |
| fall of 6 or more | -1 |
Part 2. Harvard Step Test
For each subject tested:
- Step up on to a standard gym bench (45cm high) once every two seconds for five minutes (~150 steps). Start with one foot (right or left ) and use that same foot as the starting "step up" foot throughout the exercise.
- Have someone help the subject keep to the required pace. A counter or metronome can be helpful to maintain the rate (120 count on a metronome).
- One minute after finishing the test take the subject's pulse rate for 30 seconds. Have the person refrain from talking and unnecessary movement when heart rates are being counted since any activity can skew the heart rate and influence the results
- Record the 30-sec pulse count on the data sheet.
- Two minutes after finishing the test take the subject's pulse rate for 30 seconds.
- Record the 30-sec pulse count on the data sheet.
- Three minutes after finishing the test take the subject's pulse rate for 30 seconds.
- Record the 30-sec pulse count on the data sheet.
- Use the data sheet to calculate the subject's recovery index value.
Questions for Analysis/Discussion
- How did your cardiac fitness rating compare to your Harvard Step Test cardiac fitness rating?
- Which group of tests do you think is a more accurate measurement of relative cardiac fitness? Why?
- What other methods could be used to test an individual’s cardiac fitness?
- Why do blood pressure and heart rate vary when the subject is reclining versus when they are standing?
- Why do some people feel faint when they go quickly from lying down to standing?
- Explain why athletes in top physical condition must work harder to achieve a maximum heart rate.
- Why is high blood pressure a dire health concern? What other body systems does high blood pressure affect and how?
- Explain why smoking causes a rise in blood pressure.
- How can an individual increase their cardiac fitness? Explain some ways that this could be made possible and how they would increase cardiac fitness.
References
- ↑ Harvard Step Test. Wikipedia, accessed 31 Mar 2012.
- ↑ http://www.topendsports.com/testing/tests/step-harvard.htm Accessed 31 Mar 2012.
- ↑ http://www.brianmac.demon.co.uk/havard.htm. Accessed April 27, 2007.
- ↑ Blood pressure. Wikipedia, accessed 31 Mar 2012.